Arnold-Chiari malformation: Difference between revisions
| Line 106: | Line 106: | ||
*Impaired [[gag reflex]] | *Impaired [[gag reflex]] | ||
*Impaired [[coordination]] | *Impaired [[coordination]] | ||
===X ray skull=== | ===Imaging Findings=== | ||
====X ray skull==== | |||
May demonstrate associated abnormalities of the skull base. | May demonstrate associated abnormalities of the skull base. | ||
===CT=== | ===CT=== | ||
May demonstrate hydrocephalus, herniated cerebellar tonsils, and a flattened spinal cord. Rarely will CT show a syrinx. | May demonstrate hydrocephalus, herniated cerebellar tonsils, and a flattened spinal cord. Rarely will CT show a syrinx. | ||
Revision as of 19:06, 25 July 2012
| Arnold-Chiari malformation | |
 | |
|---|---|
| An uncollapsed syrinx (before surgery). | |
| ICD-10 | Q07.0 |
| ICD-9 | 741.0 |
| OMIM | 207950 |
| DiseasesDB | 899 |
| MeSH | D001139 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Arnold-Chiari malformation, sometimes referred to as Chiari malformation or ACM, is a congenital anomaly of the brain.
Arnold-Chiari Malformation II occurs in almost all children born with both spina bifida and hydrocephalus, but ACM I is typically seen in children and adults without spina bifida. The scale of severity is rated I - IV, with IV being the most severe. [1] [2] [3]
Classification
The Austrian pathologist Hans Chiari in the late 19th century described seemingly related anomalies of the hindbrain, the so called Chiari malformations I, II and III. Later, other investigators added a fourth (Chiari IV) malformation. The scale of severity is rated I - IV, with IV being the most severe. Types III and IV are very rare.[4]
| Type | Presentation | Other notes |
|---|---|---|
| I | A congenital malformation. Is generally asymptomatic during childhood, but often manifests with headaches and cerebellar symptoms. Herniation of cerebellar tonsils.[5][6] | The most common form. |
| Syndrome of occipitoatlantoaxial hypermobility | An acquired Chiari I Malformation in patients with hereditary disorders of connective tissue.[7] Patients who exhibit extreme joint hypermobility and connective tissue weakness as a result of Ehlers-Danlos syndrome or Marfan Syndrome are susceptible to instabilities of the craniocervical junction and thus acquiring a Chiari Malformation. This type is difficult to diagnose and treat.[8] | |
| II | Usually accompanied by a lumbar myelomeningocele[9] leading to partial or complete paralysis below the spinal defect. As opposed to the less pronounced tonsillar herniation seen with Chiari I, there is a larger cerebellar vermian displacement. Low lying torcular herophili, tectal beaking, and hydrocephalus with consequent clival hypoplasia are classic anatomic associations.[10] The position of the torcular herophili is important for distinction from Dandy-Walker syndrome in which it is classically upturned. This is important because the hypoplastic cerebellum of Dandy-Walker may be difficult to distinguish from a Chiari malformation that has herniated or is ectopic on imaging. Colpocephaly may be seen due to the associated neural tube defect. | |
| III | Causes severe neurological defects. It is associated with an occipital encephalocele.[11] | |
| IV | Characterized by a lack of cerebellar development.[12] |
Other conditions sometimes associated with Chiari Malformation include hydrocephalus,[13] syringomyelia, spinal curvature, tethered spinal cord syndrome, and connective tissue disorders[7] such as Ehlers-Danlos syndrome and Marfan Syndrome.
Pathophysiology
- The most widely accepted pathophysiological mechanism by which Chiari Type 1 Malformations occur is by a reduction or lack of development of the posterior fossa as a result of either congenital or acquired disorders.
- The cerebellar tonsils are elongated and pushed down through the opening of the base of the skull (see foramen magnum), blocking the flow of cerebrospinal fluid (CSF).
- The brainstem, cranial nerves, and the lower portion of the cerebellum may be stretched or compressed.
- Therefore, any of the functions controlled by these areas may be affected. The blockage of CSF flow may also cause a syrinx to form, eventually leading to syringomyelia. Many sufferers turn to the Chiari Institute in Long Island, NY for specialized medical attention and medication.
Causes
Congenital causes are
- craniosynostosis (especially of the lambdoid suture)
- hyperostosis (ex. craniometaphyseal dysplasia
- osteopetrosis
- X-linked vitamin D-resistant rickets
- neurofibromatosis type I
Acquired disorders include space occupying lesions due to one of several potential causes ranging from brain tumors to hematomas.[14]
Historical Perspective
An Austrian pathologist, Hans Chiari, first described these hindbrain malformations in the 1890s. A colleague of Professor Chiari, Dr. Julius Arnold later contributed to the definition of the condition, and students of Dr. Arnold suggested the term "Arnold-Chiari malformation" to henceforth refer to the condition.[15]
Diagnosis
Symptoms
In infants, the most common symptoms are
- stridor
- Swallowing difficulties
In older children
- Upper (and lower as age marches on) limb weakness
- Breathing difficulties may occur
- Patients may experience no symptoms or remain asymptomatic until early adulthood at which point they will often experience severe headaches and neck pain
- Fatigue
- Dizziness
- Vertigo
- Neuropathic pain
- Pain at the point of tethering
- Visual disturbances
- Difficulty swallowing
- Ringing in the ears
- Sleep apnea
- Impaired fine motor skills
- Muscle weakness
- Palpitations
- Excessive clearing of the throat with no obstructions
- Because of the complex combination of symptoms and the lack of experience with ACM1 had by many, even outstanding neurologists and neurosurgeons, many patients are frequently misdiagnosed.
- Some patients may go an entire lifetime without having noticeable symptoms. Or, symptoms can be minimal, then turn severe suddenly due to head trauma which alters the condition of the spine, brain, or cerebellar tonsils and begins to cause more difficulties...
physical Examination
Vitals
Pulse
Rate
Tachycardia may be present.
Eye
- Nystagmus (irregular eye movements) may be present.
- pupillary dilatation
Neurologic
- Impaired gag reflex
- Impaired coordination
Imaging Findings
X ray skull
May demonstrate associated abnormalities of the skull base.
