Adenomatoid tumor
|
Adenomatoid tumor Microchapters |
| Adenomatoid tumor | |
| ICD-O: | 9054/0 |
|---|---|
| MeSH | D018254 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Mohsin, M.D.[2]
Overview
Adenomatoid tumor is a benign mesothelial tumor affecting testicular adnexa. It generally presents in the genital tract, in regions such as the testis and epididymis.However, it also has been found in the pancreas.
Pathophysiology
- Adenomatoid tumors are benign, solid extratesticular lesions that can originate from the epididymis, tunica vaginalis, or spermatic cord.[1][2][3]
- They are the most common tumor of the epididymis.[4][5]
- They occur more often in the lower pole than in the upper pole by a ratio of 4:1.[6][7][8]
- Usually an incidental finding, adenomatoid tumors manifest as a painless scrotal mass, with the majority diagnosed in patients aged 20–50 years.[9][10][11]
- They are typically unilateral and occur more frequently on the left side. When they grow noninvasively into the testicular parenchyma, they can simulate intratesticular disease.[12][13][14][15]
Gross pathology
- 1 - 5 cm, well circumscribed solid tumor, adherent to testis / testicular adnexa
- Cut surface may have small cystic spaces
Histopathology
- No distinct growth pattern
- Unencapsulated, cuboidal to flat cells forming cords that are either epithelial-like or form channels with dilated lumina simulating vessels
- Cells have acidophilic cytoplasm with cytoplasmic vacuoles
- Nuclei lack nucleoli
- Mitoses and necrosis are usually absent
- Intervening stroma may have smooth muscle and elastic fibers, desmoplastic quality and inflammatory cells
- Rarely, tumor may extend into testicular parenchyma or even rarer, be totally inside the testis[5][13]
- Patterns have been described but most tumors show a mixture of:[16][17][18][19][20]
- Adenomatoid (tubular): glandular pattern with cytoplasmic vacuoles giving a signet ring appearance
