Acute respiratory distress syndrome overview: Difference between revisions
No edit summary |
|||
| Line 210: | Line 210: | ||
*[[Mechanical ventilation modes of ventilation#High Frequency Ventilation (HFV)|'''High-frequency oscillatory ventilation (HFOV)''']] may improve oxygenation in patients with '''moderate to severe ARDS and severe refractory hypoxemia''', however, initiation of HFOV early in the course of ARDS (i.e., prior to low tidal volume/high PEEP mechanical ventilation) has been associated with ''increased mortality'' compared to low tidal volume/high PEEP ventilation<ref name="pmid12231488">{{cite journal| author=Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG et al.| title=High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. | journal=Am J Respir Crit Care Med | year= 2002 | volume= 166 | issue= 6 | pages= 801-8 | pmid=12231488 | doi=10.1164/rccm.2108052 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12231488 }} </ref><sup>,</sup><ref name="pmid23339639">{{cite journal| author=Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P et al.| title=High-frequency oscillation in early acute respiratory distress syndrome. | journal=N Engl J Med | year= 2013 | volume= 368 | issue= 9 | pages= 795-805 | pmid=23339639 | doi=10.1056/NEJMoa1215554 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23339639 }} </ref> | *[[Mechanical ventilation modes of ventilation#High Frequency Ventilation (HFV)|'''High-frequency oscillatory ventilation (HFOV)''']] may improve oxygenation in patients with '''moderate to severe ARDS and severe refractory hypoxemia''', however, initiation of HFOV early in the course of ARDS (i.e., prior to low tidal volume/high PEEP mechanical ventilation) has been associated with ''increased mortality'' compared to low tidal volume/high PEEP ventilation<ref name="pmid12231488">{{cite journal| author=Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG et al.| title=High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial. | journal=Am J Respir Crit Care Med | year= 2002 | volume= 166 | issue= 6 | pages= 801-8 | pmid=12231488 | doi=10.1164/rccm.2108052 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12231488 }} </ref><sup>,</sup><ref name="pmid23339639">{{cite journal| author=Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P et al.| title=High-frequency oscillation in early acute respiratory distress syndrome. | journal=N Engl J Med | year= 2013 | volume= 368 | issue= 9 | pages= 795-805 | pmid=23339639 | doi=10.1056/NEJMoa1215554 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23339639 }} </ref> | ||
*'''[[Acute respiratory distress syndrome mechanical ventilation therapy#APRV (Airway Pressure Release Ventilation) and ARDS / ALI |Airway pressure release ventilation (APRV)]]''' appears to be safe in ARDS, and may be associated with reduced paralytic and sedative use as well as an increase in the number of ventilator-free days<ref name="pmid19727373">{{cite journal| author=Daoud EG| title=Airway pressure release ventilation. | journal=Ann Thorac Med | year= 2007 | volume= 2 | issue= 4 | pages= 176-9 | pmid=19727373 | doi=10.4103/1817-1737.36556 | pmc=2732103 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19727373 }} </ref><sup>,</sup><ref name="pmid21762559">{{cite journal| author=Daoud EG, Farag HL, Chatburn RL| title=Airway pressure release ventilation: what do we know? | journal=Respir Care | year= 2012 | volume= 57 | issue= 2 | pages= 282-92 | pmid=21762559 | doi=10.4187/respcare.01238 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21762559 }} </ref> | *'''[[Acute respiratory distress syndrome mechanical ventilation therapy#APRV (Airway Pressure Release Ventilation) and ARDS / ALI |Airway pressure release ventilation (APRV)]]''' appears to be safe in ARDS, and may be associated with reduced paralytic and sedative use as well as an increase in the number of ventilator-free days<ref name="pmid19727373">{{cite journal| author=Daoud EG| title=Airway pressure release ventilation. | journal=Ann Thorac Med | year= 2007 | volume= 2 | issue= 4 | pages= 176-9 | pmid=19727373 | doi=10.4103/1817-1737.36556 | pmc=2732103 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19727373 }} </ref><sup>,</sup><ref name="pmid21762559">{{cite journal| author=Daoud EG, Farag HL, Chatburn RL| title=Airway pressure release ventilation: what do we know? | journal=Respir Care | year= 2012 | volume= 57 | issue= 2 | pages= 282-92 | pmid=21762559 | doi=10.4187/respcare.01238 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21762559 }} </ref> | ||
=== Extracorporeal Membrane Oxygenation (ECMO) === | |||
There is growing evidence to support the use of [[extracorporeal membrane oxygenation]] (ECMO) for severe ARDS that fails to improve despite judicious application of the ARDS Network low tidal volume/high PEEP ventilation strategy.<ref name="pmid3090285">{{cite journal| author=Gattinoni L, Pesenti A, Mascheroni D, Marcolin R, Fumagalli R, Rossi F et al.| title=Low-frequency positive-pressure ventilation with extracorporeal CO2 removal in severe acute respiratory failure. | journal=JAMA | year= 1986 | volume= 256 | issue= 7 | pages= 881-6 | pmid=3090285 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3090285 }} </ref> | |||
