Sandbox/01
|
WikiDoc Resources for Sandbox/01 |
|
Articles |
|---|
|
Most recent articles on Sandbox/01 |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox/01 at Clinical Trials.gov Clinical Trials on Sandbox/01 at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox/01
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox/01 Discussion groups on Sandbox/01 Patient Handouts on Sandbox/01 Directions to Hospitals Treating Sandbox/01 Risk calculators and risk factors for Sandbox/01
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox/01 |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2].
Overview
Glanzmann's thrombasthenia is an extremely rare disorder of the blood, in which the platelets lack glycoprotein IIb/IIIa. Hence, no fibrinogen bridging can occur, and bleeding time is significantly prolonged.
Pathophysiology
The GpIIb/IIIa is an adhesion receptor and is expressed in thrombocytes. This receptor is activated when the thrombocyte is stimulated by ADP, epinephrine, collagen and thrombin. The GpIIb/IIIa integrin is essential to the blood coagulation since it has the ability to bind fibrinogen, the von Willebrand factor, fibronectin and vitronectin. This enables the platelet to be activated by contact with the collagen-von Willebrand-complex that is exposed when the endothelial blood vessel lining is damaged and then aggregate with other thrombocytes via fibrinogen.
Patients suffering from Glanzmann's thrombasthenia thus have platelets less able to adhere to each other and to the underlying tissue of damaged blood vessels.
The understanding of its pathophysiology led to the development of GpIIb/IIIa inhibitors, a class of powerful antiplatelet agents.[1]
Etiology
Glanzmann's thrombasthenia can be inherited in an autosomal recessive manner[1] or acquired as an autoimmune disorder.[2]
Clinical Features
Characteristically, there is increased mucosal bleeding:
- epistaxis
- menorrhagia
- increased bleeding post-operatively.
The bleeding tendency is variable but may be severe.
Patients present with moderate bleeding and normal platelet morphology. Aggregation of platelets occurs in response to ristocetin, but not to other agonists such as ADP, thrombin, collagen or adrenalin.
Eponym
It is named for Eduard Glanzmann.[3][4]
Physical examination
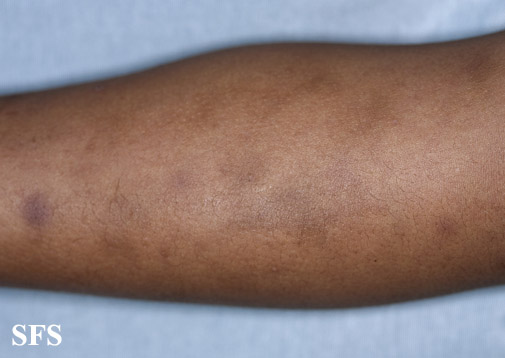
Gallery
Extremities
References
- ↑ 1.0 1.1 Seligsohn U. Glanzmann thrombasthenia: a model disease which paved the way to powerful therapeutic agents. Pathophysiol Haemost Thromb. 2002 Sep-Dec;32(5-6):216-7. PMID 13679645. Free Full Text.
- ↑ Tholouli E, Hay CR, O'Gorman P, Makris M. Acquired Glanzmann's thrombasthenia without thrombocytopenia: a severe acquired autoimmune bleeding disorder. Br J Haematol. 2004 Oct;127(2):209-13. PMID 15461628.
- ↑ Template:WhoNamedIt
- ↑ W. E. Glanzmann. Hereditäre hämorrhägische Thrombasthenie. Ein Beitrag zur Pathologie der Blutplättchen. Jahrbuch für Kinderheilkunde, 1918; 88: 1-42, 113-141.