Aortic coarctation
For patient information click here'
|
Aortic coarctation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Aortic coarctation On the Web |
|
American Roentgen Ray Society Images of Aortic coarctation |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
History
Epidemiology and demographics
Classification
Anatomy
Pathophysiology
Natural History
Genetics
Complications
Associated conditions
Diagnosis
Symptoms | Physical examination | Electrocardiogram
With severe coarctation, left ventricular hypertrophy LVH may be present.
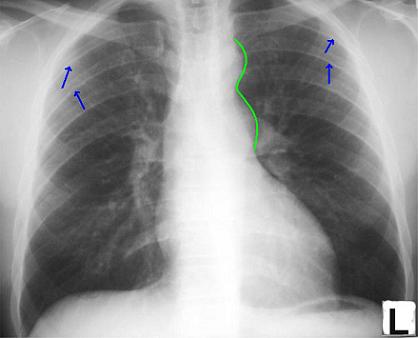
Chest X Ray
Irregularities or notching of the inferior margins of the posterior ribs results from collateral flow through dilated and pulsatile intercostal arteries. These collaterals appear after 6 years of age if the coarctation is significant.
Post-stenotic dilation of the aorta results in a classic 'reverse 3 sign' on x-ray. The characteristic bulging of the sign is caused by dilatation of the aorta due to an indrawing of the aortic wall at the site of cervical rib obstruction, with consequent post-stenotic dilation. This physiology results in the reversed '3' image for which the sign is named.[1][2][3]
Chest X-ray below showing 3 sign and arrows pointing to notching of ribs.
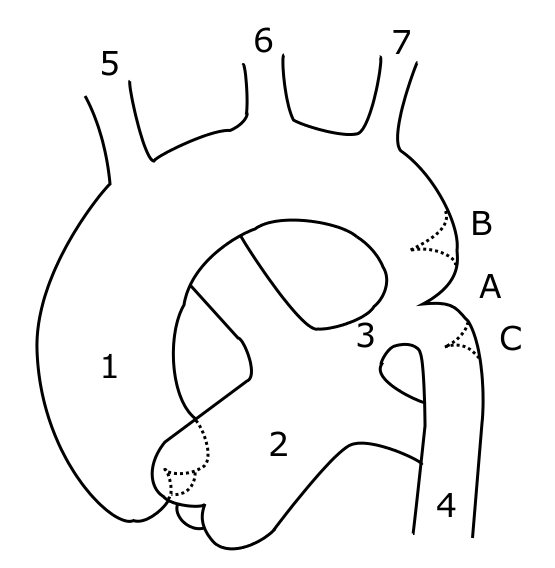
Echocardiography
- Useful in determining associated abnormalities.
- Weyman et al were able to visualize this area and make the diagnosis on 2D echo in 16/18 patients.
- Confirmation by cardiac catheterization is unnecessary. Only done when the diagnosis is unclear, which is rare. It is mandatory in the infant to determine preoperative anatomy.
<googlevideo>-1958798054061108175&hl=en</googlevideo>
<googlevideo>-5952201527214554387&hl=en</googlevideo>
Angiography
<youtube v=yvwCL3D8MFM />
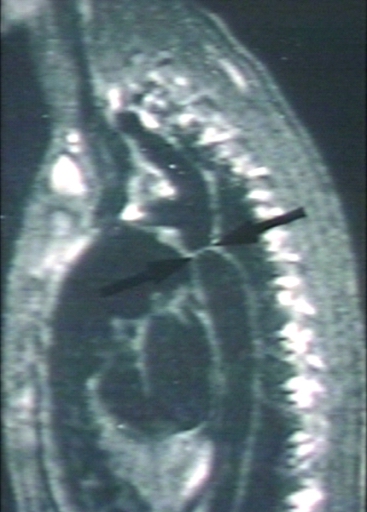
MRI
Magnetic resonance imaging (MRI) can define the location and severity of a coarctation. MRI can also detect associated cardiac abnormalities and is used for serial follow-up after surgical repair or balloon angioplasty. MR angiography has almost completely replaced invasive catheter based techniques for evaluating re coarctation. In adults with untreated coarctation blood often reaches the lower body through collaterals, eg. internal thoracic arteries via. the subclavian arteries. Those can be seen on MR or angiography.