<sup>,</sup><ref name="pmid19762075">{{cite journal| author=Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM et al.| title=Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. | journal=Lancet | year= 2009 | volume= 374 | issue= 9698 | pages= 1351-63 | pmid=19762075 | doi=10.1016/S0140-6736(09)61069-2 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19762075 }} </ref> ECMO facilitates gas exchange in circumstances where adequate oxygenation and ventilation cannot be achieved through the lungs themselves. There are two main forms of ECMO, both of which have been used successfully in the treatment of severe ARDS: | |||
*'''Veno-venous (VV)-ECMO''': Venous blood is removed through an outflow cannula placed in a large vein (usually the right femoral vein or inferior vena cava) and passed through an oxygenator where gas exchange occurs (CO<sub>2</sub> is removed and O<sub>2</sub> is introduced) before being returned to the body through an inflow cannula placed in another large vein (usually the right internal jugular vein or superior vena cava) | |||
:*Supports gas exchange but does not provide any hemodynamic support | |||
*'''Veno-arterial(VA)-ECMO''': Venous blood is removed through an outflow cannula placed in a large vein (usually the right femoral vein or inferior vena cava) and passed through an oxygenator where gas exchange occurs (CO<sub>2</sub> is removed and O<sub>2</sub> is introduced) before being returned to the body through an inflow cannula placed in a large artery (usually the right femoral artery or right carotid artery) | |||
ECMO works by removing venous blood (e.g., the right femoral vein, right internal jugular vein, or the right atrium) | |||
:*Supports gas exchange and provides hemodynamic support by bypassing the heart completely | |||
The use of ECMO in the treatment of ARDS is an ongoing area of research, and referral to a medical center with ample experience in the use of ECMO for ARDS should be considered for patients with ARDS who are failing traditional management strategies and may be candidates for ECMO. | |||
=== Inhaled Pulmonary Vasodilators === | === Inhaled Pulmonary Vasodilators === | ||
| Line 222: | Line 233: | ||
*Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3]. | *Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3]. | ||
*Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | *Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | ||
==References== | ==References== | ||
Revision as of 04:20, 20 June 2016
|
Acute respiratory distress syndrome Microchapters |
|
Differentiating Acute respiratory distress syndrome from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Acute respiratory distress syndrome overview On the Web |
|
American Roentgen Ray Society Images of Acute respiratory distress syndrome overview |
|
Directions to Hospitals Treating Acute respiratory distress syndrome |
|
Risk calculators and risk factors for Acute respiratory distress syndrome overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Acute respiratory distress syndrome (ARDS), originally known as adult respiratory distress syndrome (to contrast with neonatal respiratory distress syndrome) is a serious and potentially life-threatening inflammatory lung condition that develops rapidly (usually within 24 to 48 hours) in the setting of sepsis, toxic exposures, adverse drug reactions, trauma, or other critical illnesses. ARDS is characterized by inflammation of the lung parenchyma resulting in increased permeability of the alveolar-capillary membrane, non-cardiogenic pulmonary edema, impaired gas exchange, and decreased lung compliance.
The vast majority of patients with ARDS are managed in an intensive care unit, and nearly all will require mechanical ventilation at some point during the course of their illness and recovery. ARDS may be categorized as mild, moderate, or severe based on the degree to which oxygenation is impaired; however, all levels of severity carry a high mortality rate if appropriate measures to improve oxygenation and minimize the risk of further lung injury are not taken.[1]
Historical Perspective
Although the first pathologic descriptions of what was likely ARDS date back to the 19th century, our understanding of the distinct pathophysiologic features of ARDS evolved alongside the development of medical technologies that facilitated a more in-depth study of the syndrome. The advent of radiography permitted visualization of the bilateral pulmonary infiltrates (originally termed double pneumonia), while the development of arterial blood gas measurement and positive-pressure mechanical ventilation allowed for identification of the impaired oxygenation and reduced lung compliance that are now recognized as central features of ARDS.[2]
Ashbaugh and colleagues published he first description of what is now widely recognized as ARDS in a case series of 12 patients with rapidly progressive respiratory failure with bilateral pulmonary infiltrates and profound hypoxemia following trauma or infection in The Lancet in 1967.[3] The clinical syndrome was called the "adult respiratory distress syndrome" (ARDS) to distinguish it from the respiratory distress syndrome of infancy due to hyaline membrane disease, although the A in ARDS was later changed from acute to adult once it was recognized that the syndrome could also present in infants as a distinct entity from hyaline membrane disease.
