Cryptosporidiosis pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Cryptosporidiosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cryptosporidiosis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cryptosporidiosis pathophysiology |
|
Risk calculators and risk factors for Cryptosporidiosis pathophysiology |
Overview
Infectious agents
A number of species of Cryptosporidium infect mammals. In humans the main causes of disease are C. parvum and C. hominis (previously C. parvum genotype 1). C. canis, C. felis, C. meleagridis, and C. muris can also cause disease in humans.
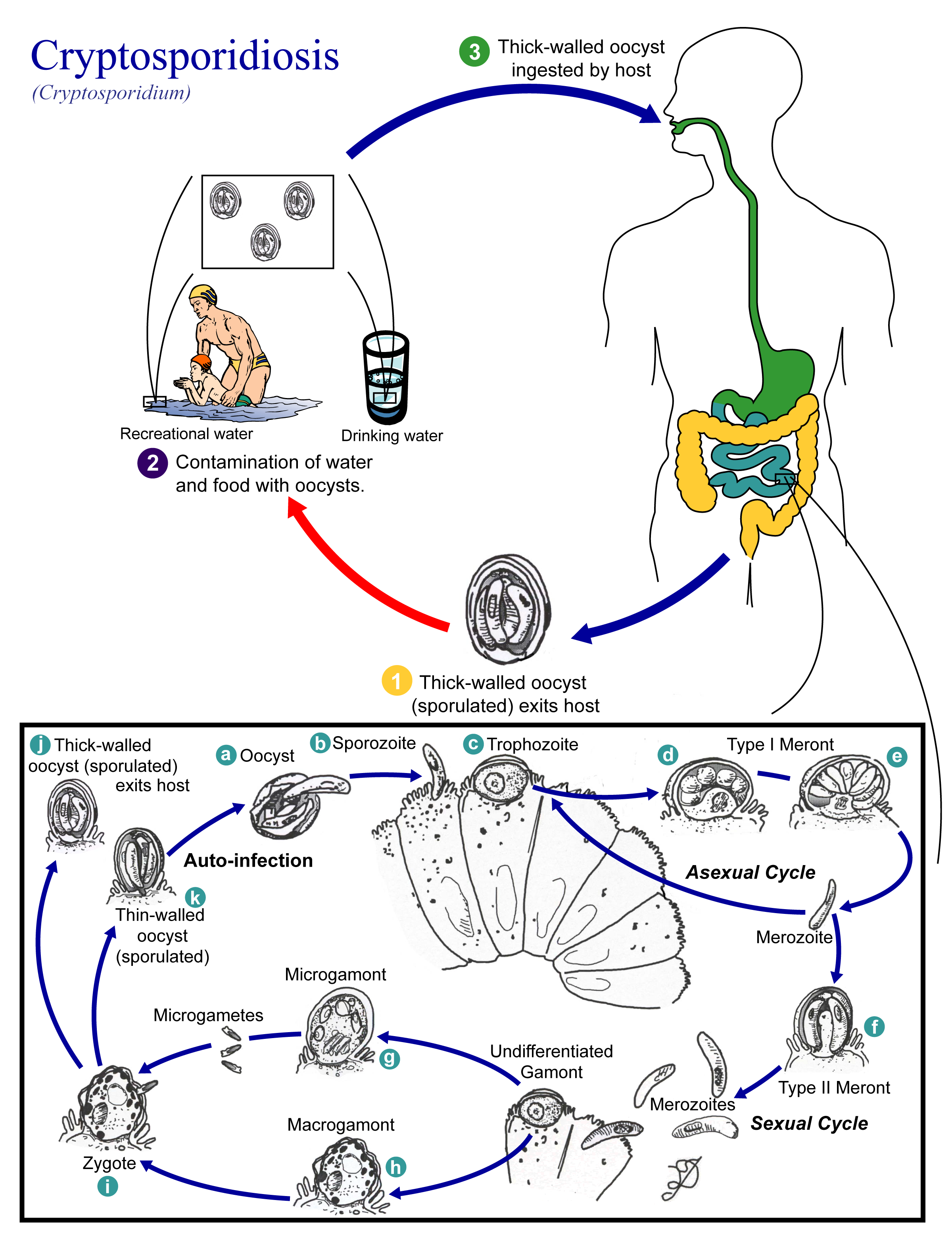
Life cycle
Cryptosporidium has a spore phase (oocyst) and in this state it can survive for lengthy periods outside a host. It can also resist many common disinfectants, notably chlorine-based disinfectants.[1]
The life cycle of Cryptosporidium parvum consists of an asexual stage and a sexual stage.[2] After being ingested, the oocysts excyst in the small intestine. They release sporozoites that attach to the microvilli of the epithelial cells of the small intestine. From there they become trophozoites that reproduce asexually by multiple fission, a process known as schizogony. The trophozoites develop into Type 1 meronts [1] that contain 8 daughter cells.[3] These daughter cells are Type 1 merozoites, which get released by the meronts. Some of these merozoites can cause autoinfection by attaching to epithelial cells. Others of these merozoites become Type II meronts,[4] which contain 4 Type II merozoites.[3] These merozoites get released and they attach to the epithelial cells. From there they become either macrogamonts or microgamonts.[4] These are the female and male sexual forms, respectively.[3] This stage, when sexual forms arise, is called gametogony.[5] Zygotes are formed by microgametes from the microgamont penetrating the macrogamonts. The zygotes develop into oocysts of two types.[4] 20% of oocysts have thin walls and so can reinfect the host by rupturing and releasing sporozoites that start the process over again.[3] The thick-walled oocysts are excreted into the environment.[4] The oocysts are mature and infective upon being excreted.[3] They can survive in the environment for months.[6]
References
- ↑ "Chlorine Disinfection of Recreational Water for Cryptosporidium parvum". CDC. Retrieved 6 May 2007.
- ↑
- ↑ 3.0 3.1 3.2 3.3 3.4
- ↑ 4.0 4.1 4.2 4.3
- ↑ Murray, Patrick R., Ken S. Rosenthal, and Michael A. Pfaller. Medical Microbiology. 5th ed. Philadelphia: Elsevier Inc., 2005: 855-856.
- ↑ "Cryptosporidiosis". Gideon. 23 February 2009.
Trial subscription required to access