Respiratory alkalosis
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
| Respiratory alkalosis | |
 | |
|---|---|
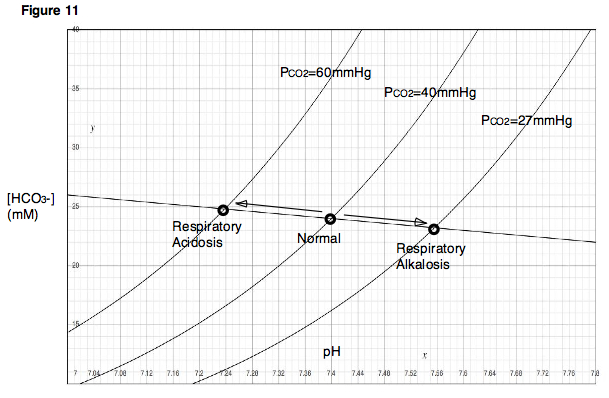
| Davenport diagram | |
| ICD-10 | E87.3 |
| ICD-9 | 276.3 |
| DiseasesDB | 406 |
| MedlinePlus | 000111 |
| eMedicine | med/2009 |
| MeSH | D000472 |
Respiratory alkalosis results from increased alveolar respiration (hyperventilation) leading to decreased plasma carbon dioxide concentration. This leads to decreased hydrogen ion and bicarbonate concentrations.
Types
There are two types of respiratory alkalosis: chronic and acute.
- In acute respiratory alkalosis, increased levels of carbon dioxide are "blown off" by the lungs, which are hyperventilating. During acute respiratory alkalosis, the person may lose consciousness where the rate of ventilation will resume to normal.
- In chronic respiratory alkalosis, for every 10 mM drop in pCO2 in blood, there is a corresponding 5 mM of bicarbonate ion drop. The drop of 5 mM of bicarbonate ion is a compensation effect which reduces the alkalosis effect of the drop in pCO2 in blood. This is termed metabolic compensation.
Causes
Causes of the alveolar hyperventilation seen in respiratory alkalosis include:
- anxiety, hysteria and stress
- moving into high altitude areas, when the low atmospheric pressure of oxygen stimulates increased ventilation
- pyrexia in fever, which stimulates the respiratory centre in the brainstem
- drugs, including doxapram and large doses of aspirin, which also stimulate the respiratory centre
- CNS causes, including stroke, subarachnoid haemorrhage, meningitis
- pregnancy
- a hypoxic drive in lung disease, such as pneumonia
- caffeine overdose and coffee abuse
In addition, a respiratory alkalosis is often produced accidentally by doctors (iatrogenically) during mechanical ventilation of patients.
Symptoms
Symptoms of respiratory alkalosis are related to the decreased blood carbon dioxide levels, and include peripheral paraesthesiae. In addition, the alkalosis may disrupt calcium ion balance, and cause the symptoms of hypocalcaemia (such as tetany) with no fall in total serum calcium levels.