Atrial fibrillation electrocardiogram: Difference between revisions
No edit summary |
|||
| (8 intermediate revisions by 4 users not shown) | |||
| Line 16: | Line 16: | ||
{{Template:Atrial fibrillation}} | {{Template:Atrial fibrillation}} | ||
{{CMG}} | {{CMG}} {{AE}} {{Anahita}} | ||
==Overview== | ==Overview== | ||
Atrial fibrillation is diagnosed | [[Atrial fibrillation]] is [[diagnosis|diagnosed]] with the [[electrocardiogram]], an investigation performed routinely whenever irregular heartbeat is suspected. Characteristic findings are the absence of [[P wave]]s, with unorganized electrical activity in their place, and irregularity of [[R-R interval]] due to irregular conduction of impulses to the [[ventricle]]s. If paroxysmal [[atrial fibrillation]] is suspected and 12-lead [[The electrocardiogram|ECG]] is normal, usage of a [[Holter monitor|24-hour ambulatory ECG monitor]] is recommended. Typical [[electrocardiogram]] findings in a [[patient]] with [[atrial fibrillation]] are absent [[P wave]]s, [[Irregularly irregular pulse|irregularly irregular]] [[Ventricle (heart)|ventricular]] response rate, and an [[Atrium (heart)|atrial]] rate that ranges from 400 to 700 BPM. A rapid, irregular, sustained, wide-[[QRS complex|QRS-complex]] [[tachycardia]] strongly suggests [[atrial fibrillation]] ([[AF]]) with conduction over an [[accessory pathway]] or [[atrial fibrillation]] ([[AF]]) with underlying [[bundle-branch block]]. | ||
==Electrocardiogram== | ==Electrocardiogram== | ||
*[[The electrocardiogram|ECG]] is essential in [[diagnosis]] of [[atrial fibrillation]]. If paroxysmal [[atrial fibrillation]] is suspected and 12-lead [[The electrocardiogram|ECG]] is normal, usage of a [[Holter monitor|24-hour ambulatory ECG monitor]] is recommended.<ref name="pmid15464683">{{cite journal| author=Tse HF, Newman D, Ellenbogen KA, Buhr T, Markowitz T, Lau CP | display-authors=etal| title=Effects of ventricular rate regularization pacing on quality of life and symptoms in patients with atrial fibrillation (Atrial fibrillation symptoms mediated by pacing to mean rates [AF SYMPTOMS study]). | journal=Am J Cardiol | year= 2004 | volume= 94 | issue= 7 | pages= 938-41 | pmid=15464683 | doi=10.1016/j.amjcard.2004.06.034 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15464683 }} </ref><ref name="pmid34020968">{{cite journal| author=Perry M, Kemmis Betty S, Downes N, Andrews N, Mackenzie S, Guideline Committee| title=Atrial fibrillation: diagnosis and management-summary of NICE guidance. | journal=BMJ | year= 2021 | volume= 373 | issue= | pages= n1150 | pmid=34020968 | doi=10.1136/bmj.n1150 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=34020968 }} </ref><ref name="pmid15155965">{{cite journal| author=Jabaudon D, Sztajzel J, Sievert K, Landis T, Sztajzel R| title=Usefulness of ambulatory 7-day ECG monitoring for the detection of atrial fibrillation and flutter after acute stroke and transient ischemic attack. | journal=Stroke | year= 2004 | volume= 35 | issue= 7 | pages= 1647-51 | pmid=15155965 | doi=10.1161/01.STR.0000131269.69502.d9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15155965 }} </ref> | |||
*[[The electrocardiogram|ECG]] is helpful to identify: | |||
* Rhythm (verify AF) | ** Rhythm (verify [[atrial fibrillation]] ([[AF]])) | ||
* [[LV hypertrophy]] | ** [[LV hypertrophy]] | ||
* [[P-wave]] duration and morphology or | ** [[P-wave]] duration and morphology or fibrillary waves | ||
* Preexcitation | ** Preexcitation | ||
* [[Bundle-branch block]] | ** [[Bundle-branch block]] | ||
* Prior [[MI]] | ** Prior [[MI]] | ||
* Other atrial arrhythmias | ** Other [[Cardiac arrhythmia|atrial arrhythmias]] | ||