- Angiomatoid (canalicular): cells have a more endothelial appearance
- Solid (plexiform): cells have a more epithelial appearance
- Cystic (mixed): rare; tumor is in form of cystic spaces lined by cuboidal to flattened lining epithelium
Cytology
- Smears are moderately cellular with sheets of monotonous round to oval cells showing indistinct cell borders and moderate to abundant pale cytoplasm with vacuolations [8][21]
- Nuclei are eccentric in location but regular with inconspicuous nucleoli[22][3][15]
Immunostaining
- Adenomatoid tumor stains positive for:[10]
- Calretinin
- Pan cytokeratins (EMA, AE1 / AE3, Cam5.2)
- CK5 / 6
- CK7 (variable, focal to diffuse)
- Adenomatoid tumor stains negative for:
- Vascular / endothelial markers (CD31, CD34)
- CEA
- HBME1
- Factor VIII Ag
- MOC31 / BerEP4
- B72.3
- CD15
- Ulex europeus agglutinin I
- Germ cell markers including:
- OCT3 / 4
- SOX2
- AFP
- PLAP
- CD117
- CD30
- NANOG
Electron microscopy
- Prominent microvilli
- Desmosomes
- Tonofilaments associated with dilated intercellular spaces
Causes
- Mesothelial origin based on immunohistochemical features and ultrastructural studies [23]
- Similar tumor in spermatic cord, ejaculatory duct, fallopian tube, uterus
Epidemiology and Demographics
- 30% of testicular adnexal tumors, 73% of benign tumors of testicular adnexa in study of 314 tumors[24]
- Usually 3rd to 5th decade; rare - 5 year old boy[25] and 70 year old man[26]
Natural History, Complications and Prognosis
- Uniformly benign behavior, no reports of malignant transformation
Diagnosis
- Diagnosis is suspected clinicoradiologically, confirmed histologically
History and Symptoms
Common sites of involvement
- Adenomatoid tumor most commonly involves the following sites:
Symptoms
- Presents as solid, well circumscribed mass in scrotum, often associated with pain
- Usually 1 - 5 cm, rarely larger[30]
- Benign, even if it extends into testis
Laboratory findings
