Eosinophilic pneumonia pathophysiology
|
Eosinophilic pneumonia Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Eosinophilic pneumonia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Eosinophilic pneumonia pathophysiology |
|
Risk calculators and risk factors for Eosinophilic pneumonia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Priyamvada Singh, M.D. [2]
Overview
Pathophysiology
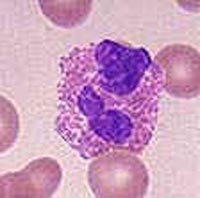
Eosinophilic pneumonia can develop in several different ways depending on the underlying cause of the disease. Eosinophils are thought to play a central role in defending the body against infection by parasites. Many diseases, such as asthma and eczema, are caused when eosinophils overreact to environmental triggers and release an excess of chemicals (cytokines) such as histamine. The common characteristic among different causes of EP is eosinophil overreaction or dysfunction in the lung.
Medications and environmental exposures
Medications, drugs of abuse, and environmental exposures may all trigger eosinophil dysfunction. Medications such NSAIDs (ie ibuprofen), nitrofurantoin, phenytoin, L-tryptophan, and ampicillin and drugs of abuse such as inhaled heroin and cocaine may trigger an allergic response which results in EP. Chemicals such as sulfites, aluminum silicate, and cigarette smoke can cause EP when inhaled. A New York City firefighter developed EP after inhalation of dust from the World Trade Center on September 11, 2001.[3]
Parasitic infections
Parasites cause EP in three different ways. Parasites can either invade the lung, live in the lung as part of their life cycle, or be spread to the lung by the bloodstream. Eosinophils migrate to the lung in order to fight the parasites and EP results. Important parasites which invade the lung include Paragonimus lung flukes and the tapeworms Echinococcus and Taenia solium. Important parasites which inhabit the lung as part of their normal life cycle include the worms (helminths) Ascaris lumbricoides, Strongyloides stercoralis and the hookworms Ancylostoma duodenale and Necator americanus. When EP is caused by this last group, it is often called "Löffler's syndrome". The final group of parasites cause EP when a large number of eggs are carried into the lungs by the bloodstream. This can include Trichinella spiralis, Strongyloides stercoralis, Ascaris lumbricoides, the hookworms, and the schistosomes.[4]
AEP and CEP
The causes for both AEP and CEP are unknown as of 2005. There is some suspicion that at least AEP is the result of the body's response to some unidentified environmental agent.