* To measure and follow the [[RR]], [[QRS]], and [[QT]] intervals in conjunction with [[antiarrhythmic | ** To measure and follow the [[RR interval|RR]], [[QRS]], and [[QT]] intervals in conjunction with [[antiarrhythmic agent]] | ||
*[[The electrocardiogram|ECG]] also could be used as a predictor of [[atrial fibrillation]]. One of the strongest predictors is the P index, which is an estimation of disorganized [[atrium|atrial]] [[depolarization]].<ref name="pmid19781423">{{cite journal| author=Perez MV, Dewey FE, Marcus R, Ashley EA, Al-Ahmad AA, Wang PJ | display-authors=etal| title=Electrocardiographic predictors of atrial fibrillation. | journal=Am Heart J | year= 2009 | volume= 158 | issue= 4 | pages= 622-8 | pmid=19781423 | doi=10.1016/j.ahj.2009.08.002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19781423 }} </ref> | |||
===Summary of Electrocardiographic Findings=== | ===Summary of Electrocardiographic Findings=== | ||
* Absent [[P wave]]s | * Absent [[P wave]]s | ||
* Irregularly irregular ventricular response rate. | * [[Irregularly irregular pulse|Irregularly irregular]] [[Ventricle (heart)|ventricular]] response rate. Regular [[RR]] intervals are possible in the presence of [[AV block]] or interference due to [[Ventricle (heart)|ventricular]] or junctional [[tachycardia]]. | ||
* An atrial rate that ranges from 400 to 700 BPM. | * An [[Atrium (heart)|atrial]] rate that ranges from 400 to 700 BPM. | ||
* Sometimes lead V1 may look as though there is [[atrial flutter]]. | * Sometimes lead V1 may look as though there is [[atrial flutter]]. This may be because the electrode overlies a portion of the [[Right atrium|RA]] with rhythmic activity. | ||
* The ventricular rate is usually between 100 and 180 BPM. | * Some authors believe that fine [[Electrocardiography|f waves]] (<.5 mm) are associated with [[Coronary heart disease|coronary artery disease]] and that coarse [[Electrocardiography|f waves]] are associated with [[Left atrial enlargement electrocardiogram|LA enlargement]] and [[rheumatic heart disease]]. | ||
* If the atrial rate is greater than 200 BPM, then consider [[WPW]] or an [[accessory pathway]]. | * The [[Ventricle (heart)|ventricular]] rate is usually between 100 and 180 BPM. | ||
* In the presence of AV junctional disease, the ventricular rate may be below 70 bpm. | * If the [[Atrium (heart)|atrial]] rate is greater than 200 BPM, then consider [[Wolff-Parkinson-White syndrome]] ([[WPW]]) or an [[accessory pathway]]. | ||
* A rapid, irregular, sustained, wide-QRS-complex [[tachycardia]] strongly suggests AF with conduction over an [[accessory pathway]] or AF with underlying [[bundle-branch block]]. | * In the presence of [[Atrioventricular dissociation|AV junctional disease]], the [[Ventricle (heart)|ventricular]] rate may be below 70 bpm. | ||
* [[Complete AV block]] is indicated by a slow ventricular rhythm with a regular RR interval. | * A rapid, irregular, sustained, wide-[[QRS complex|QRS-complex]] [[tachycardia]] strongly suggests [[atrial fibrillation]] ([[AF]]) with conduction over an [[accessory pathway]] or [[atrial fibrillation]] ([[AF]]) with underlying [[bundle-branch block]]. | ||
* In patients with electronic [[pacemaker]]s, diagnosis of AF may require temporary inhibition of the pacemaker to expose atrial | * [[Complete AV block]] is indicated by a slow [[Ventricle (heart)|ventricular]] rhythm with a regular [[RR interval]]. | ||
* Differential diagnosis includes an | * In [[patients]] with electronic [[pacemaker]]s, [[diagnosis]] of [[atrial fibrillation]] ([[AF]]) may require temporary inhibition of the [[Artificial pacemaker|pacemaker]] to expose atrial fibrillary activity. | ||
* [[Differential diagnosis]] includes an [[The electrocardiogram|ECG]] artifact such as a [[tremor]]. The oscillations in this case are largest in the [[limb leads]]. | |||