- No specific laboratory finding; however, negative markers for germ cell tumor are helpful in excluding a germ cell malignancy
Ultrasound findings
- On an ultrasound, they appear as a solid extratesticular mass with variable echogenicity.[31]
- USG reveals a relatively hypo, iso to hyperechoic mass at lower pole of epididymis, not distorting the testis
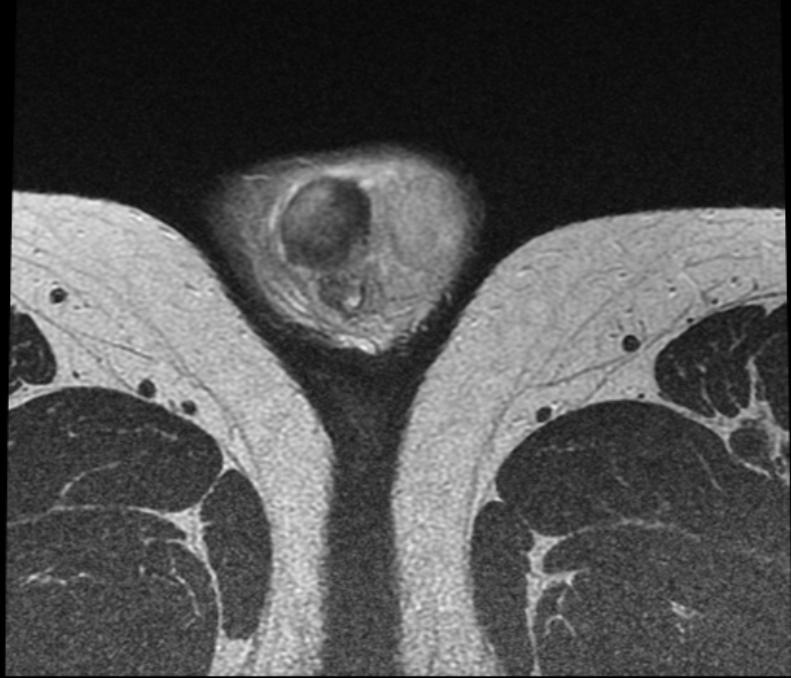
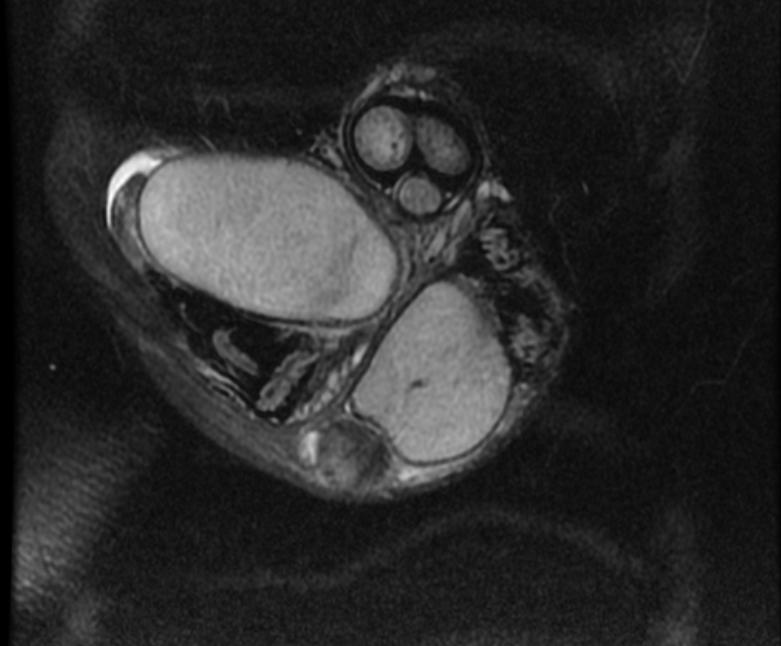
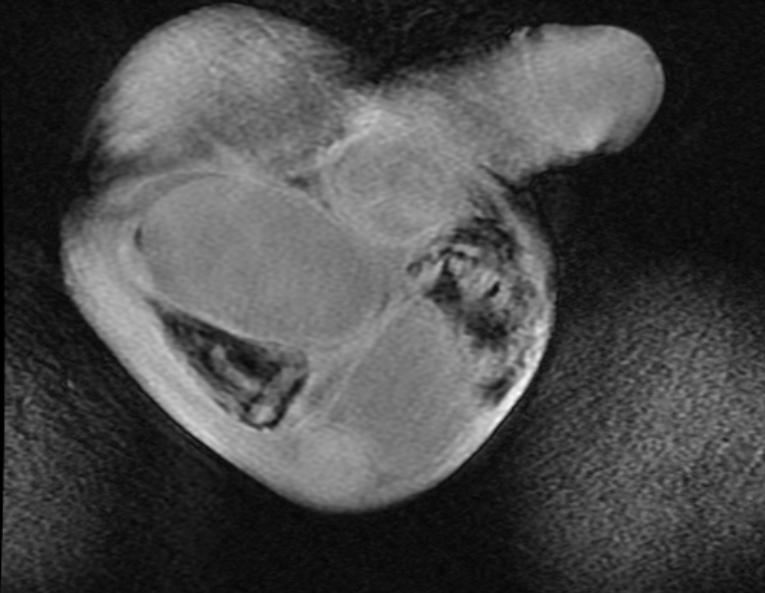
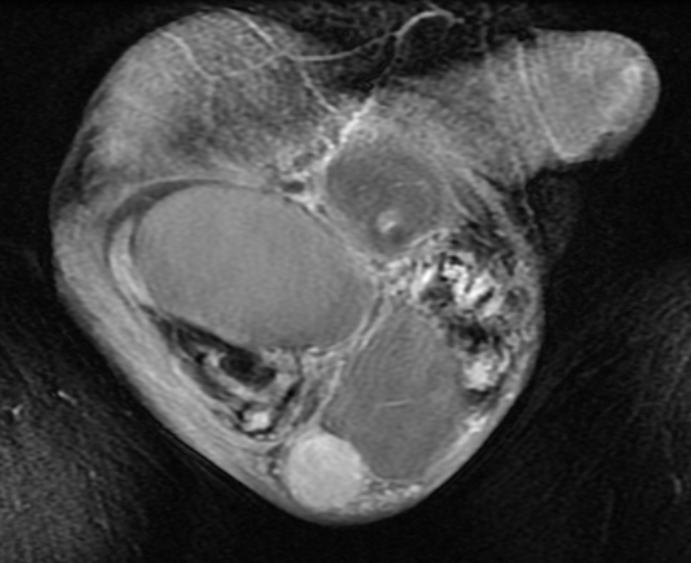
MRI
- Commonly, MRI demonstrates low signal intensity relative to the testicular parenchyma on T2-weighted images.
- MRI can aid in determining the paratesticular origin of the lesion.
- Adenomatoid tumors enhance after administration of gadolinium contrast material.
 |
 |
 |
 |
 |
Treatment
- Complete excision
- Frozen section examination may prevent unnecessary radical orchiectomy[32][33]
- Paratesticular tumors are rare tumors that are difficult to diagnose preoperatively and therefore, many patients are subjected to inguinal orchiectomy. However, radical orchiectomy can be avoided as the diagnosis of paratesticular tumor can be made on the basis of clinical suspicion, findings of tumor markers and radiological tests.
Differentiating Adenomatoid tumor from other diseases
- Adenomatoid tumor must be differentiated from:
- Malignant mesothelioma (HBME1+, mitoses and necrosis)
- Metastatic adenocarcinoma (positive for one or more of CEA, PSA, MOC31 / BerEP4 and CD15 are useful)
- Papillary cystadenoma of epididymis
References
- ↑ Amin W, Parwani AV (2009). "Adenomatoid tumor of testis". Clin Med Pathol. 2: 17–22. PMC 2990235. PMID 21151545.
- ↑ Williams SB, Han M, Jones R, Andrawis R (2004). "Adenomatoid tumor of the testes". Urology. 63 (4): 779–81. doi:10.1016/j.urology.2003.11.035. PMID 15072910.
- ↑ 3.0 3.1 Alam K, Maheshwari V, Varshney M, Aziz M, Shahid M, Basha M; et al. (2011). "Adenomatoid tumour of testis". BMJ Case Rep. 2011. doi:10.1136/bcr.01.2011.3790. PMC 3063256. PMID 22707658.