Classification
The current ARDS diagnostic criteria (commonly referred to as the Berlin Criteria or Berlin Definition) were established by the ARDS Definition Task Force in 2012. The Berlin Criteria classify ARDS as mild, moderate, and severe based on the degree of oxygenation impairment and serve as a means of risk-stratifying patients.[1]
Pathophysiology
ARDS typically develops within 24 to 48 hours of the provoking illness or injury and is classically divided into three phases:
- Exudative phase (within 24-48 hours): Systemic inflammation results in increased alveolar capillary permeability and leads to the formation of hyaline membranes along alveolar walls, accumulation of proteinaceous exudate within the alveolar air spaces (non-cardiogenic pulmonary edema), and extravasation of inflammatory cells (predominantly neutrophils and macrophages) into the lung parenchyma, leading to extensive alveolar damage and sometimes hemorrhage into alveoli
- Proliferative phase (within 5-7 days): Fibroblast proliferation, collagen deposition, and early fibrotic changes are observed within the pulmonary interstitium as alveolar exudate and hyaline membranes begin to be absorbed
- Fibrotic phase (within several weeks): Most patients with ARDS will develop some degree of pulmonary fibrosis, of which at least one-quarter will go on to develop a restrictive ventilatory defect on pulmonary function tests[4]; the development and extent of pulmonary fibrosis in ARDS correlates with an increased mortality risk[5]
Genetic Susceptibility
The role of genetics in the development of ARDS is an ongoing area of research. While studies have demonstrated associations between certain genetic factors (including single-nucleotide polymorphisms and allelic variants of angiotensin-converting enzyme[6],[7]) and increased susceptibility to developing ARDS, the nature and implications of these relationships remain uncertain.[8]
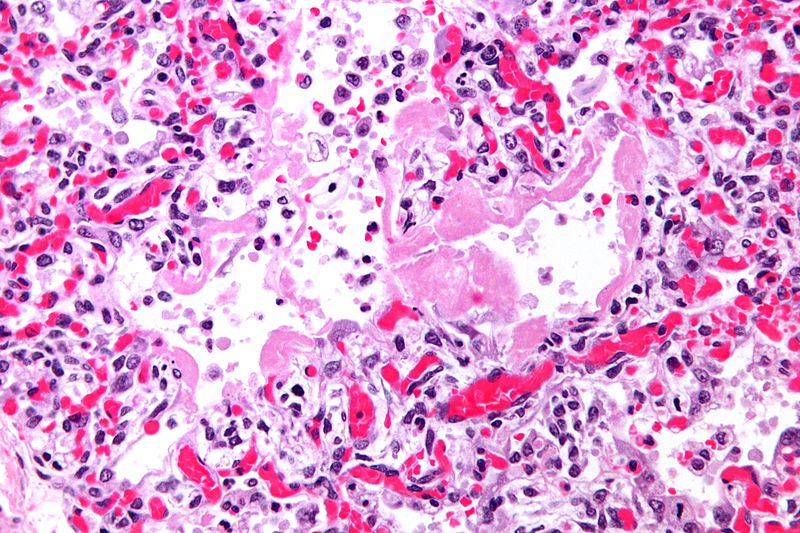
Pathology
- On gross pathology, the lungs are firm, boggy, and dusky, and they typically weigh more than healthy lungs due to edema
- On microscopic histopathological analysis, the lung parenchyma demonstrates hyaline membranes lining the alveolar air spaces, edema fluid within alveoli and the interstitium, shedding of type I pneumocytes and proliferation of type II pneumocytes, infiltration of polymorphonuclear and other inflammatory cells into the interstitial and alveolar compartments, thrombosis and obliteration of pulmonary capillaries, and occasionally hemorrhage into alveoli
- Features specific to the underlying disease process (e.g., bacterial pneumonia or aspiration pneumonitis) are often seen as well
- As ARDS progresses, alveolar infiltrates are reabsorbed and the inflammatory milieu is replaced by increased collagen deposition and proliferating fibroblasts, culminating in interstitial fibrosis
Causes
ARDS may occur as the result of either a direct or indirect insult to the lungs:
- Direct insult: Pneumonia, aspiration pneumonitis, toxic inhalation, smoke inhalation, fat embolism, amniotic fluid embolism, physical trauma to the lungs (e.g., lung contusion)
- Indirect insult: Sepsis, blood transfusion, adverse drug reaction, toxic exposures, extrapulmonary traumatic injury, pancreatitis, burns, cardiopulmonary bypass
Sepsis is the most common cause of ARDS, followed by aspiration pneumonitis and transfusion-related acute lung injury[9] Certain medical comorbidities (e.g., chronic liver or kidney disease, alcoholism, infection with the human immunodeficiency virus, prior organ transplantation) predispose to the development of ARDS, and the risk for developing ARDS increases along with the number of acute insults (e.g., pneumonia and pancreatitis versus pancreatitis alone).