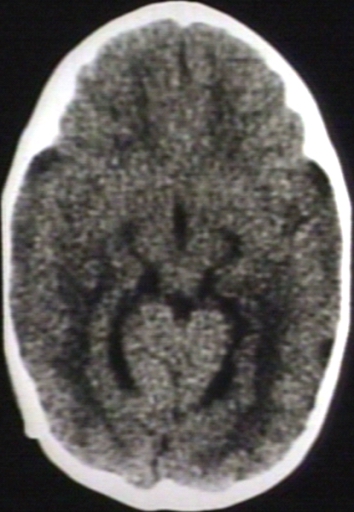
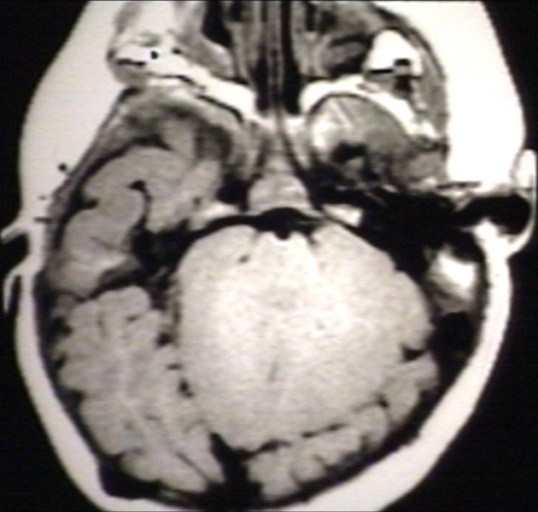
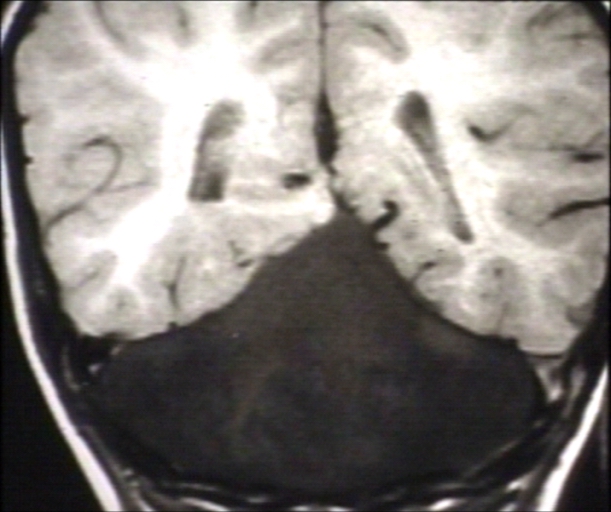
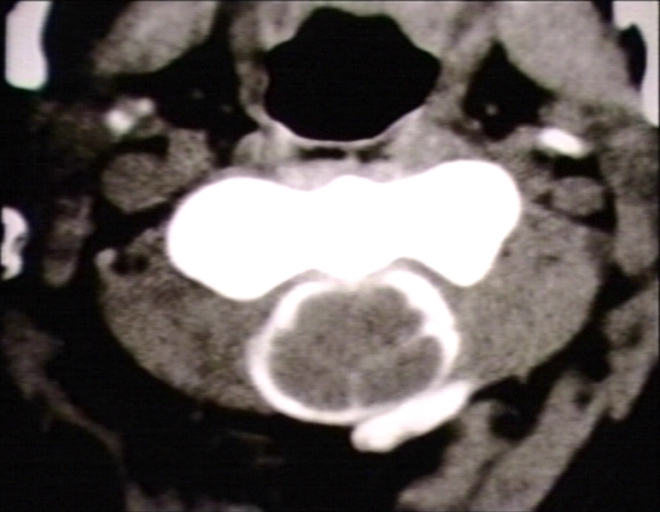
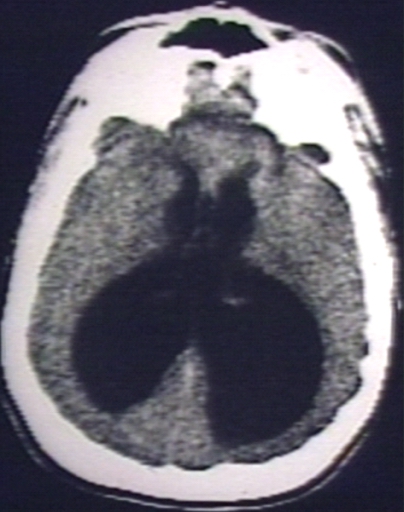
CT
May demonstrate hydrocephalus, herniated cerebellar tonsils, and a flattened spinal cord. Rarely will CT show a syrinx.
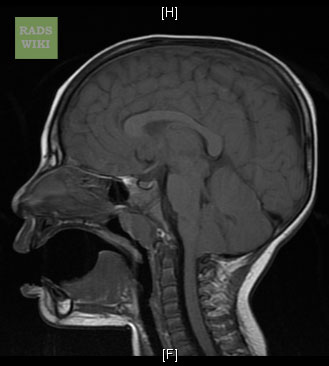
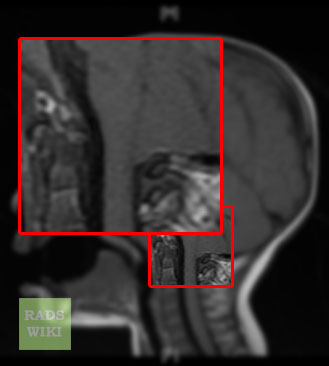
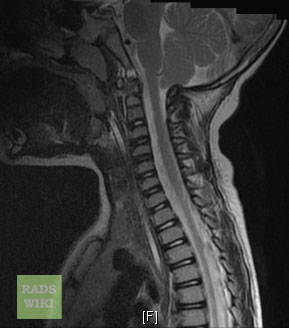
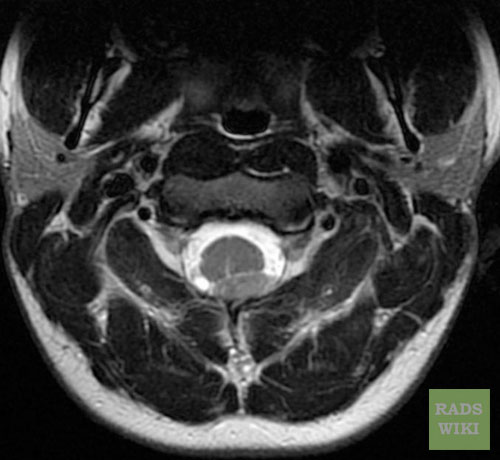
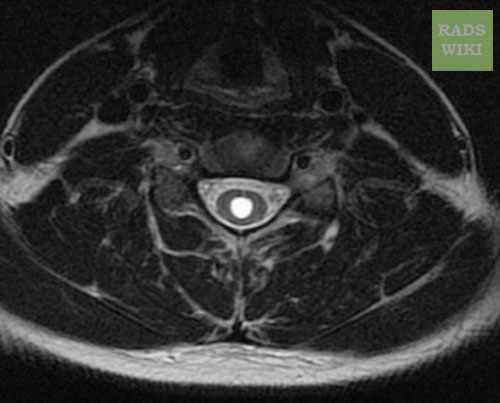
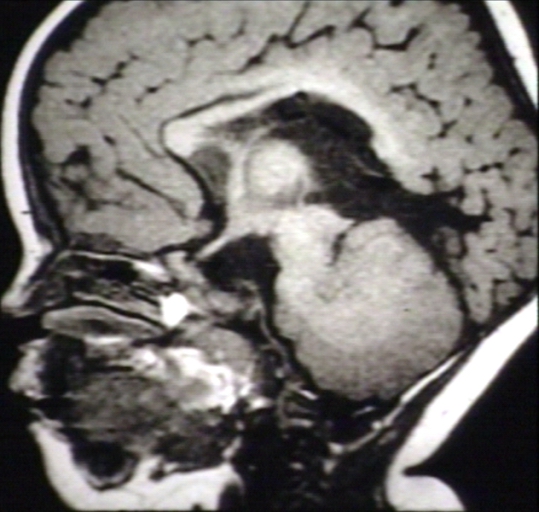
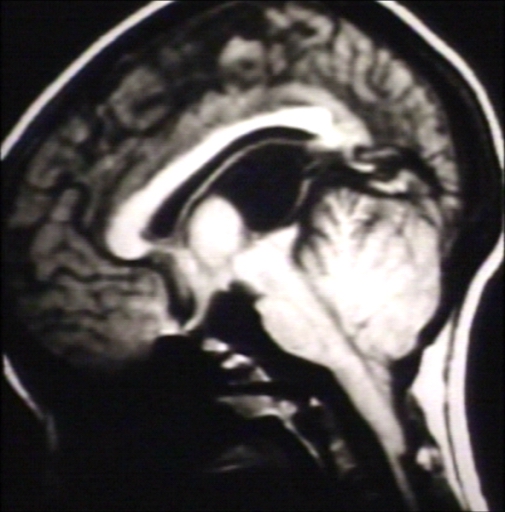
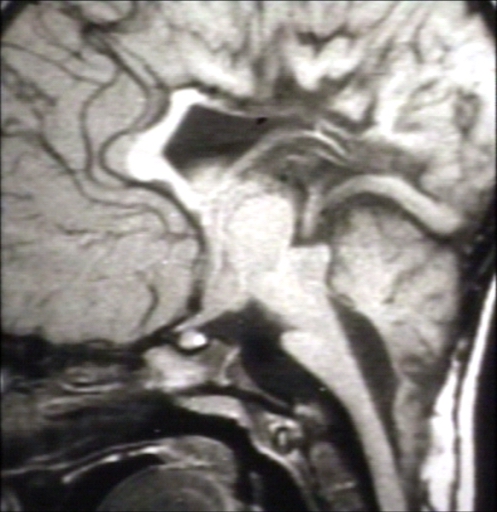
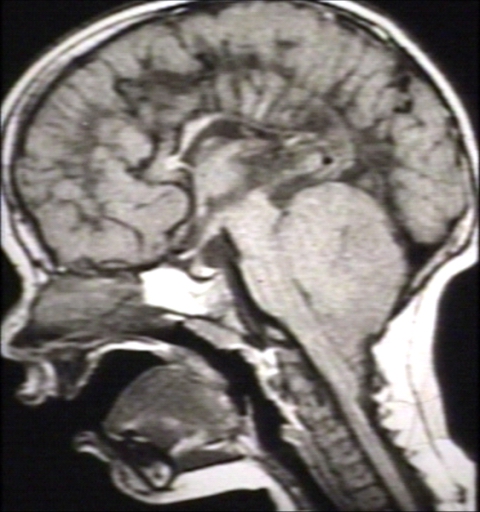
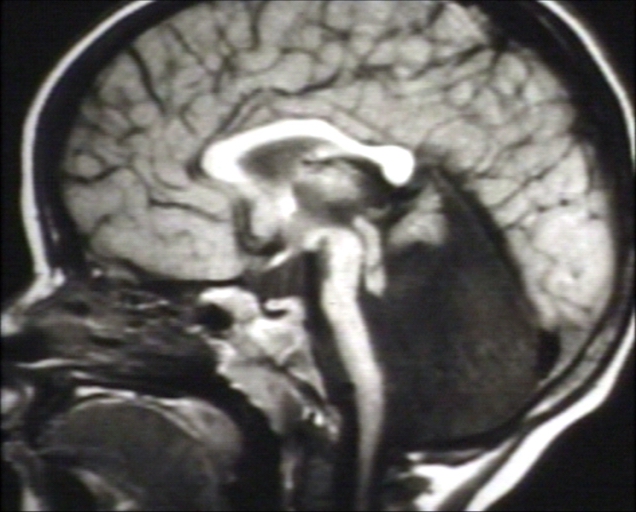
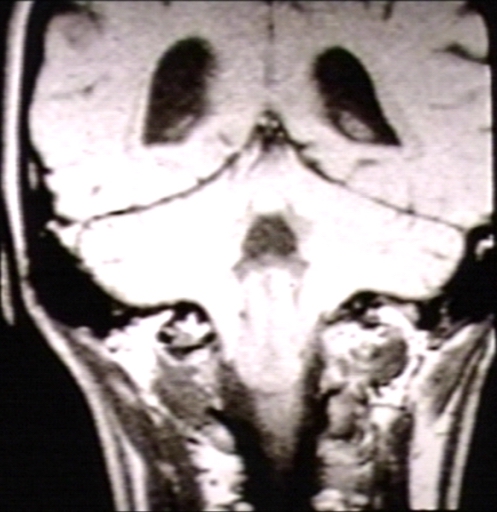
MRI
MRI is the imaging modality of choice to evaluate for a Chiari I malformation. MRI findings:
- Cerebellar tonsillar herniation
- Wedge shaped tonsils
- Syringohydromyelia
- Small posterior fossa
- Obstructive hydrocephalus
- Brainstem anomalies
- Tonsillar displacement is measured from the basion-opisthion line on a sigittal image.
- Herniation is usually at least 5mm, though patients with 3-5mm herniation may also have the malformation.
- MRI CSF flow studies may prove to be helpful and are currently under investigation.
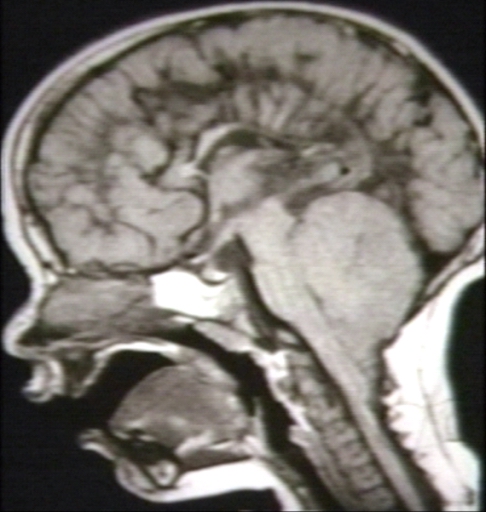
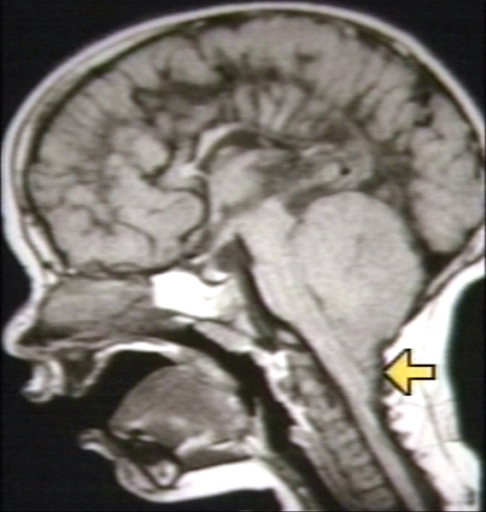
Patient #1
Images shown below are courtesy of RadsWiki and copylefted
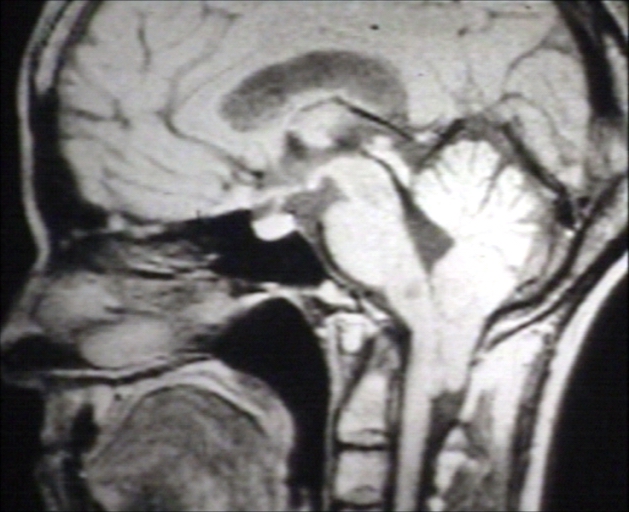
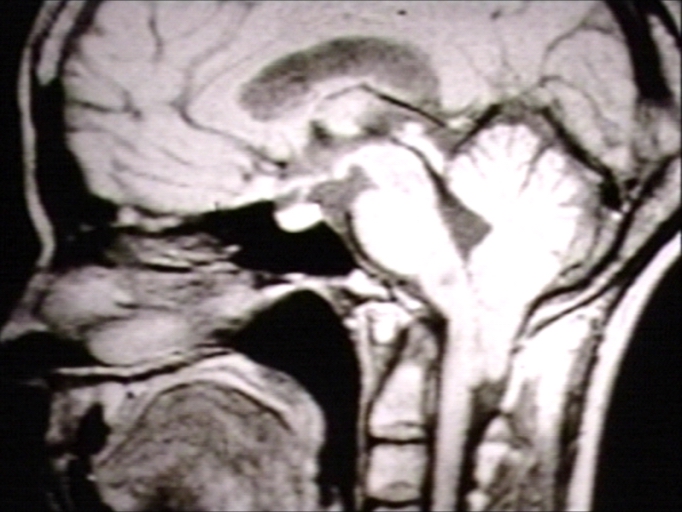