- ↑ "Adenomatoid tumor of the epididymis". Retrieved 2007-12-15.
- ↑ 5.0 5.1 Migliorini F, Baldassarre R, Artibani W, Martignoni G, Brunelli M (2014). "Rare case of intra-testicular adenomatoid tumour". Arch Ital Urol Androl. 86 (1): 44–5. doi:10.4081/aiua.2014.1.44. PMID 24704932.
- ↑ 6.0 6.1 Oyama H, Ogawa M, Mikuriya H, Kido A, Hayashi H (2001). "[Adenomatoid tumor of testicular tunica albuginea: a case report]". Hinyokika Kiyo. 47 (9): 661–3. PMID 11692607.
- ↑ Shima M, Takahashi S, Maeda T, Masumori N, Itoh N, Tsukamoto T (2009). "[Adenomatoid tumor of the testis with testicular pain: a case report]". Hinyokika Kiyo. 55 (5): 285–6. PMID 19507549.
- ↑ 8.0 8.1 Kalyani R, Das S (2009). "Adenomatatoid tumor: Cytological diagnosis of two cases". J Cytol. 26 (1): 30–2. doi:10.4103/0970-9371.54865. PMC 3167987. PMID 21938146.
- ↑ Barry P, Chan KG, Hsu J, Quek ML (2005). "Adenomatoid tumor of the tunica albuginea". Int J Urol. 12 (5): 516–8. doi:10.1111/j.1442-2042.2005.01091.x. PMID 15948758.
- ↑ 10.0 10.1 Chen D, Yu Z, Ni L, Gui Y, Yang S, Shi B; et al. (2014). "Adenomatoid tumors of the testis: A report of two cases and review of the literature". Oncol Lett. 7 (5): 1718–1720. doi:10.3892/ol.2014.1938. PMC 3997688. PMID 24765207.
- ↑ 11.0 11.1 Alexiev BA, Xu LF, Heath JE, Twaddell WS, Phelan MW (2011). "Adenomatoid tumor of the testis with intratesticular growth: a case report and review of the literature". Int J Surg Pathol. 19 (6): 838–42. doi:10.1177/1066896911398656. PMID 21427102.
- ↑ "Modern Pathology - Adenomatoid Tumor of the Pancreas: A Case Report with Comparison of Histology and Aspiration Cytology". Retrieved 2007-12-15.
- ↑ 13.0 13.1 13.2 Samad AA, Pereiro B, Badiola A, Gallego C, Zungri E (1996). "Adenomatoid tumor of intratesticular localization". Eur Urol. 30 (1): 127–8. PMID 8854081.
- ↑ Pichler R, Tulchiner G, Steinkohl F, Soleiman A, Horninger W, Heidegger IM; et al. (2018). "Adenomatoid tumor of the testis mimicking malignant testicular cancer on multiparametric ultrasound". Eur J Med Res. 23 (1): 3. doi:10.1186/s40001-018-0301-5. PMC 5765709. PMID 29325584.
- ↑ 15.0 15.1 Makkar M, Dayal P, Gupta C, Mahajan N (2013). "Adenomatoid tumor of testis: A rare cytological diagnosis". J Cytol. 30 (1): 65–7. doi:10.4103/0970-9371.107519. PMC 3643368. PMID 23661947.
- ↑ Taxy JB, Battifora H, Oyasu R (1974). "Adenomatoid tumors: a light microscopic, histochemical, and ultrastructural study". Cancer. 34 (2): 306–16. doi:10.1002/1097-0142(197408)34:2<306::aid-cncr2820340214>3.0.co;2-g. PMID 4277347.
- ↑ Quigley JC, Hart WR (1981). "Adenomatoid tumors of the uterus". Am J Clin Pathol. 76 (5): 627–35. doi:10.1093/ajcp/76.5.627. PMID 7293978.
- ↑ Yo H, Mori O, Ohaki Y, Kawamura T, Asano G (1996). "[Three cases of adenomatoid tumor of the uterus]". Nihon Ika Daigaku Zasshi. 63 (4): 294–8. PMID 8810558.
- ↑ Cheng CL, Wee A (2003). "Diffuse uterine adenomatoid tumor in an immunosuppressed renal transplant recipient". Int J Gynecol Pathol. 22 (2): 198–201. PMID 12649678.
