Acute coronary syndrome resident survival guide
Patient Presentation
Common presentation
- Substernal / precordial chest pressure / heaviness / pain
- Pain radiation to shoulder or arm / neck / jaw
- Nausea and/or vomiting
- Shortness of breath
- Diaphoresis
- Heartburn/ burning sensation in chest
- Dizziness
- Palpitations
- Near syncope / Syncope
Initial Evaluation and Orders
- Ensure patency of airway, check for adequate breathing and circulation.
- Vital signs (Pulse rate, blood pressure, respiratory rate, temperature, and oxygen saturation)
- 12-lead EKG (compare with old EKG if possible)
- Cardiac enzymes (three sets of troponin, CK, CK-MB at six hour intervals; first set may be normal, but order all three sets)
- Chest x-ray
- Oxygen (titrate for oxygen saturation levels >92%)
- IV access
- 325mg non-enteric coated aspirin by mouth (or per rectum if patient cannot take orally)
- If patient is not hypotensive and inferior myocardial infarction has been ruled out by EKG, give 0.4mg nitroglycerin sublingually up to three times, at 5 minute intervals, until chest pain improves.
- If pulmonary embolism is suspected D-dimers should be obtained.
| Important! |
|---|
| Follow up with all pending tests and lab results as soon as these become available. For information on evaluating the results go to the apppropriate section on this page. |
History and Symptoms
History of Present Illness:
- Chest pain history; ask about onset, duration, nature, intensity, location, progression, radiation (to arm, neck, jaw= acute coronary syndrome, or back=aortic dissection), aggravating (pleurtic and pericarditis chest pain worsens with respiration) and relieving factors (relieved by nitrates), constant or intermittent. Ask about any precipitating factors (trauma, physical strain, emotional distress).
- Ask if pain is associated with (head to toe). Headache, confusion, fever, photophobia, vision changes, bleeding, nausea, vomiting, apetite, weight loss, shortness of breath, palpitations, cough, sputum, abdominal pain, bowel symptoms, urinary symptoms.
Physical Examination
- General
- Check for alertness, and orientation with time, place, and person
- Patient leaning forward can point towards pericarditis
- HEENT:
- Auscultate carotid artery (check for bruit)
- Jugular venous distension, check for hepatojugular reflex
- Cardiovascular:
- Vital signs
- Pulse Rate (rate, rhythm. volume, quality, symmetry, all 4 limbs. Aortic dissection- Diminution or absence of pulses)
- Blood pressure (check for symmetry in all the limbs)
- Inspection: Check for displacement of the apex.
- Palpation: Confirm the findings of inspection (cardiac apex), musculo-skeletal tenderness, crepitus (esophageal rupture,subcutaneous emphysema), feel for any thrill (possible regurgitation), heave (right ventricular hypertrophy)
- Auscultation:
- Heart sounds (muffled in cardiac tamponade, Pericardial effusion), S3 and S4 (Heart failure)
- Murmur (commonly regurgitation murmur)
- Pericardial rub - (Pericarditis, commonly tricuspid area sounds like scratching), and gallop
- Vital signs
- Respiratory:
- Inspection: Observe for symmetry of chest movement, evidence of flail chest, tracheal deviation (pneumothorax).
- Palpation : Check for muscle tenderness, tracheal deviation, and chest wall movement.
- Percussion: Percuss all lung fields for dullness (effusion), or hyperresonance to percussion on the affected side (pneumothorax).
- Auscultation: Decreased breath sounds (effusion and tension pneumothorax), crackles (pleural effusion) rales (heart failure).
- Extremities: Check for pedal edema.
Differential Diagnosis
EKG Findings
Electrocardiogram in Unstable angina / NSTEMI
- No changes
- Non specific ST / T wave changes
- Flipped or inverted T waves
- ST Depression as shown below. Greater magnitudes of downsloping ST depression are associated with a poorer prognosis.
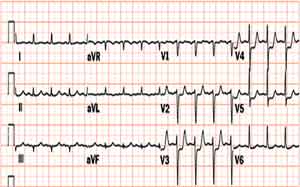
Electrocardiogram in STEMI
- ≥2 mm of ST segment elevation in 2 contiguous precordial leads
- ≥1mm in other leads (2 contiguous)
- An initial Q wave or abnormal R wave
- Additionally, new left bundle branch block and those with a true posterior MI are considered STEMI
- Specific types of STEMI:
- Anterior STEMI: ST elevation in the precordial leads + I and aVL (Left anterior descending artery)
- Posterior STEMI: ST elevations in II, III and aVF, reciprocal ST depressions in V1-V3, may have component of inferior ischemia (Left Circumflex artery)
- Inferior STEMI: ST elevation in II, III and aVF. When inferior MI is suspected a R - sided precordial leads is useful (ST elevation). Reciprocal changes in I and aVL (Right coronary artery or Left circumflex artery)
Chest X Ray Findings
- Aortic dissection: Suspect aortic dissection if findings include increased aortic diameter, widened mediastinum, and/or pleural effusion (hemothorax) in the absence of CHF
- Pulmonary embolism: May not appreciate any abnormalities on chest x ray.
- Tension pneumothorax: No pulmonary vessels are visible beyond the visceral pleural line. Tracheal deviation away from the collapsed area of lung will be seen.
- Esophageal rupture:The most common findings are pleural effusion, pneumothorax, pneumomediastinum, or subcutaneous emphysema.
- Heart failure: Cardiomegaly, and pulmonary congestion (Kerley B lines), may be seen. Obliteration of costophrenic angle may be seen in pleural effusion.
Other Diagnostic Work-up
- If esophageal rupture is suspected, a contrast-enhanced esophageal radiography is diagnostic.
- If pulmonary embolism is suspected, spiral CT scan should be obtained.
- If aortic dissection is suspected, obtain a CT scan with contrast.
- If cardiac tamponade is suspected, obtain an echocardiogram.