====When are Electrocardiograms Used for Screening?==== | ====When are Electrocardiograms Used for Screening?==== | ||
The SAFE trial found that electronic software, [[primary care physician]]s and the combination of the two had the following sensitivities and specificities:<ref name="pmid17604299">{{cite journal |author=Mant J, Fitzmaurice DA, Hobbs FD, ''et al'' |title=Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial |journal= |volume= |issue= |pages= |year=2007 |pmid=17604299 |doi=10.1136/bmj.39227.551713.AE}}</ref> | The SAFE trial found that electronic software, [[primary care physician]]s and the combination of the two had the following [[Sensitivity (tests)|sensitivities]] and [[specificity (tests)|specificities]]:<ref name="pmid17604299">{{cite journal |author=Mant J, Fitzmaurice DA, Hobbs FD, ''et al'' |title=Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial |journal= |volume= |issue= |pages= |year=2007 |pmid=17604299 |doi=10.1136/bmj.39227.551713.AE}}</ref> | ||
* Interpreted by software: [[sensitivity (tests)|sensitivity]] = 83%, [[specificity (tests)|specificity]] = 99%. | * Interpreted by software: [[sensitivity (tests)|sensitivity]] = 83%, [[specificity (tests)|specificity]] = 99%. | ||
* Interpreted by a primary care physician: sensitivity = 80%, specificity = 92%. | * Interpreted by a [[primary care physician]]: [[sensitivity (tests)|sensitivity]]= 80%, [[specificity (tests)|specificity]] = 92%. | ||
* Interpreted by a primary care physician with software: sensitivity = 92%, specificity = 91%. | * Interpreted by a [[primary care physician]] with software: [[sensitivity (tests)|sensitivity]] = 92%, [[specificity (tests)|specificity]] = 91%. | ||
If paroxysmal AF is suspected but the [[electrocardiogram]] shows a regular rhythm, episodes may be documented with the use of [[Holter monitor]]ing (continuous ECG recording for 24 hours). If the symptoms are very infrequent, longer periods of continuous monitoring may be required. | If paroxysmal [[atrial fibrillation]] ([[AF]]) is suspected but the [[electrocardiogram]] shows a regular [[Pulse|rhythm]], episodes may be documented with the use of [[Holter monitor]]ing (continuous [[The electrocardiogram|ECG]] recording for 24 hours). If the [[symptoms]] are very infrequent, longer periods of continuous monitoring may be required.<ref name="pmid15155965">{{cite journal| author=Jabaudon D, Sztajzel J, Sievert K, Landis T, Sztajzel R| title=Usefulness of ambulatory 7-day ECG monitoring for the detection of atrial fibrillation and flutter after acute stroke and transient ischemic attack. | journal=Stroke | year= 2004 | volume= 35 | issue= 7 | pages= 1647-51 | pmid=15155965 | doi=10.1161/01.STR.0000131269.69502.d9 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15155965 }} </ref> | ||
---- | ---- | ||
Shown below is an | Shown below is an [[The electrocardiogram|ECG]] showing rapid [[ventricle|ventricular]] response (short R-R interval) and no [[P wave]]s suggestive of [[atrial fibrillation]]. | ||
[[Image:AFIB_01_jpg.jpg|center|500px]] | [[Image:AFIB_01_jpg.jpg|center|500px]] | ||
| Line 63: | Line 65: | ||
---- | ---- | ||
Shown below is an | Shown below is an [[The electrocardiogram|ECG]] showing a rapid [[ventricle|ventricular]] rate (short [[RR interval|R-R interval]]) and no [[P wave]]s suggestive of [[atrial fibrillation]]. | ||
[[Image:AFIB_02.jpg|center|500px]] | [[Image:AFIB_02.jpg|center|500px]] | ||
| Line 71: | Line 73: | ||
---- | ---- | ||
Shown below is an | Shown below is an [[The electrocardiogram|ECG]] showing absent [[P wave]]s with a slow [[ventricle|ventricular]] response suggestive of [[atrial fibrillation]]. | ||
[[Image:AFIB_03.jpg|center|500px]] | [[Image:AFIB_03.jpg|center|500px]] | ||
| Line 78: | Line 80: | ||
