Abdominal aortic aneurysm overview
|
Abdominal Aortic Aneurysm Microchapters |
|
Differentiating Abdominal Aortic Aneurysm from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Abdominal aortic aneurysm overview On the Web |
|
Directions to Hospitals Treating Abdominal aortic aneurysm overview |
|
Risk calculators and risk factors for Abdominal aortic aneurysm overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Abdominal aortic aneurysm, also written as AAA and often pronounced 'triple-A', is a localized dilatation of the abdominal aorta, that exceeds the normal diameter of the abdominal aorta by more than 50%.
Historical Perspective
The etymology of the word aneurysm comes from the Greek word for "dilatation". Abdominal aortic aneurysm as a medical condition has been recognized since ancient times, but was not been successfully treated until the early part of the 20th century.
Definition
The normal diameter of one's aorta depends on the patient's age, sex, height, weight, race, body surface area, and baseline blood pressure. On average, the normal diameter of the infrarenal aorta (where abdominal aortic aneurysms are located) is 2 cm. Therefore an abdominal aortic aneurysm is defined as a dilation of 3.0 cm or more.
An abdominal aortic aneurysm is to be distinguished from aortic ectasia which is defined as a mild generalized dilatation (<50% of the normal diameter of ≤ 2.9 cm) that is due to age-related degenerative changes in vessel wall.
Anatomy
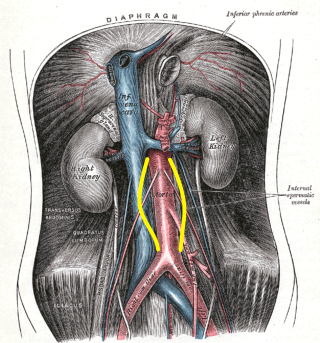
The aorta below the renal arteries, also known as the infrarenal aorta, is the location of 90% of abdominal aortic aneurysms. Other possible locations are suprarenal and pararenal. The aneurysm can extend to include one or both of the iliac arteries.
Classification
Aneurysms are usually classified by their shape:
Fusiform Aneurysms
- Most common type seen in the infrarenal aorta
- Diffuse, circumferential
Saccular Aneurysms
- Involve only a portion of the circumference, with a characteristic outpouching of the vessel wall.
Pathophysiology
The underlying pathophysiology of abdominal aortic aneurysm involves genetic influences, smoking, hypertension, hemodynamic influences and underlying atherosclerosis. In rare instances infection, arteritis, and connective tissue disorders may play a role.
Causes
Common contributors to the pathophysiology of abdominal aortic aneurysm include atherosclerosis, hypertension and smoking.
Differentiating Abdominal Aortic Aneurysm from other Disorders
An abdominal aortic aneurysm should be differentiated from other causes of abdominal pain such as acute cholecystitis.
Epidemiology and Demographics
Abdominal aortic aneurysm is the 13th leading cause of death in the US. Abdominal aortic aneurysms are more common in developed countries. Elderly, caucasian males who are smokers are at higher risk for developing an abdominal aortic aneurysm.
Risk Factors
Abdominal Aortic Aneurysm Development
The most significant modifiable risk factor for the development of an abdominal aortic aneurysm is smoking which increases the risk of aneurysm development 8 fold. Advanced age and family history are the strongest non-modifiable risk factors for the development of an abdominal aortic aneurysm. Hypercholesterolemia and hypertension are risk factors as well. Both diabetes mellitus and black race appear to be associated with a lower incidence of abdominal aortic aneurysm.
Abdominal Aortic Aneurysm Expansion
An increased rate of expansion of abdominal aortic aneurysm is related to systolic hypertension, wide pulse pressure, and ongoing smoking.
Abdominal Aortic Aneurysm Rupture
The risk of abdominal aortic aneurysm rupture is proportional to the size and rate of growth of the aneurysm. Abdominal aortic aneurysms greater than 5 cm diameter or those that grow faster than 1 cm per year have a significantly increased risk of rupture and are indications for elective operative repair. Advanced age, female gender, hypertension, active smoking, outpouchings, and mural thrombus are also risk factors for abdominal aortic aneurysm rupture.
Natural History
Abdominal aortic aneurysms expand slowly over time. It is for this reason ultrasound surveillance is recommended. If the rate of expansion exceeds 1 cm per year, this is an indication for surgery.
Complications
When an abdominal aortic aneurysm ruptures, it is a true medical emergency. Aortic dissection occurs when the innermost lining of the artery tears and blood leaks into the wall of the artery. This most commonly occurs in the aorta within the chest. Complications include:
- Acute aortic occlusion
- Aortocaval or aortoduodenal fistulae
- Arterial embolism
- Disseminated intravascular coagulation
- Heart attack
- Hypovolemic shock
- Kidney failure
- Stroke
Prognosis
Elective Surgery in the Absence of Abdominal Aortic Aneurysm Rupture
The outcome is usually good if an experienced surgeon repairs the aneurysm before it ruptures.
Emergency Surgery in the Setting of Abdominal Aortic Aneurysm Rupture
Rupture of an abdominal aortic aneurysm is associated with a 60% to 90% mortality before the patient reaches hospital. It is associated with a 30% to 80% operative mortality among those patients who survive long enough to undergo surgery.