Differentiating ARDS from other Diseases
Prior to the development of the Berlin Definition in 2012, a greater emphasis was placed on excluding other potential illnesses prior to making a diagnosis of ARDS. While it is important to recognize and treat and underlying cause of the patient's impaired ventilation and hypoxemia, this search for potential etiologies should not delay any efforts to improve oxygenation and ventilation.
On chest X-ray, the bilateral, non-cardiogenic pulmonary infiltrates of ARDS may appear similar to those of cardiogenic (hydrostatic) pulmonary edema. Therefore, it is necessary to formally assess cardiac function and volume status if ARDS is suspected but no clear precipitating insult (e.g., sepsis, trauma, toxic inhalation) can be identified. The preferred methods for making this assessment in the ICU are:
- Echocardiography to assess heart function
- Central venous catheterization to measure central venous pressure
- Pulmonary artery (Swan-Ganz) catheterization to measure right-sided heart pressures and pulmonary capillary wedge pressure (a surrogate of left atrial pressure)
Because ARDS is a clinical syndrome that, by definition, occurs in the setting of another illness or insult, identification and treatment of the underlying cause of ARDS is essential. Some standard components of this workup include:
- Chest X-ray
- Arterial blood gases
- Complete blood count with differential
- Comprehensive metabolic panel (serum electrolytes, blood urea nitrogen and creatinine, and tests of liver function)
- Coagulation markers (partial thromboplastin time and prothrombin time with international normalized ratio)
- Blood, sputum, and urine cultures
- Serum lactate
Additional testing should be guided by clinical suspicion and the patient's medical history. These may include such tests as:
- Serum lipase
- Urine or blood toxicology screens
- Blood alcohol level
- Human immunodeficiency virus (HIV) screen
- Respiratory virus screen (direct fluorescent antibody or polymerase chain reaction testing)
- Influenza virus testing
- Fungal cultures
- Tests for atypical pathogens that may cause pneumonia, for example:
- Legionella pneumophila culture and urine antigen testing
- Mycoplasma pneumoniae culture and antibody titers
- Pneumocystis jirovecii sputum silver stain and culture
- Mycobacterium tuberculosis sputum smear and culture
Epidemiology and Demographics
The incidence of ARDS in the United States is estimated at around 75 cases per 100,000 person-years, which amounts to roughly 150,000 new cases per year.[10] There is substantial variance in the rates of ARDS between different countries and geographic regions due to factors such as mean life expectancy, prevalence of different risk factors and comorbidities, and access to health care.
Age
- Advanced age is a non-modifiable risk factor for the development of ARDS
Gender
- Some studies have suggested that women are slightly more likely than men to develop ARDS, however, the mortality rate may be slightly higher among men than women[11],[12]
Race
- There does not appear to be a racial predilection for ARDS, however, in the United States the mortality rate among African Americans with ARDS is higher than for whites[11]
Risk Factors
Common risk factors in the development of ARDS are:
- Advanced age
- Chronic alcoholism
- Chronic liver disease
- Chronic kidney disease
- Cigarette smoke exposure
- Hypoproteinemia[13]
The association between chronic alcoholism and a higher risk of developing ARDS has been demonstrated in several research studies.[14],[15] In one such study, patients with a history of alcohol abuse were roughly twice as likely to develop ARDS and experienced a mortality rate that was 36% higher than age-, sex-, and disease-matched patients without a history of alcohol abuse.[14]
Natural History, Complications and Prognosis
- ARDS typically occurs within the first week of the precipitating illness or trauma and usually progresses rapidly within the first 24 to 48 hours.