-
[Courtesy of RadsWiki and copylefted]
-
[Courtesy of RadsWiki and copylefted]
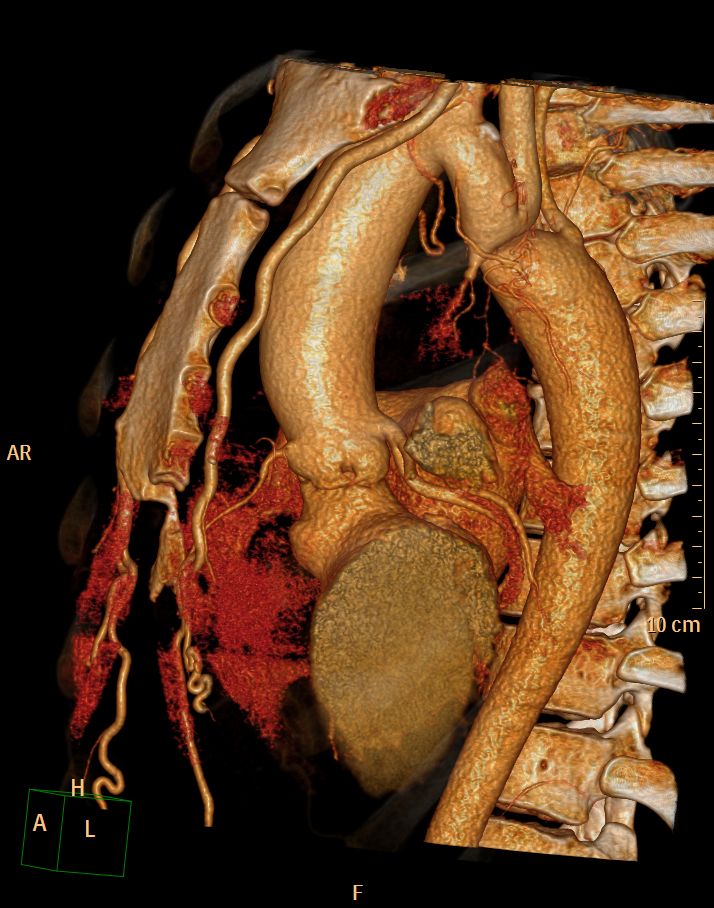
CT
CT images shown below are courtesy of Cafer Zorkun and copylefted
Therapy
Therapy is conservative if the patient is asymptomatic. If symptoms or hypertension are present, treatment for coarctation may be surgical or catheter based. The treatment choice depends on the patients age, the location of the coarctation and other associated anomalies. Recoartctaion after previous surgery is treated percutaneously with either balloon dilation and/or stenting.
References
- ↑ Sabatine, Marc (February 15, 2000). Pocket Medicine. Lippincott Williams & Wilkins. pp. 256 pages. ISBN 0781716497.
- ↑ Blecha, Matthew J. (August 30, 2005). "General Surgery ABSITE and Board Review (Pearls of Wisdom)". McGraw-Hill. ISBN 978-0071464314.
- ↑ Brady Pregerson (October 1, 2006). "Quick Essentials: Emergency Medicine, 2nd Edition". ED Insight Books. ISBN 0976155273.
External links
- A case of coarctation of the aorta was published in the New England Journal of Medicine in 2007 showing chest X-Rays and MRT Images.[1]
- Aortic Coarctation information from Seattle Children's Hospital Heart Center
- Overview and diagram at childrenscentralcal.org
- Diagram at kumc.edu
- Overview and diagram at umich.edu
- [3]
Template:Link FA de:Aortenisthmusstenose it:Coartazione dell'aorta no:Koarktasjon av aorta nn:Koarktasjon sr:Коарктација аорте uk:Коарктація аорти
- ↑ Quiros-Lopez R, Garcia-Alegria J (2007). "A medical mystery -- high blood pressure". N Engl J Med. 356 (25): 2630. PMID 17582073.

![[Courtesy of RadsWiki and copylefted]](/images/7/72/Coarctation-of-the-aorta-MRI-003.jpg)
![[Courtesy of RadsWiki and copylefted]](/images/c/c6/Coarctation-of-the-aorta-MRI-002.jpg)