Amoebiasis laboratory tests: Difference between revisions
No edit summary |
Rim Halaby (talk | contribs) No edit summary |
||
| (4 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Amoebiasis}} {{CMG}}; {{JH}} | {{Amoebiasis}} {{CMG}}; {{AE}} {{JH}} | ||
==Overview== | ==Overview== | ||
==Laboratory Findings== | ==Laboratory Findings== | ||
Asymptomatic human infections are usually diagnosed by finding cysts shed with the stool. Various flotation or sedimentation procedures have been developed to recover the cysts from fecal matter and stains help to visualize the isolated cysts for microscopic examination. Since cysts are not shed constantly, a minimum of 3 stools should be examined. In symptomatic infections, the motile form (the trophozoite) can often be seen in fresh feces. Serological tests exist and most individuals (whether with symptoms or not) will test positive for the presence of antibodies. The levels of antibody are much higher in individuals with liver abscesses. Serology only becomes positive about two weeks after infection. More recent developments include a kit that detects the presence of ameba proteins in the feces and another that detects ameba DNA in feces. These tests are not in widespread use due to their expense. | Asymptomatic human infections are usually diagnosed by finding cysts shed with the stool. Various flotation or sedimentation procedures have been developed to recover the cysts from fecal matter and stains help to visualize the isolated cysts for microscopic examination. Since cysts are not shed constantly, a minimum of 3 stools should be examined. In symptomatic infections, the motile form (the trophozoite) can often be seen in fresh feces. Serological tests exist and most individuals (whether with symptoms or not) will test positive for the presence of antibodies. The levels of antibody are much higher in individuals with liver abscesses. Serology only becomes positive about two weeks after infection. More recent developments include a kit that detects the presence of ameba proteins in the feces and another that detects ameba DNA in feces. These tests are not in widespread use due to their expense. | ||
Microscopy is still by far the most widespread method of diagnosis around the world. However it is not as sensitive or accurate in diagnosis as the other tests available. It is important to distinguish the ''E. histolytica'' cyst from the cysts of nonpathogenic intestinal protozoa such as ''[[Entamoeba coli]]'' by its appearance. ''E. histolytica'' cysts have a maximum of four nuclei, while the commensal ''Entamoeba coli'' has up to 8 nuclei. Additionally, in ''E. histolytica,'' the [[endosome]] is centrally located in the nucleus, while it is off-center in ''Entamoeba coli.'' Finally, [[chromatoidal bodies]] in ''E. histolytica'' are rounded, while they are jagged in ''Entamoeba coli''. However, other species, ''Entamoeba dispar'' and ''E. moshkovskii'', are also a commensal and cannot be distinguished from ''E. histolytica'' under the microscope. As ''E. dispar'' is much more common than ''E. histolytica'' in most parts of the world this means that there is a lot of incorrect diagnosis of ''E. histolytica'' infection taking place. The WHO recommends that infections diagnosed by microscopy alone should not be treated if they are asymptomatic and there is no other reason to suspect that the infection is actually ''E. histolytica''. | Microscopy is still by far the most widespread method of diagnosis around the world. However it is not as sensitive or accurate in diagnosis as the other tests available. It is important to distinguish the ''E. histolytica'' cyst from the cysts of nonpathogenic intestinal protozoa such as ''[[Entamoeba coli]]'' by its appearance. ''E. histolytica'' cysts have a maximum of four nuclei, while the commensal ''Entamoeba coli'' has up to 8 nuclei. Additionally, in ''E. histolytica,'' the [[endosome]] is centrally located in the nucleus, while it is off-center in ''Entamoeba