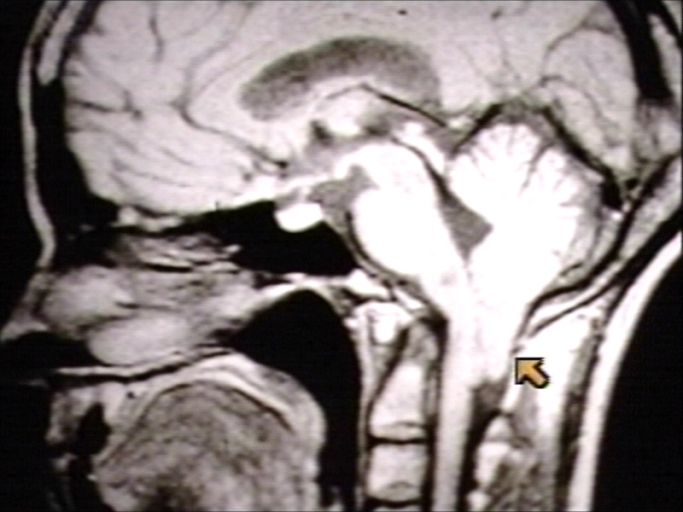
Patient #2
Images shown below are courtesy of RadsWiki and copylefted
Other Radiologic Findings
-
Brain: Arnold Chiari I; T1 (MRI)
-
Brain CT: Arnold Chiari I with Intrathecal Contrast; WC
-
Brain: Arnold Chiari I, with Hydromyelia of Cervical Spinal Cord; T1 (MRI)
-
Skull: Arnold Chiari II, Skull with Luckenschadel (Plain Film)
-
Brain: Arnold Chiari II, Hydrocephalus (CT)
-
Brain: Arnold Chiari II, 6 months Post-Shunt (CT)
-
Brain: Arnold Chiari II, with Towering of The Cerebellum and Wide Tentorial Incisure; T1 (MRI)
-
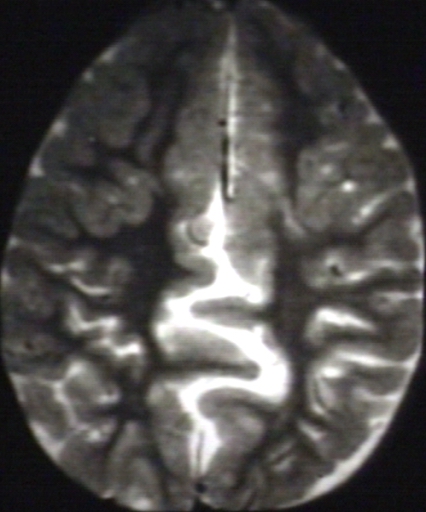
Brain: Arnold Chiari II, with Fenestrated Falx Cerebri and Interdigitating Gyri; T2 (MRI)
-
Brain: Arnold Chiari II, with Tectal Beaking and Large Massa Intermedia and Stenogyria; T1 (MRI)
-
Brain: Arnold Chiari Type II with Medullary Spur and Kink (MRI)
-
Brain: Arnold Chiari II, with Hypoplastic Corpus Callosum; T1 (MRI)
-
Brain: Arnold Chiari II, with Cerebellar Hemispheres that Creep Anteriorly Around the Brain Stem; T1 (MRI)
-
BRAIN: ARNOLD CHIARI II (MRI)
-
BRAIN: ARNOLD CHIARI II WITH ELONGATED FOURTH VENTRICLES AND STENOGYRIA; T1 (MRI)
-
BRAIN: ARNOLD CHIARI II WITH HYPOPLASTIC CORPUS CALLOSUM AND STENOGYRIA; T1 (MRI)
-
BRAIN: ARNOLD CHIARI II WITH REPAIRED MYELOMENINGOCELE AND TETHERED SPINAL CORD; T1 (MRI)
-
BRAIN: ARNOLD CHIARI TYPE IV; T1 (MRI)
-
BRAIN: ARNOLD CHIARI TYPE IV; T1 (MRI)
-
BRAIN: ARNOLD CHIARI MALFORMATION II; 1/2 PCMC (MRI)
-