---- | ---- | ||
Shown below is an | Shown below is an [[The electrocardiogram|ECG]] showing absent [[P waves]] throughout the precordium, suggestive of [[atrial fibrillation]]. | ||
[[Image:AFIB_04.jpg|center|500px]] | [[Image:AFIB_04.jpg|center|500px]] | ||
| Line 85: | Line 87: | ||
---- | ---- | ||
For more [[The electrocardiogram|ECG]] examples of [[atrial fibrillation]] click [[Atrial fibrillation EKG examples|here]]. | |||
==2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation (DO NOT EDIT)<ref name="JanuaryWann2014">{{cite journal|last1=January|first1=C. T.|last2=Wann|first2=L. S.|last3=Alpert|first3=J. S.|last4=Calkins|first4=H.|last5=Cleveland|first5=J. C.|last6=Cigarroa|first6=J. E.|last7=Conti|first7=J. B.|last8=Ellinor|first8=P. T.|last9=Ezekowitz|first9=M. D.|last10=Field|first10=M. E.|last11=Murray|first11=K. T.|last12=Sacco|first12=R. L.|last13=Stevenson|first13=W. G.|last14=Tchou|first14=P. J.|last15=Tracy|first15=C. M.|last16=Yancy|first16=C. W.|title=2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society|journal=Circulation|year=2014|issn=0009-7322|doi=10.1161/CIR.0000000000000041}}</ref>== | |||
* [[AF]] is a supraventricular [[tachyarrhythmia]] with uncoordinated [[atrium|atrial]] activation and consequently ineffective atrial contraction. [[ECG|Electrocardiogram (ECG)]] characteristics include: | |||
:* Irregular [[RR interval|R-R intervals]] (when atrioventricular conduction is present) | |||
:* Absence of distinct repeating [[P wave]]s | |||
:* Irregular atrial activity | |||
===Clinical Evaluation=== | |||
{|class="wikitable" style="width: 80%;" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' [[Electrocardiographic]] documentation is recommended to establish the diagnosis of [[AF]]. ''([[ACC AHA guidelines classification scheme#Level of Evidence|Level of Evidence: C]])'' <nowiki>"</nowiki> | |||
|} | |||
==Sources== | ==Sources== | ||
* [http://circ.ahajournals.org/content/early/2014/03/27/CIR.0000000000000041 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation]<ref name="JanuaryWann2014">{{cite journal|last1=January|first1=C. T.|last2=Wann|first2=L. S.|last3=Alpert|first3=J. S.|last4=Calkins|first4=H.|last5=Cleveland|first5=J. C.|last6=Cigarroa|first6=J. E.|last7=Conti|first7=J. B.|last8=Ellinor|first8=P. T.|last9=Ezekowitz|first9=M. D.|last10=Field|first10=M. E.|last11=Murray|first11=K. T.|last12=Sacco|first12=R. L.|last13=Stevenson|first13=W. G.|last14=Tchou|first14=P. J.|last15=Tracy|first15=C. M.|last16=Yancy|first16=C. W.|title=2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society|journal=Circulation|year=2014|issn=0009-7322|doi=10.1161/CIR.0000000000000041}}</ref> | |||
*[http://www.emedu.org/ecg_lib/index.htm John Vozenilek's (MD) ECG Collection] | *[http://www.emedu.org/ecg_lib/index.htm John Vozenilek's (MD) ECG Collection] | ||
*[http://www.ecgpedia.org ECGpedia] | *[http://www.ecgpedia.org ECGpedia] | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | |||
{{WS}} | |||
[[CME Category::Cardiology]] | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Up-To-Date]] | [[Category:Up-To-Date]] | ||
[[Category:Up-To-Date cardiology]] | [[Category:Up-To-Date cardiology]] | ||
[[Category:Arrhythmia]] | [[Category:Arrhythmia]] | ||
[[Category:Electrophysiology]] | [[Category:Electrophysiology]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Emergency medicine]] | [[Category:Emergency medicine]] | ||
Latest revision as of 06:40, 13 October 2021
| Resident Survival Guide |
| File:Critical Pathways.gif |
Sinus rhythm  |
Atrial fibrillation  |
|
Atrial Fibrillation Microchapters | |
|
Special Groups | |
|---|---|
|
Diagnosis | |
|
Treatment | |
|
Cardioversion | |
|
Anticoagulation | |
|
Surgery | |
|
Case Studies | |
|
Atrial fibrillation electrocardiogram On the Web | |
