Conjunctivitis pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Conjunctivitis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Conjunctivitis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Conjunctivitis pathophysiology |
|
Risk calculators and risk factors for Conjunctivitis pathophysiology |
Please help WikiDoc by adding more content here. It's easy! Click here to learn about editing.
Pathophysiology
Infective Conjunctivitis is spread from:
- Direct contact with the infected person’s eye drainage or drainage from the person’s cough, sneeze, or runny nose
- Contact with the infected person’s fingers, hands or objects that may have the infected person’s drainage on them (e.g. eye makeup applicators, towels, shared eye medications)
- Adjacent infectious sites (rubbing of the eyes)
Any change in the host defense or in the species of normal flora of the eye (such as streptococci, staphylococci, and corynebacteria) can lead to clinical infection and Conjunctivitis.[1] Change in the flora can occur by:
- External contamination
- Contact lens wear
- Swimming
Newborns can be infected by bacteria in the birth canal. This condition is called ophthalmia neonatorum, and it must be treated immediately to preserve eyesight. Additionally, neonatal conjunctivitis is a red eye in a newborn caused by irritation, a blocked tear duct, or infection.
Development of Allergic Conjunctivitis is result of type I hypersensitivity reactions involving the conjunctiva. IgE-mediated and Mast cell plays an important role in these allergic inflammations.[2]Combination of type I and type IV hypersensitivity reactions may be responsible for the pathogenesis of Giant papillary conjunctivitis. It is believed that an antigen is present, in predisposed individuals, which stimulates the immunological reaction.Prolonged mechanical irritation to the superior tarsal conjunctiva, of the upper lid, from any of a variety of foreign bodies may also be a contributing factor in Giant papillary conjunctivitis. [3][4] Airborne antigens may be involved in the pathogenesis of Allergic Conjunctivitis. Common airborne antigens, include:[5][6]
- Pollen,
- Grass,
- Weeds,
There is a strong association with atopic dermatitis and Allergic Conjunctivitis.
Microscopic Pathology
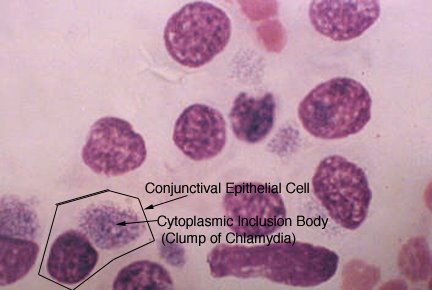
infective Conjunctivitis
The surface tissues of the eye are colonized by normal flora such as streptococci, staphylococci, and corynebacteria. Any change in the host defense or in the species of bacteria can lead to clinical infection. Any change in the flora can also occur by external contamination (contact lens wear, swimming) or spread from adjacent infectious sites (rubbing of the eyes).[1]
The primary defense against infection is the epithelial layer covering the conjunctiva. Secondary defenses include hematologic immune mechanisms carried by the conjunctival vasculature; tear film immunoglobulins and lysozyme; and the rinsing action of lacrimation and blinking. Disruption of any of these defenses mechanisms can lead to infection.[8]
Allergic Conjunctivitis
Development of Allergic Conjunctivitis is result of type I hypersensitivity reactions involving the conjunctiva. Allergic conjunctivitis is prompted by IgE-mediated immediate hypersensitivity reaction. Mast cell play an important role in these allergic inflammations.[2] Airborne antigens may be involved in the pathogenesis of Allergic Conjunctivitis. Common airborne antigens, include pollen, grass, and weeds, may provoke the symptoms of acute Allergic Conjunctivitis, and also there is a strong association with atopic dermatitis and Allergic Conjunctivitis.[5][6] Combination of type I and type IV hypersensitivity reactions may be responsible for the pathogenesis of Giant papillary conjunctivitis. It is believed that an antigen is present, in predisposed individuals, which stimulates the immunological reaction.Prolonged mechanical irritation to the superior tarsal conjunctiva, of the upper lid, from any of a variety of foreign bodies may also be a contributing factor in Giant papillary conjunctivitis. [3][4]
Keratoconjunctivitis
References
- ↑ 1.0 1.1 Everitt H, Kumar S, Little P (2003). "A qualitative study of patients' perceptions of acute infective conjunctivitis". Br J Gen Pract. 53 (486): 36–41. PMC 1314490. PMID 12564275.
- ↑ 2.0 2.1 Kyei S, Koffuor GA, Ramkissoon P, Abokyi S, Owusu-Afriyie O, Wiredu EA (2015). "Possible Mechanism of Action of the Antiallergic Effect of an Aqueous Extract of Heliotropium indicum L. in Ovalbumin-Induced Allergic Conjunctivitis". J Allergy (Cairo). 2015: 245370. doi:10.1155/2015/245370. PMC 4657065. PMID 26681960.
- ↑ 3.0 3.1 Donshik PC (1994). "Giant papillary conjunctivitis". Trans Am Ophthalmol Soc. 92: 687–744. PMC 1298525. PMID 7886881.
- ↑ 4.0 4.1 Donshik PC, Porazinski AD (1999). "Giant papillary conjunctivitis in frequent-replacement contact lens wearers: a retrospective study". Trans Am Ophthalmol Soc. 97: 205–16, discussion 216-20. PMC 1298261. PMID 10703125.
- ↑ 5.0 5.1 Malling HJ, Montagut A, Melac M, Patriarca G, Panzner P, Seberova E; et al. (2009). "Efficacy and safety of 5-grass pollen sublingual immunotherapy tablets in patients with different clinical profiles of allergic rhinoconjunctivitis". Clin Exp Allergy. 39 (3): 387–93. doi:10.1111/j.1365-2222.2008.03152.x. PMC 4233960. PMID 19134019.
- ↑ 6.0 6.1 Kämpe M, Stålenheim G, Janson C, Stolt I, Carlson M (2007). "Systemic and local eosinophil inflammation during the birch pollen season in allergic patients with predominant rhinitis or asthma". Clin Mol Allergy. 5: 4. doi:10.1186/1476-7961-5-4. PMC 2174506. PMID 17967188.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ Hutnik C, Mohammad-Shahi MH (2010). "Bacterial conjunctivitis". Clin Ophthalmol. 4: 1451–7. doi:10.2147/OPTH.S10162. PMC 3000772. PMID 21188158.
- ↑ Zhang X, Zhao L, Deng S, Sun X, Wang N (2016). "Dry Eye Syndrome in Patients with Diabetes Mellitus: Prevalence, Etiology, and Clinical Characteristics". J Ophthalmol. 2016: 8201053. doi:10.1155/2016/8201053. PMC 4861815. PMID 27213053.