coli.'' Finally, [[chromatoidal bodies]] in ''E. histolytica'' are rounded, while they are jagged in ''Entamoeba coli''. However, other species, ''Entamoeba dispar'' and ''E. moshkovskii'', are also a commensal and cannot be distinguished from ''E. histolytica'' under the microscope. As ''E. dispar'' is much more common than ''E. histolytica'' in most parts of the world this means that there is a lot of incorrect diagnosis of ''E. histolytica'' infection taking place. The WHO recommends that infections diagnosed by microscopy alone should not be treated if they are asymptomatic and there is no other reason to suspect that the infection is actually ''E. histolytica''. | ||
===Food | ===Food Analysis=== | ||
''E. histolytica'' cysts may be recovered from contaminated food by methods similar to those used for recovering ''[[Giardia lamblia]]'' cysts from feces. Filtration is probably the most practical method for recovery from drinking water and liquid foods.''E. histolytica'' cysts must be distinguished from cysts of other parasitic (but nonpathogenic) protozoa and from cysts of free-living protozoa as discussed above. Recovery procedures are not very accurate; cysts are easily lost or damaged beyond recognition, which leads to many falsely negative results in recovery tests. (See the FDA Bacteriological Analytical Manual.) | ''E. histolytica'' cysts may be recovered from contaminated food by methods similar to those used for recovering ''[[Giardia lamblia]]'' cysts from feces. Filtration is probably the most practical method for recovery from drinking water and liquid foods.''E. histolytica'' cysts must be distinguished from cysts of other parasitic (but nonpathogenic) protozoa and from cysts of free-living protozoa as discussed above. Recovery procedures are not very accurate; cysts are easily lost or damaged beyond recognition, which leads to many falsely negative results in recovery tests. (See the FDA Bacteriological Analytical Manual.) | ||
== | ==Gallery== | ||
<gallery> | <gallery> | ||
Image: Amebiasis02.jpeg| '''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis02.jpeg| '''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis06.jpeg| '''Entamoeba histolytica cyst.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis06.jpeg| '''Entamoeba histolytica cyst.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis07.jpeg| '''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis07.jpeg| '''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis08.jpeg| '''Entamoeba histolytica cysts.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis08.jpeg| '''Entamoeba histolytica cysts.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis09.jpeg| '''Intestinal amebiasis infection.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis09.jpeg| '''Intestinal amebiasis infection.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis10.jpeg| '''Histopathology of amebiasis.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis10.jpeg| '''Histopathology of amebiasis.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
Image: Amebiasis19.jpeg|'''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name= | Image: Amebiasis19.jpeg|'''Entamoeba histolytica trophozoite.''' <SMALL><SMALL>''[http://phil.cdc.gov/phil/home.asp Adapted from Public Health Image Library (PHIL).] ''<ref name=PHIL> {{Cite web | title = Public Health Image Library (PHIL) | url = http://phil.cdc.gov/phil/home.asp}}</ref></SMALL></SMALL> | ||
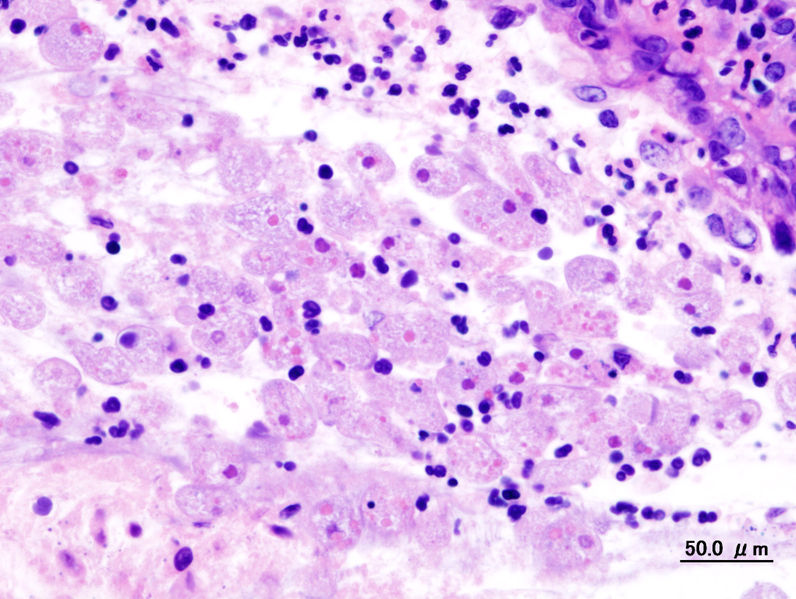
Image:Amoebic dysentery in colon biopsy (1).jpg|'''Amebic dysentery in colon biopsy''' | |||
</gallery> | </gallery> | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
Latest revision as of 17:34, 26 December 2014
|
Amoebiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Amoebiasis laboratory tests On the Web |
|
American Roentgen Ray Society Images of Amoebiasis laboratory tests |
|
Risk calculators and risk factors for Amoebiasis laboratory tests |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2]
