AV nodal reentrant tachycardia
| AV nodal reentrant tachycardia | |
 | |
|---|---|
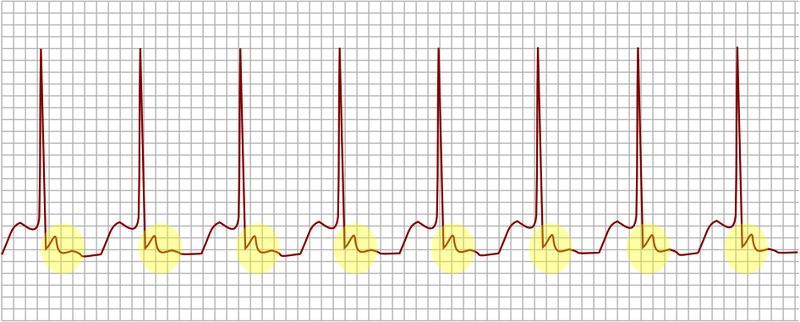
| AV nodal reentrant tachycardia. In yellow, is evidenced the P wave that falls after the QRS complex. | |
| ICD-10 | I47.1 |
| ICD-9 | 426.89, 427.0 |
| MeSH | D013611 |
|
AVNRT Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
AV nodal reentrant tachycardia On the Web |
|
American Roentgen Ray Society Images of AV nodal reentrant tachycardia |
|
Risk calculators and risk factors for AV nodal reentrant tachycardia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: AVNRT; AV node reentrant tachycardia; AV nodal reentry tachycardia; AV node reentry tachycardia; atrioventricular node reentrant tachycardia; atrioventricular nodal reentry tachycardia; atrioventricular node reentry tachycardia;
Overview
Historical Perspective
Pathophysiology
Classification
Risk Factors
Differentiating AVNRT from other Disorders
Epidemiology and Demographics
Natural History, Complications, Prognosis
Diagnosis
Symptoms | Physical Examination | Laboratory Findings | Electrocardiogram
Treatment
Overview | Patient position | Medical Therapy
Patient Position
Place the patient in a supine position to improve cerebral perfusion and reduce the odds of syncope. Placing the patient in Trendelenburg position may actually terminate the rhythm.
Vagal maneuvers
Some people with known AVNRT may be able to stop their attack by using various tricks to activate the vagus nerve. This includes carotid sinus massage (pressure on the carotid sinus in the neck), submersion of the face in ice water to trigger the diving reflex, putting the patient in Trendelenburg position or the Valsalva maneuver (increasing the pressure in the chest by attempting to exhale against a closed airway). Vagel maneuvers are contraindicated in the presence of hypotension.
Cardioversion
In very rare instances, cardioversion (the electrical restoration of a normal heart rhythm) is needed in the treatment of AVNRT. This would normally only happen if all other treatments have been ineffective, or if the fast heart rate is poorly tolerated (e.g. the development of heart failure symptoms, hypotension (low blood pressure) or unconsciousness).
Electrophysiology and Radiofrequency Ablation
After being diagnosed with AVNRT, patients can also undergo an electrophysiology (EP) study to confirm the diagnosis. Catheter ablation of the slow pathway, if successfully carried out, and cures 95% of patients with AVNRT. The risk of complications is quite low.
Prevention
Triggers such as alcohol and caffeine should be avoided.