|
Directions to Hospitals Treating Atrial fibrillation electrocardiogram | |
|
Risk calculators and risk factors for Atrial fibrillation electrocardiogram | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Anahita Deylamsalehi, M.D.[2]
Overview
Atrial fibrillation is diagnosed with the electrocardiogram, an investigation performed routinely whenever irregular heartbeat is suspected. Characteristic findings are the absence of P waves, with unorganized electrical activity in their place, and irregularity of R-R interval due to irregular conduction of impulses to the ventricles. If paroxysmal atrial fibrillation is suspected and 12-lead ECG is normal, usage of a 24-hour ambulatory ECG monitor is recommended. Typical electrocardiogram findings in a patient with atrial fibrillation are absent P waves, irregularly irregular ventricular response rate, and an atrial rate that ranges from 400 to 700 BPM. A rapid, irregular, sustained, wide-QRS-complex tachycardia strongly suggests atrial fibrillation (AF) with conduction over an accessory pathway or atrial fibrillation (AF) with underlying bundle-branch block.
Electrocardiogram
- ECG is essential in diagnosis of atrial fibrillation. If paroxysmal atrial fibrillation is suspected and 12-lead ECG is normal, usage of a 24-hour ambulatory ECG monitor is recommended.[1][2][3]
- ECG is helpful to identify:
- Rhythm (verify atrial fibrillation (AF))
- LV hypertrophy
- P-wave duration and morphology or fibrillary waves
- Preexcitation
- Bundle-branch block
- Prior MI
- Other atrial arrhythmias
- To measure and follow the RR, QRS, and QT intervals in conjunction with antiarrhythmic agent
- ECG also could be used as a predictor of atrial fibrillation. One of the strongest predictors is the P index, which is an estimation of disorganized atrial depolarization.[4]
Summary of Electrocardiographic Findings
- Absent P waves
- Irregularly irregular ventricular response rate. Regular RR intervals are possible in the presence of AV block or interference due to ventricular or junctional tachycardia.
- An atrial rate that ranges from 400 to 700 BPM.
- Sometimes lead V1 may look as though there is atrial flutter. This may be because the electrode overlies a portion of the RA with rhythmic activity.
- Some authors believe that fine f waves (<.5 mm) are associated with coronary artery disease and that coarse f waves are associated with LA enlargement and rheumatic heart disease.
- The ventricular rate is usually between 100 and 180 BPM.
- If the atrial rate is greater than 200 BPM, then consider Wolff-Parkinson-White syndrome (WPW) or an accessory pathway.
- In the presence of AV junctional disease, the ventricular rate may be below 70 bpm.
- A rapid, irregular, sustained, wide-QRS-complex tachycardia strongly suggests atrial fibrillation (AF) with conduction over an accessory pathway or atrial fibrillation (AF) with underlying bundle-branch block.
- Complete AV block is indicated by a slow ventricular rhythm with a regular RR interval.
- In patients with electronic pacemakers, diagnosis of atrial fibrillation (AF) may require temporary inhibition of the pacemaker to expose atrial fibrillary activity.
- Differential diagnosis includes an ECG artifact such as a tremor. The oscillations in this case are largest in the limb leads.
When are Electrocardiograms Used for Screening?
The SAFE trial found that electronic software, primary care physicians and the combination of the two had the following sensitivities and specificities:[5]
- Interpreted by software: sensitivity = 83%, specificity = 99%.
- Interpreted by a primary care physician: sensitivity= 80%, specificity = 92%.
- Interpreted by a primary care physician with software: sensitivity = 92%, specificity = 91%.