- The early clinical features of ARDS include:
- Hypoxemia (a declining peripheral blood oxygen saturation [SpO2] on pulse oximetry or a declining partial pressure of oxygen [PaO2] on arterial blood gas analysis) requiring high concentrations of supplemental oxygen (i.e., a higher fraction of inspired oxygen [FIO2]) or positive pressure ventilation (i.e., a higher continuous positive airway pressure [CPAP] or a higher positive end-expiratory pressure [PEEP]) in order to maintain acceptable blood oxygenation
- Tachypnea and labored breathing
- Tachycardia
- Signs or symptoms that suggest worsening of the underlying illness
- Left untreated, the mortality rate from ARDS is estimated to be upwards of 70%.[16] Long-term sequelae are more likely to develop among those who do not receive adequate treatment and include:
- Significant weakness due to muscle atrophy, sometimes leading to lifelong physical disability
- Impaired lung function
- Chronic ventilator dependency
- Pulmonary fibrosis
- Psychiatric illness (e.g., post-traumatic stress disorder [PTSD], anxiety, and depression)
- Cognitive impairment
- The most common complications of ARDS are those associated with a prolonged ICU stay:
- Secondary or nosocomial infections (e.g., ventilator-associated pneumonia [VAP] or central line-associated blood stream infection [CLABSI])
- Venous thromboembolic events (e.g., deep vein thrombosis [DVT] or pulmonary embolism [PE])
- Gastrointestinal bleeding
- Pressure ulcers and poor wound-healing
- Muscle wasting and atrophy
- Prognosis for patients with ARDS varies based on the severity of illness, the precipitating insult, and medical comorbidities:
- The mortality rate among patients with ARDS due to trauma appears to be lower than among patients with ARDS due to sepsis[17]
- The ARDS Definition Task Force calculated 90-day morality rates for mild, moderate, and severe ARDS as 27%, 32%, and 45%, respectively[1]
- One study of patients diagnosed with ARDS in Maryland, United States, from 1992 through 1995 calculated an in-hospital mortality rate of 36% to 52%[16]
- The 1-year mortality rate for patients with ARDS who survive to hospital discharge varies widely between different studies and is estimated to be anywhere from 11% to over 40%[18],[19],[20]
Diagnosis
Diagnostic Criteria
The diagnosis of ARDS is made when the following diagnostic criteria are met:[1]
| Acute Respiratory Distress Syndrome | |
|---|---|
| Timing | ❑ Within 1 week of a known clinical insult or new or worsening respiratory symptoms |
| Chest imaging a | ❑ Bilateral opacities – not fully explained by effusions, lobar/lung collapse, or nodule |
| Origin of edema | ❑ Respiratory failure not fully explained by cardiac failure or fluid overload b |
| Oxygenation c | |
|
❑ 200 mm Hg < PaO2/FiO2 ≤ 300 mmHg with PEEP or CPAP > 5 cm H2O d |
|
❑ 100 mm Hg < PaO2/FIO2 ≤ 200 mm Hg with PEEP ≥ 5 cm H2O |
|
❑ PaO2/FiO2 ≤ 100 mm Hg with PEEP ≥ 5 cm H2O |
| |
Symptoms
Symptoms of ARDS are fairly nonspecific and typically include:
- Tachypnea
- Shortness of breath
- Tachycardia
- Symptoms associated with the underlying illness/trauma
Physical Examination
There are no physical exam findings specific to/pathognomonic of ARDS. The most notable physical exam findings tend to be those of the underlying illness/trauma.
Laboratory Findings
The most important laboratory finding in ARDS is an arterial partial pressure of oxygen (PaO2 that is inappropriately low relative to the fraction of inspired oxygen (FIO2) that is being administered to the patient. This is referred to as the PaO2 to FIO2 ratio (sometimes abbreviated as P/F ratio) and is calculated by dividing the PaO2 (in mm Hg) by the FIO2 (as a decimal):
- A patient with a PaO2 of 80 mm Hg who is mechanically ventilated with an FIO2 of 35% and a PEEP of 5 cm H2O has a PaO2/FIO2 ratio of 80/0.35 = 229 (mild ARDS)
- A patient with a PaO2 of 80 mm Hg who is mechanically ventilated with an FIO2 of 50% and a PEEP of 5 cm H2O has a PaO2/FIO2 ratio of 80/0.40 = 160 (moderate ARDS)
- A patient with a PaO2 of 80 mm Hg who is mechanically ventilated with an FIO2 of 80% and a PEEP of 5 cm H2O has a PaO2/FIO2 ratio of 80/0.80 = 100 (severe ARDS)
Other notable laboratory findings are those that support an underlying diagnosis that led to the development of ARDS (e.g., positive blood cultures and an elevated white blood cell count in a septic patient or an elevated lipase in a patient with acute pancreatitis).
Imaging Findings
Chest X-ray is the preferred imaging modality in the assessment of ARDS. Classic findings of ARDS on chest X-ray include:

- Diffuse, hazy airspace opacities that are bilateral but often asymmetric
- Obscuration of the pulmonary vessels
Computed tomography (CT) may also be used in the evaluation of patients with ARDS. Although there are no CT findings that are diagnostic of ARDS, some common features include:

- Pulmonary opacification that appears more dense in the dependent lung zones
- Ground-glass opacities that may either be patchy or diffuse
- Islands of normal-appearing lung parenchyma
Other Diagnostic Studies
There are no other diagnostic studies specific to ARDS beyond chest radiography to identify bilateral airspace opacities and arterial blood gas analysis to calculate the PaO2/FIO2 ratio.
