Arrhythmogenic right ventricular dysplasia pathophysiology
|
Arrhythmogenic right ventricular dysplasia Microchapters |
|
Differentiating Arrhythmogenic right ventricular dysplasia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Arrhythmogenic right ventricular dysplasia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Arrhythmogenic right ventricular dysplasia pathophysiology |
|
FDA on Arrhythmogenic right ventricular dysplasia pathophysiology |
|
CDC on Arrhythmogenic right ventricular dysplasia pathophysiology |
|
Arrhythmogenic right ventricular dysplasia pathophysiology in the news |
|
Blogs onArrhythmogenic right ventricular dysplasia pathophysiology |
|
Directions to Hospitals Treating Arrhythmogenic right ventricular dysplasia |
|
Risk calculators and risk factors for Arrhythmogenic right ventricular dysplasia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The pathogenesis of ARVD involves apoptosis with fatty and fibro-fatty infiltration of the right ventricular free wall leading to heart failure and ventricular arrhythmias.
Pathophysiology
There are two pathological patterns seen in ARVD, fatty infiltration and fibro-fatty infiltration.
Apoptosis
Apoptosis (programmed cell death) appears to play a role in the pathogenesis of ARVD and high levels of apopain have been observed.[1] It is unclear why only the right ventricle is involved. The disease process starts in the subepicardial region and works its way towards the endocardial surface, leading to transmural involvement (possibly accounting for the aneurysmal dilatation of the RV). The presence of residual myocardium is confined to the subendocardial region and the trabeculae of the RV. These trabeculae may become hypertrophied.
Aneurysmal Dilation of the Right Ventricle
Aneurysmal dilatation of the right ventricle is observed in 50% of cases at autopsy. It usually occurs in the diaphragmatic, apical, and infundibular regions (known as the triangle of dysplasia).
Left Ventricular Involvement
The left ventricle is involved in 50-67% of individuals. If the left ventricle is involved, it is usually late in the course of disease, and confers a poor prognosis.
Fatty infiltration
The first, fatty infiltration, is confined to the right ventricle. This involves a partial or near-complete substitution of myocardium with fatty tissue without wall thinning. It involves predominantly the apical and infundibular regions of the RV. The left ventricle and ventricular septum are usually spared. No inflammatory infiltrates are seen in fatty infiltration. There is evidence of myocyte (myocardial cell) degeneration and death seen in 50% of cases of fatty infiltration.
Fibro-fatty infiltration
The second, fibro-fatty infiltration, involves replacement of myocytes with fibro-fatty tissue. A patchy myocarditis is observed in up to 2/3 of cases, with inflammatory infiltrates (mostly T cells) seen on microscopy. Myocardial atrophy is due to injury and apoptosis. This leads to thinning of the RV free wall (to < 3 mm thickness). The regions preferentially involved include the RV inflow tract, the RV outflow tract, and the RV apex. However, the LV free wall may be involved in some cases. Involvement of the ventricular septum is rare. The areas involved are prone to aneurysm formation.
Genetics
There is an autosomal dominant pattern of inheritance..
ARVD1
This variant is due to a heterozygous mutation in the TGFB3 gene (190230) on chromosome 14q24.[2]
ARVD2
This variant (600996) is associated with a mutation in the RYR2 gene (180902) on chromosome 1q42-q43.[3]
ARVD3
This variant (602086) is associated with a mutation in the chromosome 14q12-q22 region.[4]
ARVD4
This variant (602087) is associated with a mutation in the chromosome 2q32.1-q32.3 region.[5]
ARVD5
This variant (604400) is associated with a mutation in the TMEM43 gene (612048) on chromosome 3p23 region.[6]
ARVD6
This variant (604401), is associated with a mutation in the chromosome 10p14-p12 region.[7]
ARVD7
This variant 609160) is associated with a mutation in the chromosome 10q22.3 region.[8]
ARVD8
This variant 607450) is associated with a mutation in the DSP gene (125647) on chromosome 6p24.<ref.Rampazzo A, Nava A, Malacrida S et-al. Mutation in human desmoplakin domain binding to plakoglobin causes a dominant form of arrhythmogenic right ventricular cardiomyopathy. Am. J. Hum. Genet. 2002;71 (5): 1200-6. doi:10.1086/344208 - Free text at pubmed - Pubmed citation</ref>
ARVD9
This variant (609040) is associated with a mutation in the PKP2 gene (602861) on chromosome 12p11.