Screening
Approximately 16% of large abdominal aortic aneurysms (diameter > 5.5 cm) rupture, causing 9,000 AAA-related deaths in the United States per year [1] Several studies have shown that screening can drastically reduce the aneurysm rupture rate by 45-49% for men older than 60, and reduce AAA-related mortality by 21-68%. In a landmark study randomizing 67,800 men, (The Multicenter Aneurysm Screening Study) aneurysm-related mortality was 53% lower in the screening group as compared with control patients.[2][3] The United States Preventive Services Task Force (USPSTF) recommends one-time screening for abdominal aortic aneurysm (AAA) by ultrasonography in any man aged 65 to 75 who has ever smoked. The USPSTF makes no recommendation for or against screening for AAA in men aged 65 to 75 who have never smoked. The USPSTF recommends against routine screening for AAA in women.
History
Given that smoking increases the risk of abdominal aortic aneurysm development, a smoking history should be obtained in elderly men. If a male over the age of 65 has a history of smoking, they should undergo ultrasonography to screen for an abdominal aortic aneurysm.
Symptoms
The vast majority of aneurysms are asymptomatic. Spontaneous abdominal pain in a patient with a pulsatile epigastric mass or a known AAA may signal rupture into the retroperitoneum or leakage within the aneurysm wall. If a patient does develop symptoms, the risk of rupture is quite high, which is why symptoms are considered an indication for surgery.
Possible symptoms include:
- Low back pain
- Flank pain
- Abdominal pain
- Groin pain
- Pulsating abdominal mass
- Peripheral embolization is rare with abdominal aortic aneurysms in contrast to popliteal artery aneurysms in which distal embolization is common.
Physical Examination
Physical examination has a low sensitivity in the detection of small abdominal aortic aneurysms (29-61% for abdominal aortic aneurysms 3.0-3.9 cm in diameter) but has a sensitivity of 76-82% to detect those abdominal aortic aneurysms that are 5.0 cm or larger that may warrant repair. It is easier to detect a pulsatile mass in thin patients and those who do not have tense abdomens. Contrary to popular belief, gentle palpation of abdominal aortic aneurysms is safe, and does not precipitate rupture.
Abdominal Ultrasound
Abdominal ultrasound is the imaging modality of choice to detect and follow the progression of an abdominal aortic aneurysm. It has a sensitivity that is close to 100%. Ultrasound also detects the presence of mural thrombus and iliac artery aneurysms. Patients should fast before examination to optimize image quality.
Abdominal X-Ray
Up to 50% of AAAs can be recognized on plain roentgenograms as a calcified aneurysmal wall.
Computed Tomography (CT)
Although CT scanning provides detailed anatomic information and is valuable in planning abdominal aortic aneurysm repair, it is not used as a screening tool given the potential nephrotoxicity associated with the dye load, the cost, and the exposure to radiation.
Magnetic Resonance Imaging (MRI)
Although MRI does not require nephrotoxic contrast, it is less accurate than thin-slice CT. It is also costly, and is not as readily available as contrast CT and ultrasonography.
Prevention
Smoking cessation and blood pressure management are two strategies to reverse modifiable risk factors for the development of, progression of, and rupture of an abdominal aortic aneurysm.
Medical Therapy
Risk factor modification including smoking cessation, management of hypertension, and lipid lowering are essential in reducing the risk of development and the rate of progression of abdominal aortic aneurysms.
Surgery
Indications for operative repair of an abdominal aortic aneurysm include the presence of symptoms such as back pain, the presence of a rupture or contained rupture, an abdominal aortic aneurysm diameter greater than 5.5 cm, a rate of expansion of greater than 1 cm in one year, and an inflammatory or infectious etiology. Open surgical repair is favored in young patients as an elective procedure, the presence of an expanding aneurysm, symptomatic aneurysm, or ruptured aneurysm. An endovascular repair (EVAR) is favored in older patients and high risk patients or those unfit for open repair. Risk factors for postoperative morbidity and mortality include extensive atheromatous disease, mural calcification, thrombosis, juxtarenal extension of the aneurysm and the presence of inflammatory changes.
References
- ↑ Gillum RF (1995). "Epidemiology of aortic aneurysm in the United States". Journal of Clinical Epidemiology. 48 (11): 1289–98. PMID 7490591. Retrieved 2012-10-27. Unknown parameter
|month=ignored (help) - ↑ Ashton HA, Buxton MJ, Day NE, Kim LG, Marteau TM, Scott RA, Thompson SG, Walker NM (2002). "The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial". Lancet. 360 (9345): 1531–9. PMID 12443589. Retrieved 2012-10-27. Unknown parameter
|month=ignored (help) - ↑ "Multicentre aneurysm screening study (MASS): cost effectiveness analysis of screening for abdominal aortic aneurysms based on four year results from randomised controlled trial". BMJ (Clinical Research Ed.). 325 (7373): 1135. 2002. PMC 133450. PMID 12433761. Retrieved 2012-10-27. Unknown parameter
|month=ignored (help)