Treatment
Medical Therapy
Medical therapies for ARDS that have been demonstrated to improve outcomes are:
- Lower tidal volume ventilation (≤ 6 ml/kg predicted body weight) is associated with reduced mortality and a greater number of ventilator-free days[23]
- Lower tidal volume ventilation should be continued even if the arterial partial pressure of carbon dioxide (PaCO2) rises (this is called permissive hypercapnia)
- Permissive hypercapnia usually results in a drop in blood pH, however, treatment of acidemia (e.g., intravenous administration of sodium bicarbonate or tromethamine) is not indicated if the pH remains at or above 7.15 to 7.20
- Higher positive end-expiratory pressure (PEEP) combined with lower tidal volume ventilation is associated with decreased mortality in patients with moderate or severe ARDS (PaO2/FIO2 ≤ 200)[24]
- Prone positioning for at least 16 consecutive hours each day is associated with improved 28-day and 90-day survival in patients with ARDS and a PaO2/FIO2 ratio < 150 on an FIO2 ≥ 60% and PEEP ≥ 5 mm Hg
- Cisatracurium, when started within the first 48 hours of ARDS diagnosis and continued for 48 hours, have been associated with improved 90-day survival, a greater number of ventilator-free days, and a decreased incidence of barotrauma[25]
ARDS Network Mechanical Ventilation Protocol
In 1994 the National Institutes of Health (NIH) and National Heart, Lung, and Blood Institute (NHLBI) founded the ARDS Network (often abbreviated as ARDSnet) – a consortium of over 40 hospitals that conduct clinical research trials aimed at improving care for patients with ARDS. In order to simplify the mechanical ventilation of patients with ARDS, the NIH-NHLBI ARDS Network has compiled a Mechanical Ventilation Protocol Summary that outlines the mechanical ventilation strategies associated with better outcomes in an easy-to-use format for ICU health care providers.[26]
Alternative Mechanical Ventilation Strategies
Several specialized modes of mechanical ventilation have been tested in ARDS, however, none carries a morbidity or mortality benefit and should only be considered if oxygenation does not improve with a judicious trial of the first-line mechanical ventilation strategies as outlined by the ARDS Network.[27]
- High-frequency oscillatory ventilation (HFOV) may improve oxygenation in patients with moderate to severe ARDS and severe refractory hypoxemia, however, initiation of HFOV early in the course of ARDS (i.e., prior to low tidal volume/high PEEP mechanical ventilation) has been associated with increased mortality compared to low tidal volume/high PEEP ventilation[28],[29]
- Airway pressure release ventilation (APRV) appears to be safe in ARDS, and may be associated with reduced paralytic and sedative use as well as an increase in the number of ventilator-free days[30],[31]
Extracorporeal Membrane Oxygenation (ECMO)
There is growing evidence to support the use of extracorporeal membrane oxygenation (ECMO) for severe ARDS that fails to improve despite judicious application of the ARDS Network low tidal volume/high PEEP ventilation strategy.[32] ,[33] ECMO facilitates gas exchange in circumstances where adequate oxygenation and ventilation cannot be achieved through the lungs themselves. There are two main forms of ECMO, both of which have been used successfully in the treatment of severe ARDS:
- Veno-venous (VV)-ECMO: Venous blood is removed through an outflow cannula placed in a large vein (usually the right femoral vein or inferior vena cava) and passed through an oxygenator where gas exchange occurs (CO2 is removed and O2 is introduced) before being returned to the body through an inflow cannula placed in another large vein (usually the right internal jugular vein or superior vena cava)
- Supports gas exchange but does not provide any hemodynamic support
- Veno-arterial(VA)-ECMO: Venous blood is removed through an outflow cannula placed in a large vein (usually the right femoral vein or inferior vena cava) and passed through an oxygenator where gas exchange occurs (CO2 is removed and O2 is introduced) before being returned to the body through an inflow cannula placed in a large artery (usually the right femoral artery or right carotid artery)
ECMO works by removing venous blood (e.g., the right femoral vein, right internal jugular vein, or the right atrium)
- Supports gas exchange and provides hemodynamic support by bypassing the heart completely
The use of ECMO in the treatment of ARDS is an ongoing area of research, and referral to a medical center with ample experience in the use of ECMO for ARDS should be considered for patients with ARDS who are failing traditional management strategies and may be candidates for ECMO.
Inhaled Pulmonary Vasodilators
Inhaled pulmonary vasodilators have been used to improve hypoxemia by reversing ventilation/perfusion (V/Q) mismatching, however, studies of inhaled nitric oxide (iNO) and inhaled prostacyclin have not demonstrated a survival benefit.[34],[35],[36],[37] It is important to monitor the platelet count when initiating treatment with inhaled prostacyclin due to the low risk of thrombocytopenia.
Surgery
Surgical treatment plays no role in the management of ARDS, except where an operation might be recommended to treat the underlying cause.
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
References
- ↑ 1.0 1.1 1.2 1.3 ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E; et al. (2012). "Acute respiratory distress syndrome: the Berlin Definition". JAMA. 307 (23): 2526–33. doi:10.1001/jama.2012.5669. PMID 22797452.