BRAIN: ARNOLD CHIARI MALFORMATION II, HERNIATED CEREBELLAR TONSIL; 1/2 PCMC - ARROW (MRI)
-
SPINAL CORD: ARNOLD CHIARI MALFORMATION II; 2/2 PCMC (MRI)
-
SPINAL CORD: ARNOLD CHIARI MALFORMATION II; 2/2 PCMC - ARROW (MRI)
-
BRAIN: ARNOLD CHIARI MALFORMATION; 1/3 T2 (MRI)
-
BRAIN: ARNOLD CHIARI MALFORMATION; 1/3 - ARROW T2 (MRI)
-
BRAIN: ARNOLD CHIARI MALFORMATION; 2/3 T2 (MRI)
-
SPINAL CORD: ARNOLD CHIARI MALFORMATION; 3/3 (CT)
-
BRAIN: ARNOLD CHIARI MALFORMATION (CT)
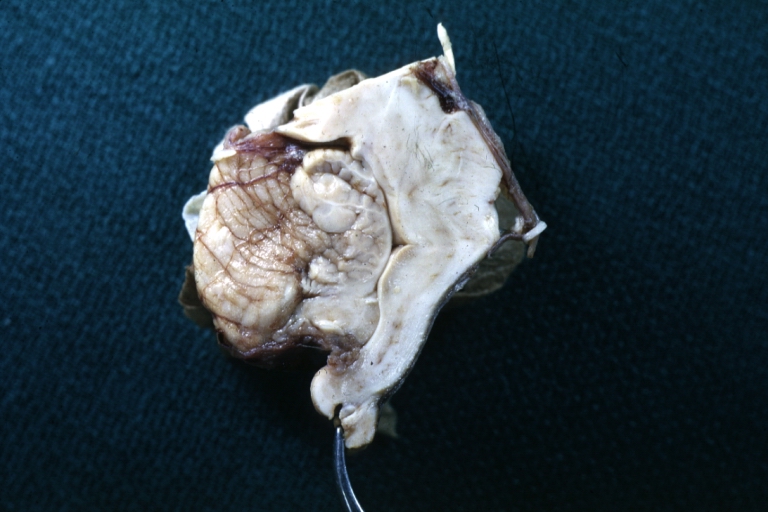
Pathological Findings
-
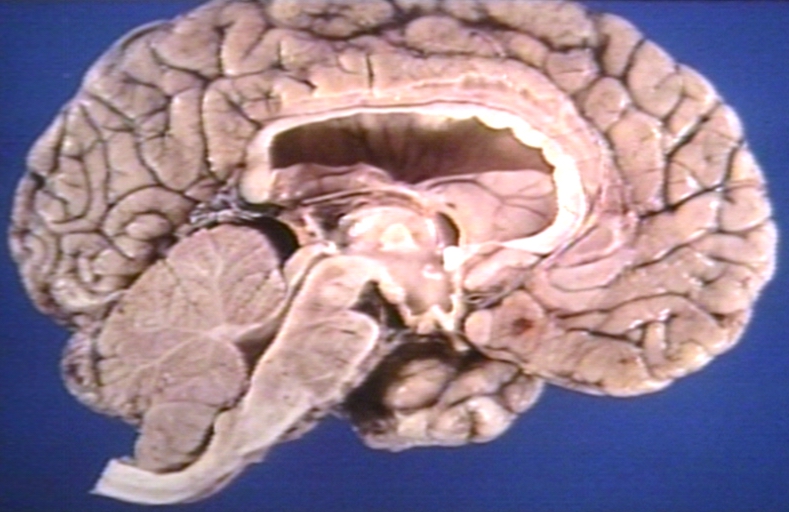
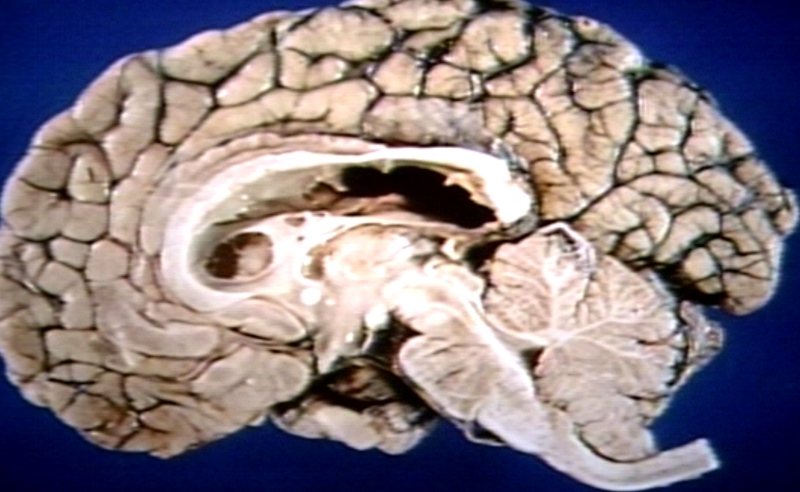
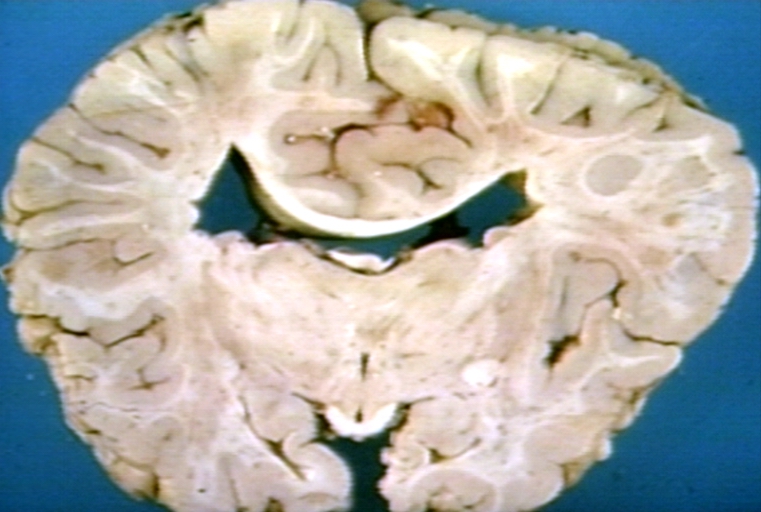
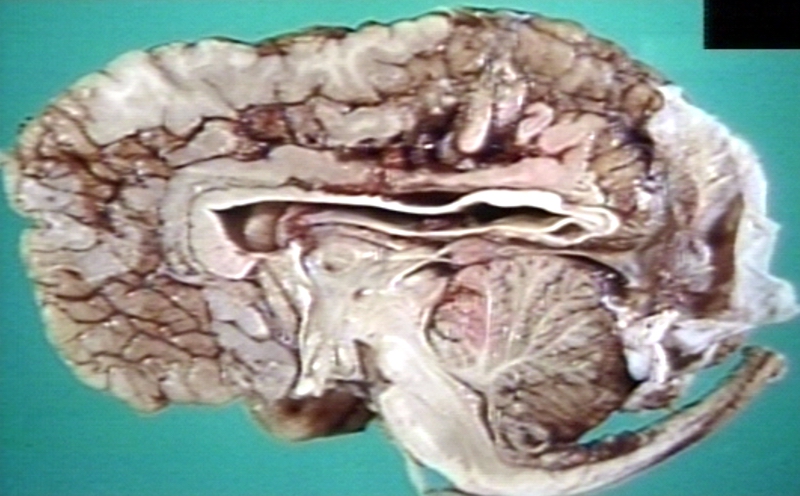
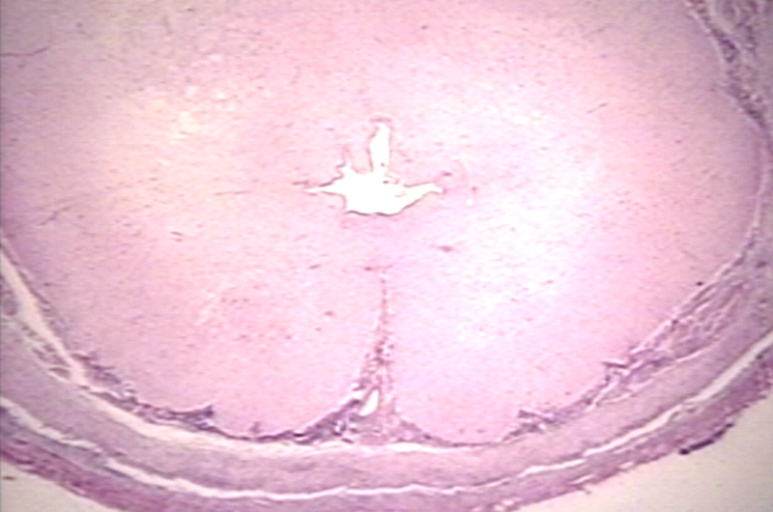
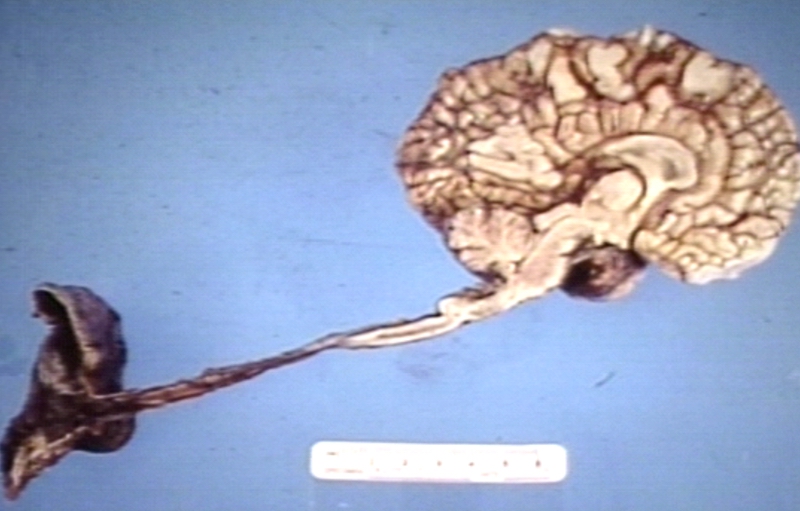
Brain: Arnold-Chiari Malformation: Gross fixed tissue sagittal section brain stem
-
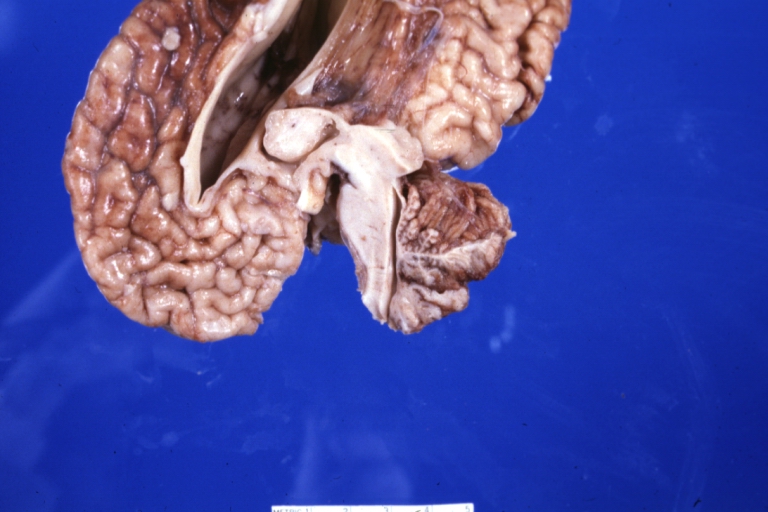
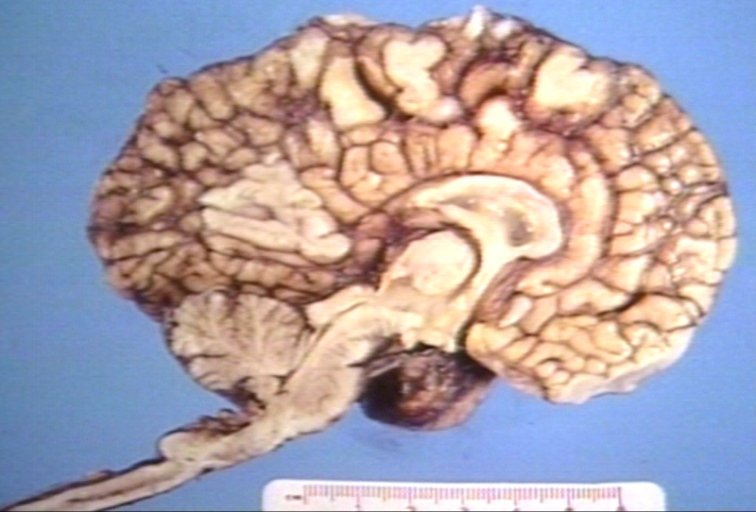
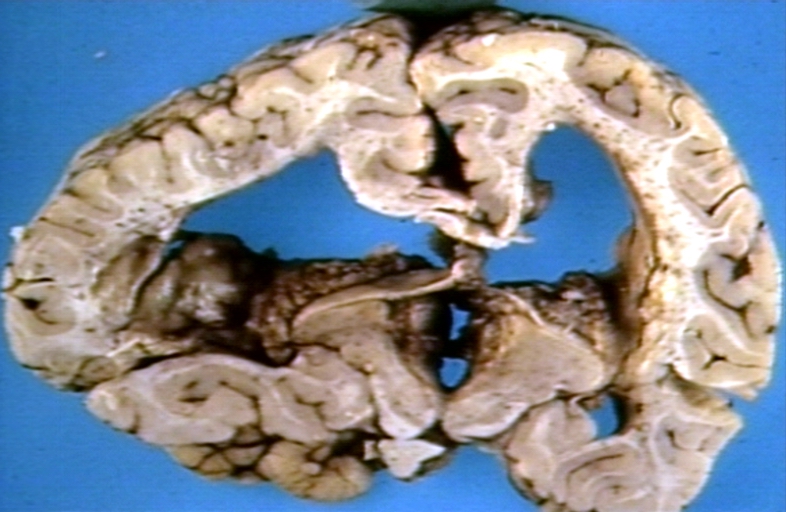
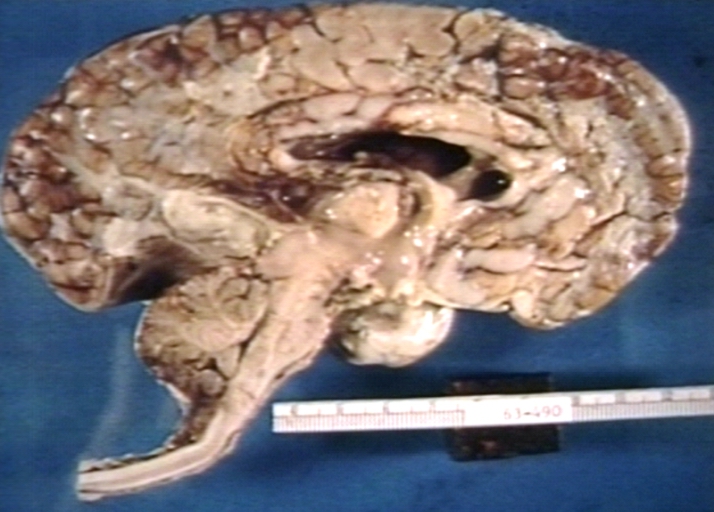
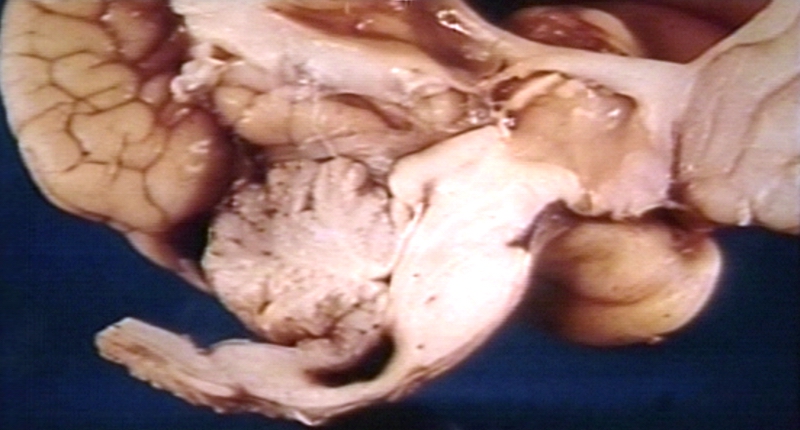
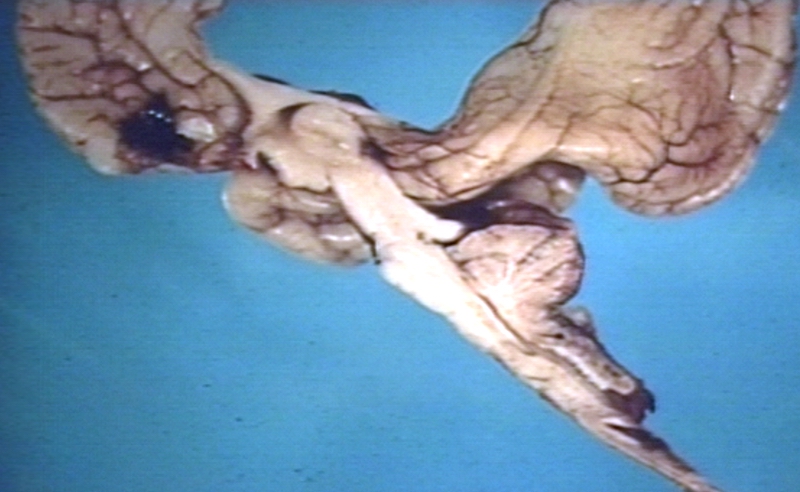
Brain: Arnold Chiari Malformation: Gross fixed tissue sagittal section cerebrum brainstem and cerebellum
-
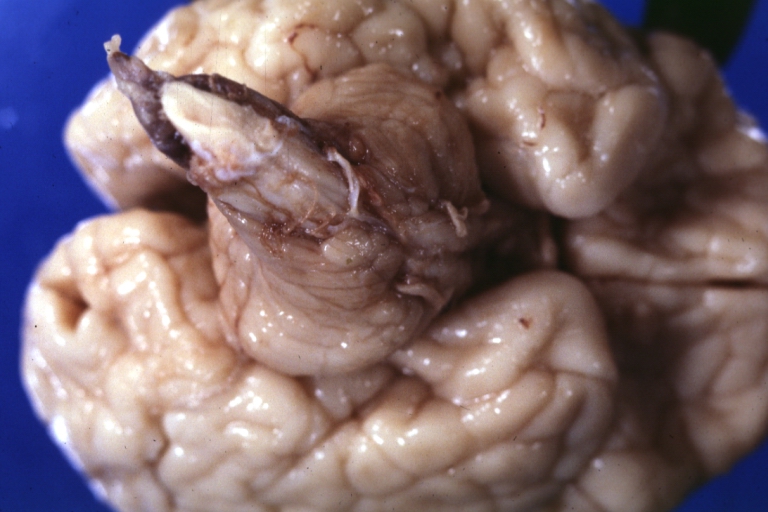
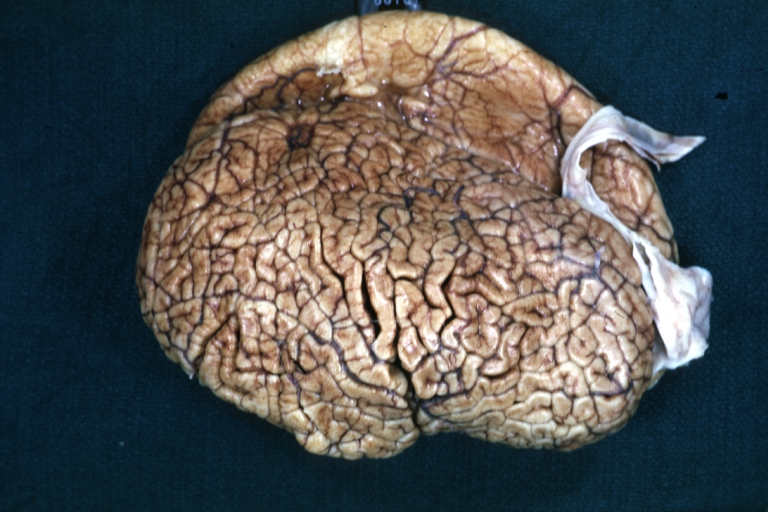
Brain: Arnold Chiari Malformation And Polygyria: Gross fix tissue external view
-
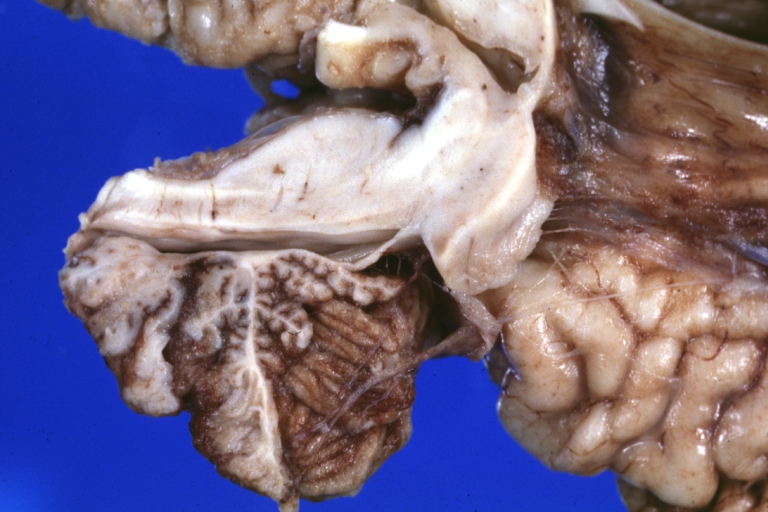
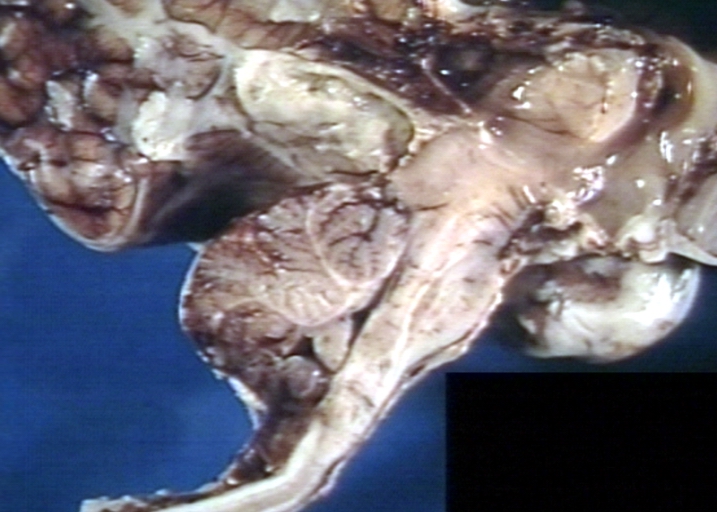
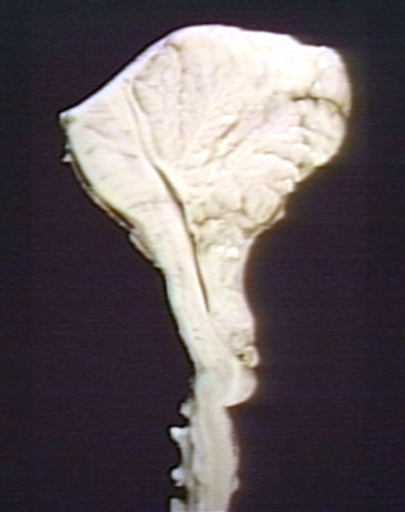
Brain: Arnold Chiari Malformation: Gross fixed tissue sagittal section brainstem close-up