ARVD10
This variant (610193) is associated with a mutation in the DSG2 gene (125671) on chromosome 18q12.1-q12.
ARVD11
This variant (610476) is associated with a mutation in the DSC2 gene (125645) on chromosome 18q12.1.
ARVD12
This variant (611528) is associated with a mutation in the JUP gene (173325) on chromosome 17q21.
Ventricular arrhythmias
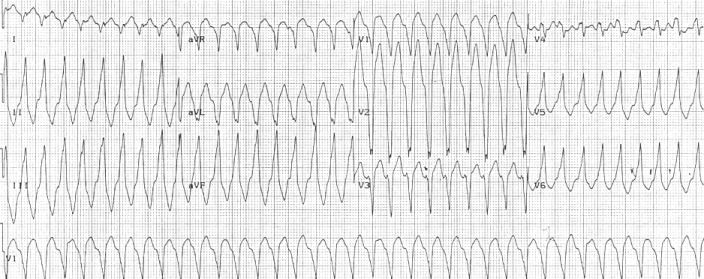 Right ventricular outflow tract tachycardia |
| Monomorphic ventricular tachycardia originating from the right ventricular outflow tract. |
Ventricular arrhythmias due to ARVD typically arise from the diseased right ventricle. The type of arrhythmia ranges from frequent premature ventricular complexes (PVCs) to ventricular tachycardia (VT) to ventricular fibrillation (VF).
While the initiating factor of the ventricular arrhythmias is unclear, it may be due to triggered activity or reentry.
Ventricular arrhythmias are usually exercise-related, suggesting that they are sensitive to catecholamines. The ventricular beats typically have a right axis deviation. Multiple morphologies of ventricular tachycardia may be present in the same individual, suggesting multiple arrhythmogenic foci or pathways.
Right ventricular outflow tract (RVOT) tachycardia is the most common VT seen in individuals with ARVD. In this case, the EKG shows a left bundle branch block (LBBB) morphology with an inferior axis.
References
- ↑ Mallat Z, Tedgui A, Fontaliran F et-al. Evidence of apoptosis in arrhythmogenic right ventricular dysplasia. N. Engl. J. Med. 1996;335 (16): 1190-6. doi:10.1056/NEJM199610173351604 - Pubmed citation
- ↑ Basso C, Corrado D, Marcus FI et-al. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373 (9671): 1289-300. doi:10.1016/S0140-6736%2809%2960256-7 - Pubmed citation
- ↑ Rampazzo A, Nava A, Erne P et-al. A new locus for arrhythmogenic right ventricular cardiomyopathy (ARVD2) maps to chromosome 1q42-q43. Hum. Mol. Genet. 1995;4 (11): 2151-4. Hum. Mol. Genet. (link) - Pubmed citation
- ↑ Severini GM, Krajinovic M, Pinamonti B et-al. A new locus for arrhythmogenic right ventricular dysplasia on the long arm of chromosome 14. Genomics. 1996;31 (2): 193-200. Genomics (link) - Pubmed citation
- ↑ Rampazzo A, Nava A, Miorin M et-al. ARVD4, a new locus for arrhythmogenic right ventricular cardiomyopathy, maps to chromosome 2 long arm. Genomics. 1997;45 (2): 259-63. doi:10.1006/geno.1997.4927 - Pubmed citation
- ↑ Ahmad F, Li D, Karibe A et-al. Localization of a gene responsible for arrhythmogenic right ventricular dysplasia to chromosome 3p23. Circulation. 98 (25): 2791-5. Circulation (link) - Pubmed citation
- ↑ Li D, Ahmad F, Gardner MJ et-al. The locus of a novel gene responsible for arrhythmogenic right-ventricular dysplasia characterized by early onset and high penetrance maps to chromosome 10p12-p14. Am. J. Hum. Genet. 2000;66 (1): 148-56. doi:10.1086/302713 - Free text at pubmed - Pubmed citation
- ↑ Kuhl A, Melberg A, Meinl E et-al. Myofibrillar myopathy with arrhythmogenic right ventricular cardiomyopathy 7: corroboration and narrowing of the critical region on 10q22.3. Eur. J. Hum. Genet. 2008;16 (3): 367-73. doi:10.1038/sj.ejhg.5201980 - Pubmed citation