- ↑ Bernard GR (2005). "Acute respiratory distress syndrome: a historical perspective". Am J Respir Crit Care Med. 172 (7): 798–806. doi:10.1164/rccm.200504-663OE. PMC 2718401. PMID 16020801.
- ↑ Ashbaugh DG, Bigelow DB, Petty TL, Levine BE (1967). "Acute respiratory distress in adults". Lancet. 2 (7511): 319–23. PMID 4143721.
- ↑ Burnham EL, Janssen WJ, Riches DW, Moss M, Downey GP (2014). "The fibroproliferative response in acute respiratory distress syndrome: mechanisms and clinical significance". Eur Respir J. 43 (1): 276–85. doi:10.1183/09031936.00196412. PMC 4015132. PMID 23520315.
- ↑ Martin C, Papazian L, Payan MJ, Saux P, Gouin F (1995). "Pulmonary fibrosis correlates with outcome in adult respiratory distress syndrome. A study in mechanically ventilated patients". Chest. 107 (1): 196–200. PMID 7813276.
- ↑ Jerng JS, Yu CJ, Wang HC, Chen KY, Cheng SL, Yang PC (2006). "Polymorphism of the angiotensin-converting enzyme gene affects the outcome of acute respiratory distress syndrome". Crit Care Med. 34 (4): 1001–6. doi:10.1097/01.CCM.0000206107.92476.39. PMID 16484896.
- ↑ Cardinal-Fernández P, Ferruelo A, El-Assar M, Santiago C, Gómez-Gallego F, Martín-Pellicer A; et al. (2013). "Genetic predisposition to acute respiratory distress syndrome in patients with severe sepsis". Shock. 39 (3): 255–60. doi:10.1097/SHK.0b013e3182866ff9. PMID 23364437.
- ↑ Tejera P, Meyer NJ, Chen F, Feng R, Zhao Y, O'Mahony DS; et al. (2012). "Distinct and replicable genetic risk factors for acute respiratory distress syndrome of pulmonary or extrapulmonary origin". J Med Genet. 49 (11): 671–80. doi:10.1136/jmedgenet-2012-100972. PMC 3654537. PMID 23048207.
- ↑ Pepe PE, Potkin RT, Reus DH, Hudson LD, Carrico CJ (1982). "Clinical predictors of the adult respiratory distress syndrome". Am J Surg. 144 (1): 124–30. PMID 7091520.
- ↑ Lucas AC (1988). "The future of radiological instrumentation". Health Phys. 55 (2): 191–5. PMID 3410685.
- ↑ 11.0 11.1 Moss M, Mannino DM (2002). "Race and gender differences in acute respiratory distress syndrome deaths in the United States: an analysis of multiple-cause mortality data (1979- 1996)". Crit Care Med. 30 (8): 1679–85. PMID 12163776.
- ↑ Heffernan DS, Dossett LA, Lightfoot MA, Fremont RD, Ware LB, Sawyer RG; et al. (2011). "Gender and acute respiratory distress syndrome in critically injured adults: a prospective study". J Trauma. 71 (4): 878–83, discussion 883-5. doi:10.1097/TA.0b013e31822c0d31. PMC 3201740. PMID 21986736.
- ↑ Mangialardi RJ, Martin GS, Bernard GR, Wheeler AP, Christman BW, Dupont WD; et al. (2000). "Hypoproteinemia predicts acute respiratory distress syndrome development, weight gain, and death in patients with sepsis. Ibuprofen in Sepsis Study Group". Crit Care Med. 28 (9): 3137–45. PMID 11008971.
- ↑ 14.0 14.1 Moss M, Bucher B, Moore FA, Moore EE, Parsons PE (1996). "The role of chronic alcohol abuse in the development of acute respiratory distress syndrome in adults". JAMA. 275 (1): 50–4. PMID 8531287.
- ↑ Moss M, Burnham EL (2003). "Chronic alcohol abuse, acute respiratory distress syndrome, and multiple organ dysfunction". Crit Care Med. 31 (4 Suppl): S207–12. doi:10.1097/01.CCM.0000057845.77458.25. PMID 12682442.
- ↑ 16.0 16.1 Reynolds HN, McCunn M, Borg U, Habashi N, Cottingham C, Bar-Lavi Y (1998). "Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million-person population base". Crit Care. 2 (1): 29–34. doi:10.1186/cc121. PMC 28999. PMID 11056707.
- ↑ Sheu CC, Gong MN, Zhai R, Chen F, Bajwa EK, Clardy PF; et al. (2010). "Clinical characteristics and outcomes of sepsis-related vs non-sepsis-related ARDS". Chest. 138 (3): 559–67. doi:10.1378/chest.09-2933. PMC 2940067. PMID 20507948.
- ↑ Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F; et al. (2003). "One-year outcomes in survivors of the acute respiratory distress syndrome". N Engl J Med. 348 (8): 683–93. doi:10.1056/NEJMoa022450. PMID 12594312.