-
Brain: Arnold Chiari Malformation: Gross fixed tissue brain stem sagittal section close-up
-
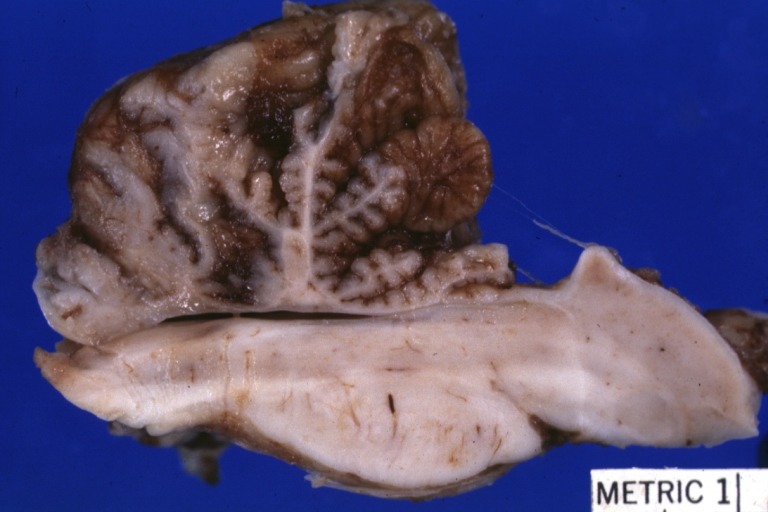
Brain: Arnold Chiari Malformation: Gross fixed tissue sagittal section brain stem and cerebellum
-
Brain: Arnold Chiari Malformation: Gross fixed tissue sagittal section brain stem cerebellum and spinal column
-
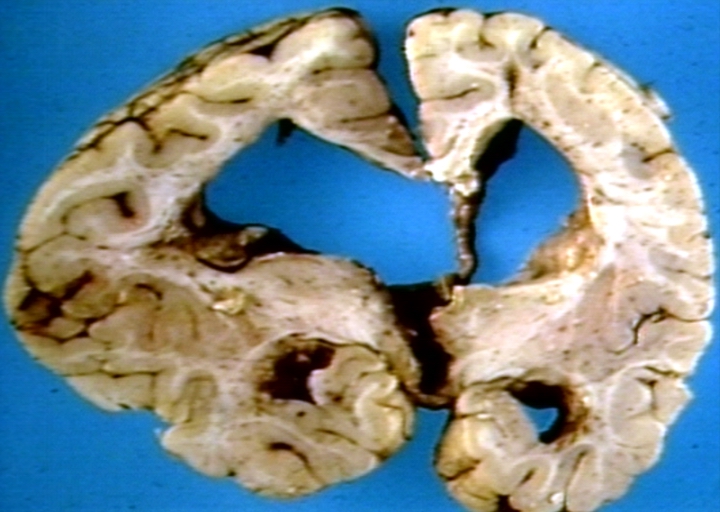
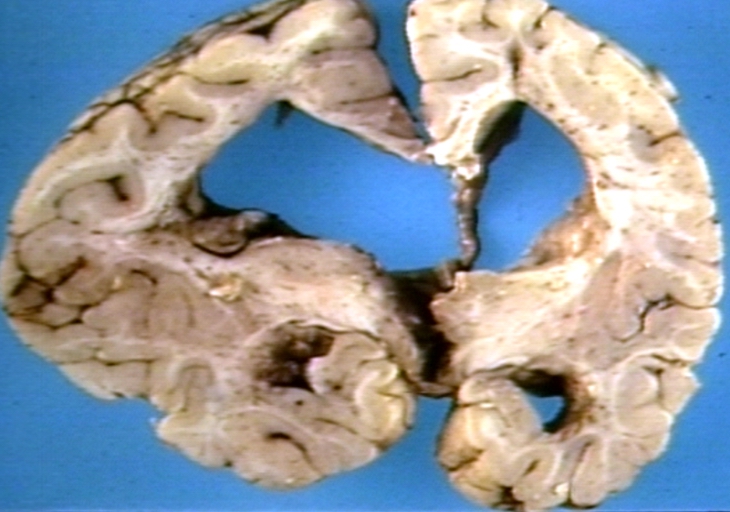
Brain: Hydrocephalus Secondary To Arnold Chiari Malformation: Gross fixed tissue three coronal sections cerebral hemispheres
-
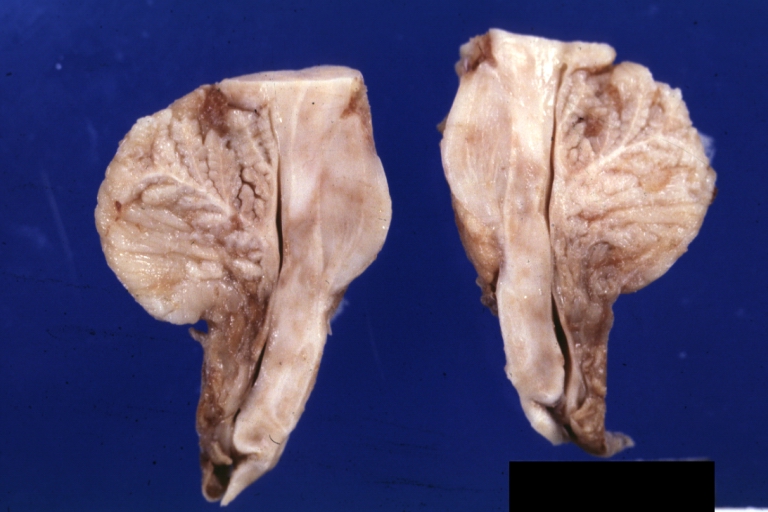
Brain: Arnold Chiari Malformation: Gross fixed tissue cerebellum and brainstem
-
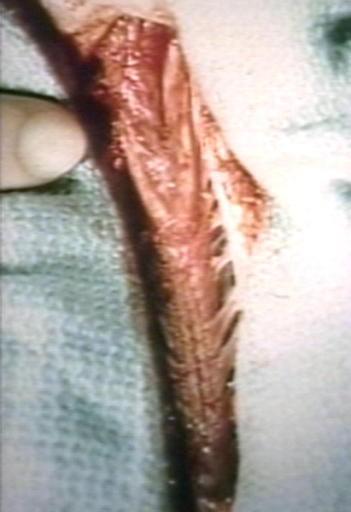
Spinal cord: Malformation Vertebral Bodies: Gross natural color sagittal section spinal column with malformation in region C7 T1 associated with Arnold Chiari malformation
-
Brain: Arnold Chiari Malformation; with Hydrocephalus, Type I
-
Brain: Arnold Chiari Malformation; Type II
-
Brain: Arnold Chiari Type II with Meningomyelocele
-
Brain: Arnold Chiari Malformation; Mid Sagittal
-
Brain: Arnold Chiari Malformation with Myelocele
-
Brain: Arnold Chiari Malformation with Hydrocephalus
-
Brain: Arnold Chiari Malformation with Hydrocephalus
-
Brain: Arnold Chiari Malformation
-
Brain: Arnold Chiari Malformation
-
Brain: Arnold Chiari Malformation
-
Brain: Arnold Chiari Malformation, a close up view
-
Brain: Arnold Chiari Malformation; Tonsilar Herniation of Cerebellum Compressing Medulla