Overview
Laboratory Findings
Asymptomatic human infections are usually diagnosed by finding cysts shed with the stool. Various flotation or sedimentation procedures have been developed to recover the cysts from fecal matter and stains help to visualize the isolated cysts for microscopic examination. Since cysts are not shed constantly, a minimum of 3 stools should be examined. In symptomatic infections, the motile form (the trophozoite) can often be seen in fresh feces. Serological tests exist and most individuals (whether with symptoms or not) will test positive for the presence of antibodies. The levels of antibody are much higher in individuals with liver abscesses. Serology only becomes positive about two weeks after infection. More recent developments include a kit that detects the presence of ameba proteins in the feces and another that detects ameba DNA in feces. These tests are not in widespread use due to their expense.
Microscopy is still by far the most widespread method of diagnosis around the world. However it is not as sensitive or accurate in diagnosis as the other tests available. It is important to distinguish the E. histolytica cyst from the cysts of nonpathogenic intestinal protozoa such as Entamoeba coli by its appearance. E. histolytica cysts have a maximum of four nuclei, while the commensal Entamoeba coli has up to 8 nuclei. Additionally, in E. histolytica, the endosome is centrally located in the nucleus, while it is off-center in Entamoeba coli. Finally, chromatoidal bodies in E. histolytica are rounded, while they are jagged in Entamoeba coli. However, other species, Entamoeba dispar and E. moshkovskii, are also a commensal and cannot be distinguished from E. histolytica under the microscope. As E. dispar is much more common than E. histolytica in most parts of the world this means that there is a lot of incorrect diagnosis of E. histolytica infection taking place. The WHO recommends that infections diagnosed by microscopy alone should not be treated if they are asymptomatic and there is no other reason to suspect that the infection is actually E. histolytica.
Food Analysis
E. histolytica cysts may be recovered from contaminated food by methods similar to those used for recovering Giardia lamblia cysts from feces. Filtration is probably the most practical method for recovery from drinking water and liquid foods.E. histolytica cysts must be distinguished from cysts of other parasitic (but nonpathogenic) protozoa and from cysts of free-living protozoa as discussed above. Recovery procedures are not very accurate; cysts are easily lost or damaged beyond recognition, which leads to many falsely negative results in recovery tests. (See the FDA Bacteriological Analytical Manual.)
Gallery
-
Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica cyst. Adapted from Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica cysts. Adapted from Public Health Image Library (PHIL). [1]
-
Intestinal amebiasis infection. Adapted from Public Health Image Library (PHIL). [1]
-
Histopathology of amebiasis. Adapted from Public Health Image Library (PHIL). [1]
-
Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]
-
Amebic dysentery in colon biopsy
References
![Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]](/images/3/35/Amebiasis02.jpeg)
![Entamoeba histolytica cyst. Adapted from Public Health Image Library (PHIL). [1]](/images/a/a5/Amebiasis06.jpeg)
![Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]](/images/5/52/Amebiasis07.jpeg)
![Entamoeba histolytica cysts. Adapted from Public Health Image Library (PHIL). [1]](/images/a/aa/Amebiasis08.jpeg)
![Intestinal amebiasis infection. Adapted from Public Health Image Library (PHIL). [1]](/images/2/2b/Amebiasis09.jpeg)
![Histopathology of amebiasis. Adapted from Public Health Image Library (PHIL). [1]](/images/3/30/Amebiasis10.jpeg)
![Entamoeba histolytica trophozoite. Adapted from Public Health Image Library (PHIL). [1]](/images/c/c4/Amebiasis19.jpeg)