Cervical cancer pathophysiology
|
Cervical cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cervical cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cervical cancer pathophysiology |
|
Risk calculators and risk factors for Cervical cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]}Associate Editor(s)-in-Chief: Nima Nasiri, M.D.[2]Monalisa Dmello, M.B,B.S., M.D. [3] Aida Javanbakht, M.D.
Overview
It is established that human papillomavirus (HPV) is the main cause of development of cervical neoplasia, only high risk strain of HPV can cause cervical cancer among women whom are affected. This is because of HPV produced proteins E7 which alters epithelium of cervix mainly at junctional zone.
Pathophysiology
Pathogenesis:
Role of high risk strains of HPV, mainly HPV types 16 and 18 had been identified as a potent cause of cancer of cervix, but there are other cofactors that cause progression of cervical neoplasia, some of these include:[1][2]
- HLA type
- Immunosuppression, since response to HPV infection is cell mediated.
- Sex steroid hormons
- Smoking which disrupts immune response.
- Co-infection with herpse simplex virus type 2, cytomegalovirus (CMV), human herpesvirus 6 (HHV-6), and HHV-7, which cause promotion of infection with HPV and plays an initiation role.
Role of HPV in pathogenesis of cervical cancer widely related to dirupting cell cycle growth and regulations, summary of these include:[3]
- The high risk HPV E6 and E7 gene products which are involved in viral replication and oncogenesis bind to p53 and prevents its normal activities which is G1 arrest, apoptosis, and DNA repair.
- HPV enters the host cell which are squamous cells of epithelium in cervix, mainly in junctional zone and viral transcription and replication begins.
Genetic:
- L-1β, encoded by the IL-1B gene, is an inflammatory cytokine and part of the innate immune system.[4]
- TNF-α, encoded by the TNFA gene, is another potent pro-inflammatory cytokine that has been implicated in the control of HPV infection.
- Polymorphisms within HLA plays a role in pathogenesis of cervical neoplasia.
- Interleukin-12 A and B gene (IL12A and IL12B)
- IFN-γ, encoded by the IFNG gene has defensive role against viruses and induces immune mediated inflammatory responses
- Interleukin-10 and the risk and the progression of cervical cancer have been associated with increased IL-10 serum levels
- Cytotoxic T-lymphocyte antigen-4
- HPV E6/E7 oncogenes, proteins that interfere with cell cycle growth and tumor supressor genes.
- Primary microRNA-218 (pri-miR-218) and laminin-5 β3 (LAMB3)
Associated Conditions:
Gross Pathology:
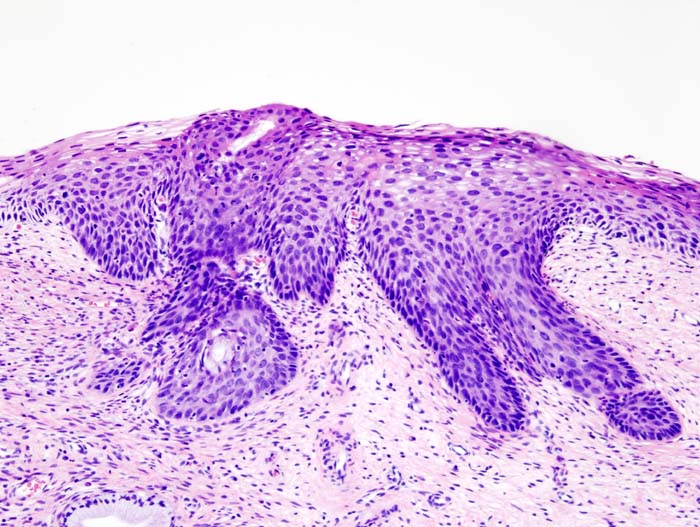
Microscopic pathology
- Prominent nucleoli.
- Blurred or scalloped epithelial-stromal interface.
- Loss of nuclear polarity.
- Pseudoglandular pattern because of acantholysis and central necrosis.
-
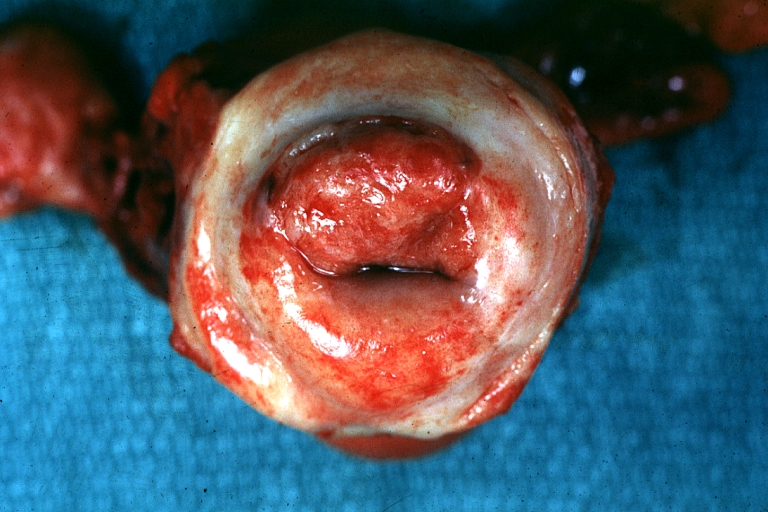
Uterus: Cervical Carcinoma: Gross, an excellent example of tumor (labeled as invasive)
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology -
Histopathologic image (H&E stain) of cervical intraepithelial neoplasia.
Video
{{#ev:youtube|J3kULzKGzws}}
References
- ↑ Arends MJ, Buckley CH, Wells M (February 1998). "Aetiology, pathogenesis, and pathology of cervical neoplasia". J. Clin. Pathol. 51 (2): 96–103. PMID 9602680.
- ↑ zur Hausen H (December 1982). "Human genital cancer: synergism between two virus infections or synergism between a virus infection and initiating events?". Lancet. 2 (8312): 1370–2. PMID 6129466.
- ↑ Burd EM (January 2003). "Human papillomavirus and cervical cancer". Clin. Microbiol. Rev. 16 (1): 1–17. PMC 145302. PMID 12525422.
- ↑ . doi:10.1016/S1674-8301(11)60020-1. Check
|doi=value (help). Missing or empty|title=(help)