-
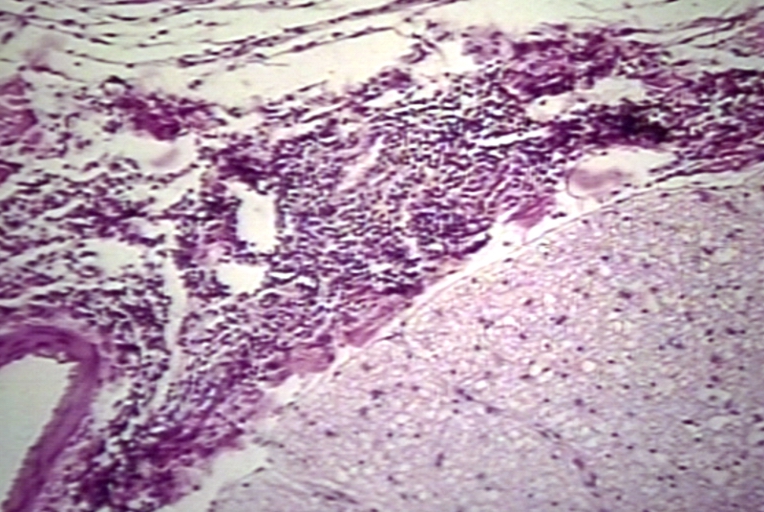
Brain: Arnold Chiari Malformation; Meningomyelocele, Type II, Meningitis
-
Brain: Arnold Chiari Malformation, Type II; Meningomyelocele, Meningitis, Close-up of Previous one
-
Brain: Arnold Chiari Malformation, Intramedullary Hemorrhage
-
Brain: Arnold Chiari Malformation, Type II
-
Spinal Cord: Arnold Chiari Malformation; Type II, Meningomyelitis
-
Spinal Cord: Arnold Chiari Malformation; Type II, Meningomyelitis
-
Brain: Arnold Chiari Malformation
-
Brain: Arnold Chiari Malformation; Note Z-Shaped Kink in Cervical Spinal Cord
-
Brain: Arnold Chiari Malformation with Hydrocephalus
-
Skin: Myelomeningocele with Hydrocephalus; Arnold Chiari; Note Underdevelopment of Legs
-
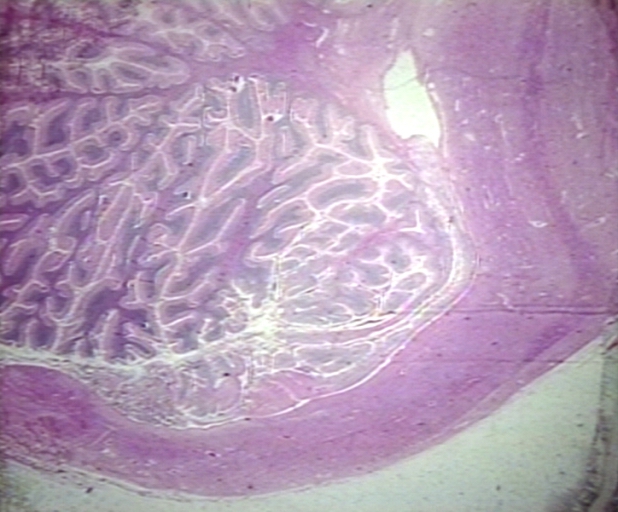
Brain: Cerebellum Arnold Chiari: Gross fixed tissue flattened cerebellum
-
Brain: Polymicrogyria: Gross fixed brain lateral view of left cerebral hemisphere case of Arnold Chiari cerebellum
Treatment
Surgery
Once these "onset of symptoms" occurs, the most frequent treatment is decompression surgery, in which a neurosurgeon seeks to open the base of the skull and through various methods unrestrict CSF flow to the spine.
This treatment is under observation and review. Decompression is a very taxing surgical procedure and is now, in some circles, disdained in lieu of tethered cord detachment at the base of the spine. Some neurological surgeons find that detethering the spinal cord relieves the compression of the brain against the skull opening (foramen magnum) obviating the need for decompression surgery and associated trauma. It should be noted that the alternative spinal surgery is not without risk.