If paroxysmal atrial fibrillation (AF) is suspected but the electrocardiogram shows a regular rhythm, episodes may be documented with the use of Holter monitoring (continuous ECG recording for 24 hours). If the symptoms are very infrequent, longer periods of continuous monitoring may be required.[3]
Shown below is an ECG showing rapid ventricular response (short R-R interval) and no P waves suggestive of atrial fibrillation.
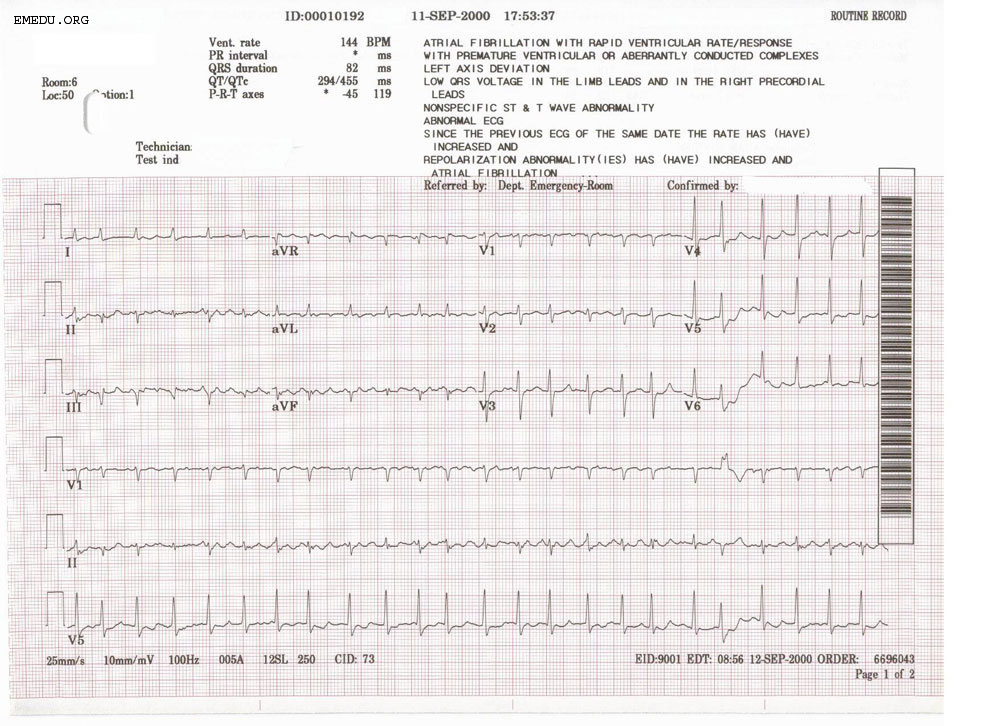
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an ECG showing a rapid ventricular rate (short R-R interval) and no P waves suggestive of atrial fibrillation.
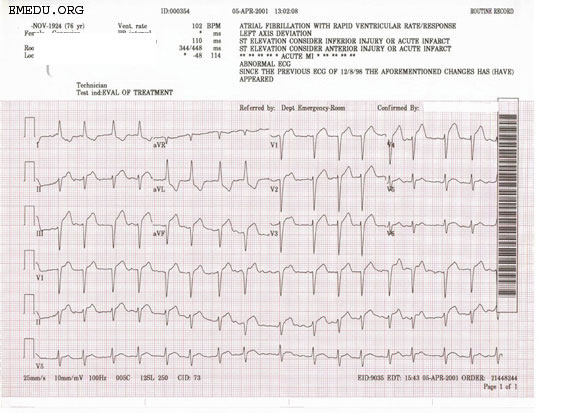
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an ECG showing absent P waves with a slow ventricular response suggestive of atrial fibrillation.
