Chronic cholecystitis pathophysiology
| https://https://www.youtube.com/watch?v=aU1lWPzUZgY%7C350}} |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Furqan M M. M.B.B.S[2] Aditya Govindavarjhulla, M.B.B.S. [3]
|
Chronic cholecystitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Chronic cholecystitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Chronic cholecystitis pathophysiology |
|
Risk calculators and risk factors for Chronic cholecystitis pathophysiology |
Overview
Inflammation of the gallbladder is termed as cholecystitis. Chronic calculous cholecystitis is usually caused by the mechanical obstruction due to gallstones. Chronic acalculous cholecystitis is caused predominantly by the gallbladder stasis. Lith gene is also involved in the pathogenesis of cholecystitis Cholecystitis is more common in siblings and first degree relatives of affected persons. On gross pathology, chronic cholecystitis usually shows enlarged/distended gallbladder and serosal or mucosal exudates. Fibrosis of gallbladder may also be seen. Microscopic pathology shows mononuclear inflammatory infiltrates and metaplasia and lipid/mucolipid accumulations in the gallbladder wall.
Pathophysiology
Pathogenesis
Inflammation of the gallbladder is termed as cholecystitis. Chronic calculous cholecystitis is usually caused by the mechanical obstruction due to gallstones. Chronic acalculous cholecystitis is caused predominantly by the gallbladder stasis. The pathogenesis of chronic cholecystitis involves the following:[1][2][3][4][5]
Gallbladder obstruction
- Gallstones are one of the major causes of cholecystitis. These cause physical obstruction to the lumen of the neck or cystic duct. This results in an increase in the intraluminal pressure. The degree and duration of obstruction are the two main factors that determine its progression.
- Partial obstruction of short duration may cause biliary colic. Long-term obstruction may progress to chronic cholecystitis.
- Some studies suggest that the pancreatic biliary reflux plays a role in the development of chronic cholecystitis.
Bile Stasis
Bile stasis results in acute acalculous cholecystitis but can also lead to chronic acalculous cholecystitis.
- Loss of fluids, opioid drugs, positive pressure ventilation, and other factors cause an increased concentration of bile in the biliary tract.
- Bile contains phosphatidyl choline, which in increased concentrations can cause mucosal disruption.
Genetics
- Cholecystitis is more common in siblings and first degree relatives of affected persons.[6][7]
- Lith gene is involved in the pathogenesis of cholecystitis.[8]
- Mutations in the hepatic cholesterol transporter ABCG8 also predispose an individual to the develop gallstones.[9]
Associated conditions
The following conditions are associated with gallstones:[10]
- Diabetes
- Insulin resistance
- Cardiovascular diseases
- Non-alcoholic fatty liver disease (NAFLD)
- Gastrointestinal malignancies:
Gross Pathology
- On gross pathology, chronic cholecystitis has the following features:[11][12][13]
- Enlarged/distended of gallbladder
- Serosal or mucosal exudates
- Thickened wall with hemorrhage and edema
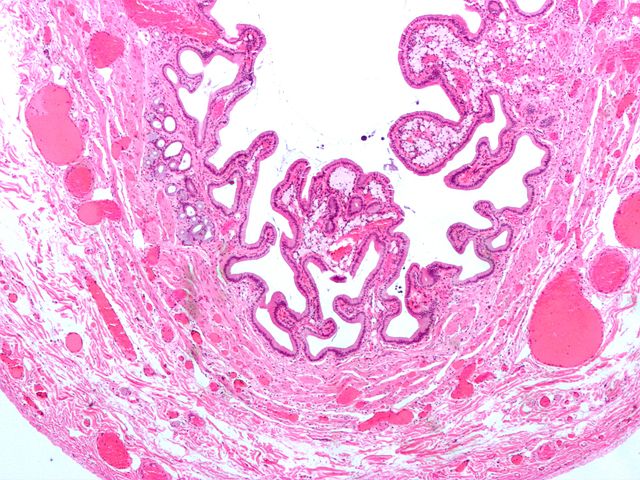
Microscopic Pathology
- On microscopic pathology, chronic cholecystitis has the following features:[13]
- Mononuclear inflammatory infiltrates and metaplasia
- Fibrosis
- Lipid and mucolipid acuumulation in gallbladder wall
{{#ev:youtube|gxGvP3GV_1E}}
|
References
- ↑ Kalloo AN, Kantsevoy SV (2001). "Gallstones and biliary disease". Prim. Care. 28 (3): 591–606, vii. PMID 11483446.
- ↑ Ahmed A, Cheung RC, Keeffe EB (2000). "Management of gallstones and their complications". Am Fam Physician. 61 (6): 1673–80, 1687–8. PMID 10750875.
- ↑ "Acute acalculous cholecystitis - Surgical Treatment - NCBI Bookshelf". Retrieved 2012-08-20.
- ↑ Amr AR, Hamdy HM, Nasr MM, Hedaya MS, Hassan AM (2012). "Effect of pancreatic biliary reflux as a cofactor in cholecystitis". Journal of the Egyptian Society of Parasitology. 42 (1): 121–8. PMID 22662601. Unknown parameter
|month=ignored (help);|access-date=requires|url=(help) - ↑ "The management of chronic cholecystitis - The American Journal of Surgery".
- ↑ "An Increased Familial Frequency of Gallstones - Gastroenterology".
- ↑ Weiss KM, Ferrell RE, Hanis CL, Styne PN (1984). "Genetics and epidemiology of gallbladder disease in New World native peoples". Am. J. Hum. Genet. 36 (6): 1259–78. PMC 1684666. PMID 6517051.
- ↑ Wang HH, Portincasa P, Afdhal NH, Wang DQ (2010). "Lith genes and genetic analysis of cholesterol gallstone formation". Gastroenterol. Clin. North Am. 39 (2): 185–207, vii–viii. doi:10.1016/j.gtc.2010.02.007. PMID 20478482.
- ↑ Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ (2016). "Gallstones". Nat Rev Dis Primers. 2: 16024. doi:10.1038/nrdp.2016.24. PMID 27121416.
- ↑ Tiderington E, Lee SP, Ko CW (2016). "Gallstones: new insights into an old story". F1000Res. 5. doi:10.12688/f1000research.8874.1. PMC 4962289. PMID 27508070.
- ↑ Huang SM, Yao CC, Pan H, Hsiao KM, Yu JK, Lai TJ, Huang SD (2010). "Pathophysiological significance of gallbladder volume changes in gallstone diseases". World J. Gastroenterol. 16 (34): 4341–7. PMC 2937116. PMID 20818819.
- ↑ Jones MW, Ferguson T. "Gallbladder, Cholecystitis, Acalculous". PMID 29083717.
- ↑ 13.0 13.1 "Chronic cholecystitis".
- ↑ "Acute cholecystitis - Libre Pathology".