References
- ↑ Barkovich AJ, Wippold FJ, Sherman JL, Citrin CM. Significance of cerebellar tonsillar position on MR. AJNR Am J Neuroradiol. 1986 Sep-Oct;7(5):795-9.
- ↑ Haughton VM, Korosec FR, Medow JE, Dolar MT, Iskandar BJ. Peak systolic and diastolic CSF velocity in the foramen magnum in adult patients with Chiari I malformations and in normal control participants. AJNR Am J Neuroradiol. 2003 Feb;24(2):169-76.
- ↑ Elster A, Chen M. Chiari I malformations: clinical and radiologic reappraisal. Radiology. 1992; 183:347-353.
- ↑ "Arnold Chiari Malformation".
- ↑ Kojima A, Mayanagi K, Okui S (2009). "Progression of pre-existing Chiari type I malformation secondary to cerebellar hemorrhage: case report". Neurol. Med. Chir. (Tokyo). 49 (2): 90–2. doi:10.2176/nmc.49.90. PMID 19246872. Unknown parameter
|month=ignored (help)[dead link] - ↑ O'Shaughnessy BA, Bendok BR, Parkinson RJ; et al. (2006). "Acquired Chiari malformation Type I associated with a supratentorial arteriovenous malformation. Case report and review of the literature". J. Neurosurg. 104 (1 Suppl): 28–32. doi:10.3171/ped.2006.104.1.28. PMID 16509477. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 Milhorat TH, Bolognese PA, Nishikawa M, McDonnell NB, Francomano CA (2007). "Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and chiari malformation type I in patients with hereditary disorders of connective tissue". Journal of Neurosurgery: Spine. 7 (6): 601–9. doi:10.3171/SPI-07/12/601. PMID 18074684. Unknown parameter
