Thymoma overview
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma overview On the Web |
|
American Roentgen Ray Society Images of Thymoma overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2]
Overview
Thymoma is one of the organs contained in the anterior mediastinum, located behind the sternum in front of the great vessels that involutes during puberty, but continues to take part in lymphocytes maturation throughout adulthood. Thymic malignancies count for less than 0.13/100,000/year.
They can be divided into two major groups: thymoma and thymic carcinoma. Prognosis and proper management are essentially determined by pathologic classification. Surgery is the only curative treatment, but they can be sensitive to chemotherapy and radiotherapy especially in unresectable disease.
Thymoma is the most common tumor of the anterior mediastinum, consisting of any type of thymic epithelial cell as well as lymphocytes that are usually abundant and probably not neoplastic. Thymoma usually is benign, and frequently encapsulated uncommon tumor, best known for its association with the neuromuscular disorder myasthenia gravis. Thymoma is found in 15% of patients with myasthenia gravis. Once diagnosed, thymomas may be removed surgically. When occasionally malignant, then it is invasive: metastasis is extremely rare. In the rare case of a malignant tumor, chemotherapy may be used.
Malignant lymphomas that involve the thymus, e.g., lymphosarcoma, Hodgkin's disease (termed "granulomatous thymoma" in the past), should not be regarded as thymoma.[1]
Thymomas associated with autoimmune disorders usually are benign. Malignant thymomas can metastasize, generally to pleura, kidney, bone, liver or brain.[2]
-
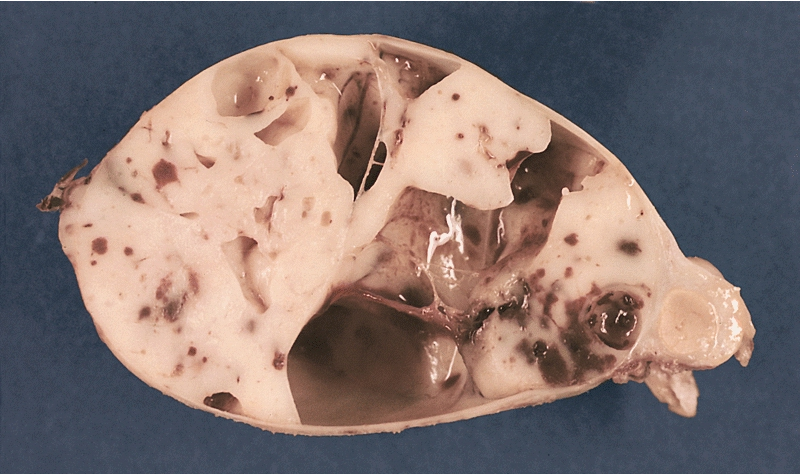
MEDIASTINUM: ENCAPSULATED CYSTIC THYMOMA. Post-formalin-fixed cut surface reveals an ivory-colored tumor with multiple cystic spaces varying from pin-head sized to a few centimeters in diameter. Small hemorrhages are also noted
References
- ↑ Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". J. Clin. Oncol. 17 (7): 2280–9. PMID 10561285.
- ↑ Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 17 (7): 2280–9. PMID 10561285. Retrieved 2012-01-18. Unknown parameter
|month=ignored (help)