- ↑ Otis CN (1996). "Uterine adenomatoid tumors: immunohistochemical characteristics with emphasis on Ber-EP4 immunoreactivity and distinction from adenocarcinoma". Int J Gynecol Pathol. 15 (2): 146–51. PMID 8786204.
- ↑ Gupta S, Garg S, Agarwal R, Sen R (2012). "Aspiration cytology of adenomatoid tumor of epididymis: An important diagnostic tool". J Surg Case Rep. 2012 (4): 11. doi:10.1093/jscr/2012.4.11. PMC 3649525. PMID 24960828.
- ↑ 22.0 22.1 Monappa V, Rao AC, Krishnanand G, Mathew M, Garg S (2009). "Adenomatoid tumor of tunica albuginea mimicking seminoma on fine needle aspiration cytology: a case report". Acta Cytol. 53 (3): 349–52. doi:10.1159/000325324. PMID 19534283.
- ↑ Marcus JB, Lynn JA (1970). "Ultrastructural comparison of an adenomatoid tumor, lymphangioma, hemangioma, and mesothelioma". Cancer. 25 (1): 171–5. doi:10.1002/1097-0142(197001)25:1<171::aid-cncr2820250125>3.0.co;2-2. PMID 5410308.
- ↑ Beccia DJ, Krane RJ, Olsson CA (1976). "Clinical management of non-testicular intrascrotal tumors". J Urol. 116 (4): 476–9. doi:10.1016/s0022-5347(17)58867-9. PMID 802862.
- ↑ Liu W, Wu RD, Yu QH (2011). "Adenomatoid tumor of the testis in a child". J Pediatr Surg. 46 (10): E15–7. doi:10.1016/j.jpedsurg.2011.06.020. PMID 22008356.
- ↑ Morote J, Rabella A, Benasco C (1984). "[Adenomatoid tumor of the epididymis]". Arch Esp Urol. 37 (1): 61–4. PMID 6721596.
- ↑ Cabral Ribeiro J, Sousa L, Gonçalves V (2018). "[Tunica albuginea adenomatoid tumor. A challenging case managed conservatively]". Rev Int Androl. 16 (2): 82–86. doi:10.1016/j.androl.2017.02.008. PMID 30300129.
- ↑ Sun AY, Polackwich AS, Sabanegh ES (2016). "Adenomatoid Tumor of the Testis Arising From the Tunica Albuginea". Rev Urol. 18 (1): 51–3. PMC 4859931. PMID 27162515.
- ↑ Pacheco AJ, Torres JL, de la Guardia FV, Arrabal Polo MA, Gómez AZ (2009). "Intraparenchymatous adenomatoid tumor dependent on the rete testis: A case report and review of literature". Indian J Urol. 25 (1): 126–8. doi:10.4103/0970-1591.45551. PMC 2684313. PMID 19468443.
- ↑ Ferenczy A, Fenoglio J, Richart RM (1972). "Observations on benign mesothelioma of the genital tract (adenomatoid tumor). A comparative ultrastructural study". Cancer. 30 (1): 244–60. doi:10.1002/1097-0142(197207)30:1<244::aid-cncr2820300135>3.0.co;2-c. PMID 5040745.
- ↑ Urkmez A, Akan S, Ozsoy E, Sahin A, Koca O, Ozturk MI (2018). "Diagnosis and Treatment of Paratesticular Adenomatoid Tumors". J Coll Physicians Surg Pak. 28 (9): S217–S219. doi:10.29271/jcpsp.2018.09.S217. PMID 30173704.
- ↑ Goel A, Jain A, Dalela D (2011). "Can radical orchiectomy be avoided for paratesticular adenomatoid tumor?". Indian J Urol. 27 (4): 556–7. doi:10.4103/0970-1591.91454. PMC 3263233. PMID 22279331.
- ↑ Subik MK, Gordetsky J, Yao JL, di Sant'Agnese PA, Miyamoto H (2012). "Frozen section assessment in testicular and paratesticular lesions suspicious for malignancy: its role in preventing unnecessary orchiectomy". Hum Pathol. 43 (9): 1514–9. doi:10.1016/j.humpath.2011.11.013. PMID 22406369.