|month=ignored (help) - ↑ "Dr. Bland Discusses Chiari & EDS 4(10)". Conquerchiari.org. 2006-11-20. Retrieved 2011-11-04.
- ↑ "Neuroradiology - Chiari malformation (I-IV)".
- ↑ "Cleveland Clinic Children's Hospital Pediatric Radiology Image Gallery". Cleveland Clinic. 2010. Archived from the original on 27 June 2010. Retrieved June 14, 2010.
- ↑ Arnold-Chiari+Malformation at the US National Library of Medicine Medical Subject Headings (MeSH)
- ↑ "Chiari Malformations - Department of Neurological Surgery".
- ↑ "Neuropathology For Medical Students".
- ↑ Loukas M, Shayota BJ, Oelhafen K, Miller JH, Chern JJ, Tubbs RS, Oakes WJ (2011). "Associated disorders of Chiari Type I malformations: a review". Neurosurg Focus. 31 (3): E3. doi:10.3171/2011.6.FOCUS11112. PMID 21882908.
- ↑ Template:WhoNamedIt
Template:Congenital malformations and deformations of nervous system ca:Malformació d'Arnold-Chiari de:Chiari-Malformation it:Sindrome di Arnold-Chiari
- Pages using duplicate arguments in template calls
- Pages with citations using unsupported parameters
- CS1 maint: Multiple names: authors list
- All articles with dead external links
- Articles with dead external links from May 2009
- Articles with invalid date parameter in template
- CS1 maint: Explicit use of et al.
- Pages with broken file links
- Overview complete
- Neurology
- Needs patient information
- Disease