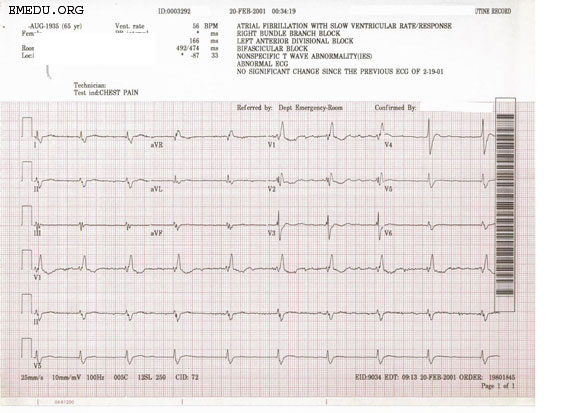
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
Shown below is an ECG showing absent P waves throughout the precordium, suggestive of atrial fibrillation.
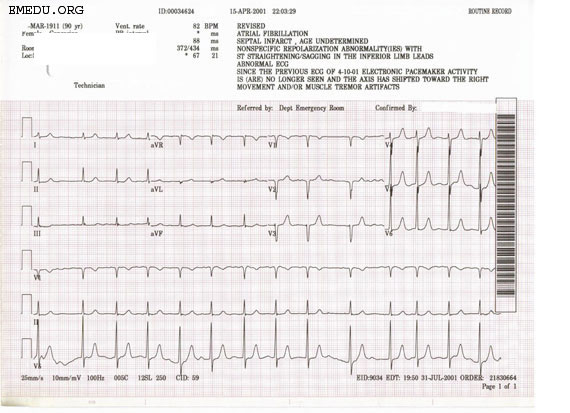
Copyleft image obtained courtesy of ECGpedia, http://en.ecgpedia.org/wiki/Main_Page
For more ECG examples of atrial fibrillation click here.
2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation (DO NOT EDIT)[6]
- AF is a supraventricular tachyarrhythmia with uncoordinated atrial activation and consequently ineffective atrial contraction. Electrocardiogram (ECG) characteristics include:
- Irregular R-R intervals (when atrioventricular conduction is present)
- Absence of distinct repeating P waves
- Irregular atrial activity
Clinical Evaluation
| Class I |
| "1. Electrocardiographic documentation is recommended to establish the diagnosis of AF. (Level of Evidence: C) " |
Sources
References
- ↑ Tse HF, Newman D, Ellenbogen KA, Buhr T, Markowitz T, Lau CP; et al. (2004). "Effects of ventricular rate regularization pacing on quality of life and symptoms in patients with atrial fibrillation (Atrial fibrillation symptoms mediated by pacing to mean rates [AF SYMPTOMS study])". Am J Cardiol. 94 (7): 938–41. doi:10.1016/j.amjcard.2004.06.034. PMID 15464683.
- ↑ Perry M, Kemmis Betty S, Downes N, Andrews N, Mackenzie S, Guideline Committee (2021). "Atrial fibrillation: diagnosis and management-summary of NICE guidance". BMJ. 373: n1150. doi:10.1136/bmj.n1150. PMID 34020968 Check
|pmid=value (help). - ↑ 3.0 3.1 Jabaudon D, Sztajzel J, Sievert K, Landis T, Sztajzel R (2004). "Usefulness of ambulatory 7-day ECG monitoring for the detection of atrial fibrillation and flutter after acute stroke and transient ischemic attack". Stroke. 35 (7): 1647–51. doi:10.1161/01.STR.0000131269.69502.d9. PMID 15155965.
- ↑ Perez MV, Dewey FE, Marcus R, Ashley EA, Al-Ahmad AA, Wang PJ; et al. (2009). "Electrocardiographic predictors of atrial fibrillation". Am Heart J. 158 (4): 622–8. doi:10.1016/j.ahj.2009.08.002. PMID 19781423.
- ↑ Mant J, Fitzmaurice DA, Hobbs FD; et al. (2007). "Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial". doi:10.1136/bmj.39227.551713.AE. PMID 17604299.
- ↑ 6.0 6.1 January, C. T.; Wann, L. S.; Alpert, J. S.; Calkins, H.; Cleveland, J. C.; Cigarroa, J. E.; Conti, J. B.; Ellinor, P. T.; Ezekowitz, M. D.; Field, M. E.; Murray, K. T.; Sacco, R. L.; Stevenson, W. G.; Tchou, P. J.; Tracy, C. M.; Yancy, C. W. (2014). "2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society". Circulation. doi:10.1161/CIR.0000000000000041. ISSN 0009-7322.