AVNRT overview: Difference between revisions
No edit summary |
|||
| Line 27: | Line 27: | ||
===Premature Ventricular Complex=== | ===Premature Ventricular Complex=== | ||
The second most common mechanism whereby AVNRT is triggered is via the entry of a [[premature ventricular complex]] down either the slow conducting pathway (similar to a [[premature atrial complex]] above) or down the rapidly conducting pathway. | The second most common mechanism whereby AVNRT is triggered is via the entry of a [[premature ventricular complex]] down either the slow conducting pathway (similar to a [[premature atrial complex]] above) or down the rapidly conducting pathway. | ||
==Natural History, Complications, Prognosis== | |||
AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia and accounts for 60% to 70% of these cases. | |||
===Sex=== | |||
The ratio of female to male involvement is 3:1 | |||
===Age=== | |||
There is no age predilection. | |||
==Electrocardiogram== | ==Electrocardiogram== | ||
Revision as of 19:52, 9 September 2012
|
AVNRT Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
AVNRT overview On the Web |
|
American Roentgen Ray Society Images of AVNRT overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
AV nodal reentrant tachycardia is a type of tachycardia (fast rhythm) of the heart. It is one of several types of supraventricular tachycardia (SVT), and like all SVTs the electrical impulse originates proximal to the bundle of HIS. In the case of AVNRT, the electrical impulse originates in the AV node and the immediately surrounding tissue. AVNRT is the most common cause of supraventricular tachycardia.
Classification
There are several types of AVNRT. The "common form" or "usual" AVNRT utilizes the slow AV nodal pathway as the anterograde limb of the circuit and the fast AV nodal pathway as the retrograde limb. The reentry circuit can be reversed such that the fast AV nodal pathway is the anterograde limb and the slow AV nodal pathway is the retrograde limb. This, not surprisingly is referred to as the "uncommon form" of AVNRT. However, there is also a third type of AVNRT that utilizes the slow AV nodal pathway as the anterograde limb and left atrial fibers that approach the AV node from the left side of the inter-atrial septum as the retrograde limb. This is known as atypical, or Slow-Slow AVNRT.
Common AVNRT
In common AVNRT, the anterograde conduction is via the slow pathway and the retrograde conduction is via the fast pathway ("slow-fast" AVNRT). This accounts for 80%-90% of cases of AVNRT.
Because the retrograde conduction is via the fast pathway, stimulation of the atria (which produces the inverted P wave) will occur at the same time as stimulation of the ventricles (which causes the QRS complex). As a result, the inverted P waves may not be seen on the surface ECG since they are buried with the QRS complexes. Often the retrograde p-wave is visible, but also in continuity with the QRS complex, appearing as a "pseudo R prime" wave in lead V1 or a "pseudo S" wave in the inferior leads.
Uncommon AVNRT
In uncommon AVNRT, the anterograde conduction is via the fast pathway and the retrograde conduction is via the slow pathway ("fast-slow" AVNRT). Multiple slow pathways can exist so that both anterograde and retrograde conduction are over slow pathways. ("slow-slow" AVNRT).
Because the retrograde conduction is via the slow pathway, stimulation of the atria will be delayed by the slow conduction tissue and will typically produce an inverted P wave that falls after the QRS complex on the surface ECG.
AVNRT occurs when a reentry circuit forms within or just next to the atrioventricular node. The circuit usually involves two anatomical pathways: the fast pathway and the slow pathway, which are both in the right atrium. The slow pathway (which is usually targeted for ablation) is located inferiorly and slightly posterior to the AV node, often following the anterior margin of the coronary sinus. The fast pathway is usually located just superior and posterior to the AV node. These pathways are formed from tissue that behaves very much like the AV node, and some authors regard them as part of the AV node. In the usual form of AVNRT, the conduction from the atrium to the ventricle is down the slow pathway, and the retrograde conduction from the ventricle to the atrium is up the fast pathway.
Electrophysiologic Triggers
Premature Atrial Complex
The most common trigger for an episode of AVNRT is when an atrial premature complex (APC) approaches the fast pathway, and is blocked due to the longer refractory period of this pathway, and instead conducts down the slow pathway. As the impulse goes down the slow pathway, the fast pathway recovers, and allows the impulse to conduct backward or retrograde toward the atrium. It then re-enters the atrial entrance of the slow pathway and the cycle repeats itself.
Premature Ventricular Complex
The second most common mechanism whereby AVNRT is triggered is via the entry of a premature ventricular complex down either the slow conducting pathway (similar to a premature atrial complex above) or down the rapidly conducting pathway.
Natural History, Complications, Prognosis
AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia and accounts for 60% to 70% of these cases.
Sex
The ratio of female to male involvement is 3:1
Age
There is no age predilection.
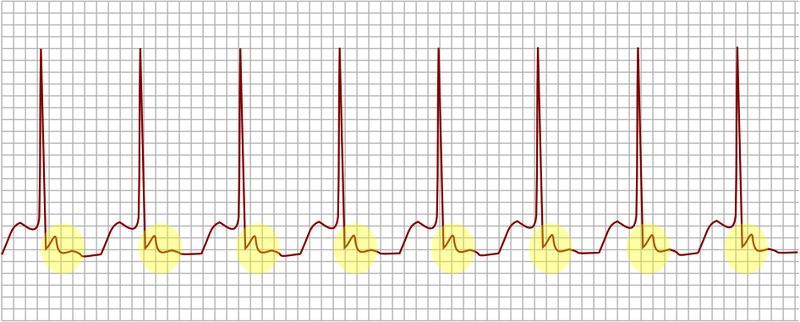
Electrocardiogram
An electrocardiogram performed during the occurrence of symptoms may confirm the diagnosis of AVNRT.
Slow-Fast AVNRT (Common AVNRT)
- This form of AVNRT accounts for 80% to 90% of cases of AVNRT.
- The retrograde P wave that is conducted retrograde up the fast pathway is usually burried within the QRS but less frequently may be observed at the end of the QRS complex as a pseudo r’ wave in lead V1 or an S wave in leads II, III or aVF.
Fast-Slow AVNRT (Uncommon AVNRT)
- This form of AVNRT Accounts for 10% of cases of AVNRT
- In this form of AVNRT, the impulse is first conducted antegrade down the Fast AV nodal pathway and is then conducted retrograde up the Slow AV nodal pathway.
- In contrast to Common AVNRT, a retrograde P wave may be observed after the QRS complex before the T wave
Slow-Slow AVNRT (Atypical AVNRT)
- This form of AVNRT accounts for 1-5% of cases of AVNRT
- In this form of AVNRT, the impulse is first conducted antegrade down the Slow AV nodal pathway and retrograde up the Slow left atrial fibres approaching the AV node.
- The p wave may appear just before the QRS complex, and this makes it hard to distinguish the rhythm from sinus tachycardia.
Aberrant Conduction
It is not uncommon for there to be a wide QRS complex due to aberrant conduction due to underlying conduction system disease. This can make it difficult to distinguish AVNRT from VT. The distinguishing features include:
- AVNRT is associated with a QRS complex morphology resembles a typical bundle branch block
- AVNRT is not associated with AV dissociation where there is variable coupling of the p wave and the QRS complex
- AVNRT is associated with Cannon a waves
- AVNRT is not associated with capture beats or fusion beats
- AVNRT may convert with adenosine or vagal maneuvers
An electrophysiologic study may be needed to confirm AVNRT prior to ablation.
Holter Monitor / Event Recorder
If the patient complains of recurrent palpitations and no arrhythmia is present on the resting EKG, then a Holter Monitor or Cardiac Event Monitor should be considered.