- ↑ Linko R, Suojaranta-Ylinen R, Karlsson S, Ruokonen E, Varpula T, Pettilä V; et al. (2010). "One-year mortality, quality of life and predicted life-time cost-utility in critically ill patients with acute respiratory failure". Crit Care. 14 (2): R60. doi:10.1186/cc8957. PMC 2887181. PMID 20384998.
- ↑ Wang CY, Calfee CS, Paul DW, Janz DR, May AK, Zhuo H; et al. (2014). "One-year mortality and predictors of death among hospital survivors of acute respiratory distress syndrome". Intensive Care Med. 40 (3): 388–96. doi:10.1007/s00134-013-3186-3. PMC 3943651. PMID 24435201.
- ↑ Case courtesy of Associate Professor Frank Gaillard, M.D. "http://radiopaedia.org/cases/35985"
- ↑ Case courtesy of Dr. Sajoscha Sorrentino, M.D. "http://radiopaedia.org/cases/16290"
- ↑ "Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network". N Engl J Med. 342 (18): 1301–8. 2000. doi:10.1056/NEJM200005043421801. PMID 10793162.
- ↑ Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD; et al. (2010). "Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis". JAMA. 303 (9): 865–73. doi:10.1001/jama.2010.218. PMID 20197533.
- ↑ Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A; et al. (2010). "Neuromuscular blockers in early acute respiratory distress syndrome". N Engl J Med. 363 (12): 1107–16. doi:10.1056/NEJMoa1005372. PMID 20843245. Review in: Ann Intern Med. 2011 Jan 18;154(2):JC1-3
- ↑ NIH-NHLBI ARDS Clinical Network Mechanical Ventilation Protocol Summary. "http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf"
- ↑ NIH-NHLBI ARDS Clinical Network Mechanical Ventilation Protocol Summary. "http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf"
- ↑ Derdak S, Mehta S, Stewart TE, Smith T, Rogers M, Buchman TG; et al. (2002). "High-frequency oscillatory ventilation for acute respiratory distress syndrome in adults: a randomized, controlled trial". Am J Respir Crit Care Med. 166 (6): 801–8. doi:10.1164/rccm.2108052. PMID 12231488.
- ↑ Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P; et al. (2013). "High-frequency oscillation in early acute respiratory distress syndrome". N Engl J Med. 368 (9): 795–805. doi:10.1056/NEJMoa1215554. PMID 23339639.
- ↑ Daoud EG (2007). "Airway pressure release ventilation". Ann Thorac Med. 2 (4): 176–9. doi:10.4103/1817-1737.36556. PMC 2732103. PMID 19727373.
- ↑ Daoud EG, Farag HL, Chatburn RL (2012). "Airway pressure release ventilation: what do we know?". Respir Care. 57 (2): 282–92. doi:10.4187/respcare.01238. PMID 21762559.
- ↑ Gattinoni L, Pesenti A, Mascheroni D, Marcolin R, Fumagalli R, Rossi F; et al. (1986). "Low-frequency positive-pressure ventilation with extracorporeal CO2 removal in severe acute respiratory failure". JAMA. 256 (7): 881–6. PMID 3090285.
- ↑ Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM; et al. (2009). "Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial". Lancet. 374 (9698): 1351–63. doi:10.1016/S0140-6736(09)61069-2. PMID 19762075.
- ↑ Taylor RW, Zimmerman JL, Dellinger RP, Straube RC, Criner GJ, Davis K; et al. (2004). "Low-dose inhaled nitric oxide in patients with acute lung injury: a randomized controlled trial". JAMA. 291 (13): 1603–9. doi:10.1001/jama.291.13.1603. PMID 15069048.
- ↑ Adhikari NK, Dellinger RP, Lundin S, Payen D, Vallet B, Gerlach H; et al. (2014). "Inhaled nitric oxide does not reduce mortality in patients with acute respiratory distress syndrome regardless of severity: systematic review and meta-analysis". Crit Care Med. 42 (2): 404–12. doi:10.1097/CCM.0b013e3182a27909. PMID 24132038.
- ↑ Walmrath D, Schneider T, Schermuly R, Olschewski H, Grimminger F, Seeger W (1996). "Direct comparison of inhaled nitric oxide and aerosolized prostacyclin in acute respiratory distress syndrome". Am J Respir Crit Care Med. 153 (3): 991–6. doi:10.1164/ajrccm.153.3.8630585. PMID 8630585.
- ↑ Zwissler B, Kemming G, Habler O, Kleen M, Merkel M, Haller M; et al. (1996). "Inhaled prostacyclin (PGI2) versus inhaled nitric oxide in adult respiratory distress syndrome". Am J Respir Crit Care Med. 154 (6 Pt 1): 1671–7. doi:10.1164/ajrccm.154.6.8970353. PMID 8970353.