Alcoholic liver disease pathophysiology
|
Alcoholic liver disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Alcoholic liver disease pathophysiology On the Web |
|
American Roentgen Ray Society Images of Alcoholic liver disease pathophysiology |
|
Risk calculators and risk factors for Alcoholic liver disease pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
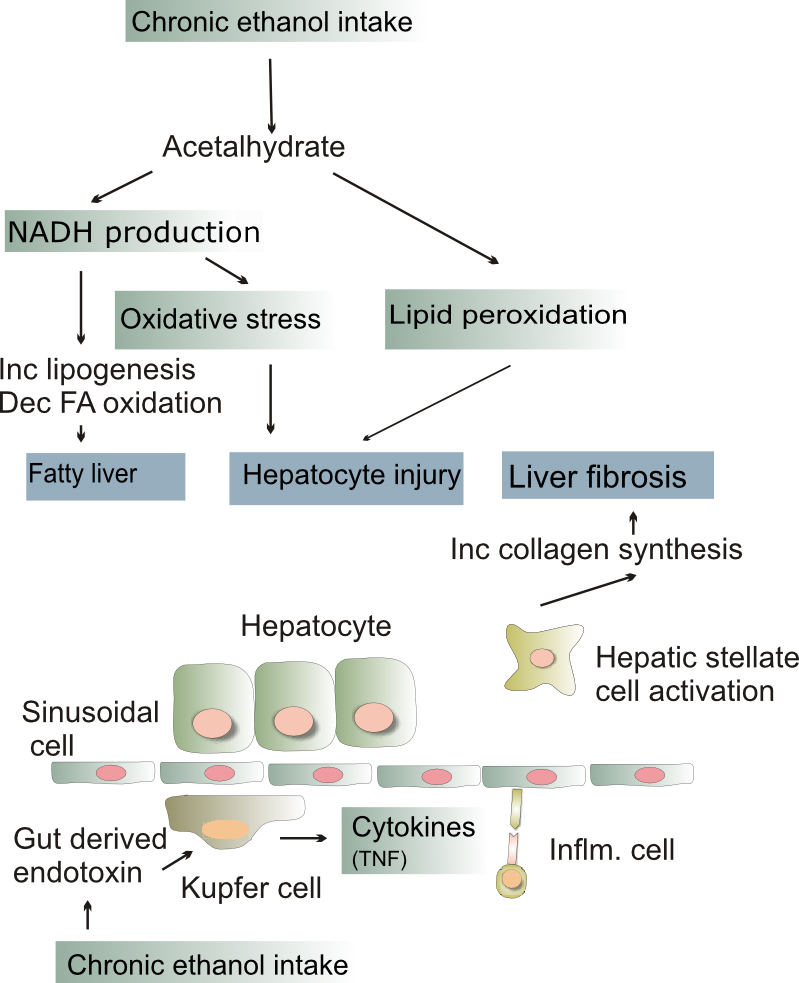
Alcoholic liver disease can vary in its level of severity. Fatty liver occurs by the excess generation of NAD by enzymes aldehyde dehydrogenase and alcohol dehydrogenase, leading to shunting of substrates into lipid biosynthesis. This can worsen into alcoholic hepatitis when inflammation, necrosis, and the generation of ROS occurs at the sites of fatty change. Cirrhosis is the final and irreversible stage of the progression of alcoholic liver disease, and is marked by fibrosis and disruption of liver architechture.
Pathophysiology
Alcoholic liver disease generally occurs after years of excessive drinking. The longer the alcohol use and the more alcohol that was consumed, the greater the likelihood of developing liver disease. Acute alcoholic hepatitis can result from binge drinking. It may be life-threatening if severe.
Persons who drink excessively can become malnourished due of the the lack of nutrients in alcohol, reduced appetite, and poor absorption (malabsorption) of nutrients in the intestines. Malnutrition contributes to the development of liver disease.
Other factors that contribute to the development of alcoholic liver disease are:
- Genetic factors
- Personal susceptibility to alcohol-induced liver disease
- Toxicity of alcohol (ethanol) to the liver
Alcoholic liver disease does not affect all heavy drinkers. Women may be more susceptible than men. It is not neccesary for a person to be a binge drinker for the disease to develop. Fatty change and alcoholic hepatitis are likely reversible. The later stages of fibrosis and cirrhosis tend to be irreversible but can usually be quite well managed for long periods of time.
Fatty change
- Fatty change, or steatosis is the accumulation of fat in liver cells which can be seen as fatty globules under the microscope.
- Alcoholism causes large fatty globules (macrovesicular steatosis).
- Other causes of macrovesicular steatosis include diabetes, obesity and starvation.
- Alcoholic fatty change is probably dose related.
- Small fatty globules have different causes.
Fatty change occurs at a microscopic level by:
- The excess generation of NAD by the enzymes alcohol dehydrogenase and aldehyde dehydrogenase which cause shunting of normal substrates from catabolism towards lipid biosynthesis.
- The impaired assembly and secretion of lipoproteins and increased peripheral lipid catabolism may also contribute
Alcoholic hepatitis
- Some people get an acute hepatitis or inflammatory reaction to the cells affected by fatty change. This is not directly related to the dose of alcohol.
- Some people seem more prone to this reaction than others. This is called alcoholic steatonecrosis and the inflammation probably predisposes to liver fibrosis.
Alcoholic hepatitis occurs at a microscopic level by:
- Acetaldehyde formed from alcohol inducing lipid peroxidation and acetaldehyde protein adduct formation which disrupt cytoskeleton
- Directly affecting the microtubule organization, mitochondrial function and membrane fluidity
- The generation of ROS
- Neutrophil attack at the site of hepatocyte necrosis
Liver fibrosis
- Liver fibrosis, in itself, is largely asymptomatic but as it progresses can turn into cirrhosis, where the fibrosis alters the architecture and impairs the function of the liver.
Cirrhosis
- Cirrhosis is a late stage of liver disease marked by fibrosis and altered liver architecture.
- It is often progressive and may eventually lead to liver failure.
- Late complications of cirrhosis or liver failure include portal hypertension, coagulation disorders, ascites and other complications including hepatic encephalopathy and the hepatorenal syndrome.
- Cirrhosis also has number of other causes, such as hepatitis and toxins. The late stages of cirrhosis (say from viral hepatitis or alcohol) may look similar. This phenomenon is termed a "final common pathway" for a disease.