Thymoma CT: Difference between revisions
Amr Marawan (talk | contribs) No edit summary |
Amr Marawan (talk | contribs) No edit summary |
||
| Line 22: | Line 22: | ||
Image:Th00.png| A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, axial | Image:Th00.png| A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, axial | ||
Image:Th01.png| A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, coronal | Image:Th01.png| A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, coronal | ||
Image:Th02 | Image:Th02.png| CT shows [[Thymoma]] | ||
Image:Th04.png| CT shows [[Invasive Thymoma]] | Image:Th04.png| CT shows [[Invasive Thymoma]] | ||
| Line 37: | Line 35: | ||
Image:Th09.png| CT demonstrates a well circumscribed soft tissue mass in the anterior mediastinum, proven to be thymoma | Image:Th09.png| CT demonstrates a well circumscribed soft tissue mass in the anterior mediastinum, proven to be thymoma | ||
Image:Th11.png| CT showing well defined solid lesion is seen in the anterior mediastinum. No calcification cystic or fat component is seen within | Image:Th11.png| CT showing well defined solid lesion is seen in the anterior mediastinum. No calcification cystic or fat component is seen within | ||
Revision as of 19:16, 25 February 2014
|
Thymoma Microchapters |
|
Diagnosis |
|---|
|
Case Studies |
|
Thymoma CT On the Web |
|
American Roentgen Ray Society Images of Thymoma CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Amr Marawan, M.D. [2]
Overview
The tumor is generally located inside the thymus, and can be calcified. Increased vascular enhancement can be indicative of malignancy, as can be pleural deposits.
CT Scan
When a thymic mass is identified, the made is achieved with histology (obtaining a tissue sample of the mass). When a thymoma is suspected, a CT/CAT scan is generally performed to estimate the size of the tumor, and can be biopsied with a CT-guided needle. There is a small risk of pneumomediastinum, mediastinitis and the risk of damaging the heart or large blood vessels. The final diagnosis is made by removing the thymus. Pathological investigation of the specimen will reveal if the tumor was benign or malignant, although the initial biopsy is usually indicative.[1]
Biopsy
CT-guided core needle biopsy or CT-guided fine needle-aspiration (FNA) should be done to confirm the histological classification and the diagnosis. CT-guided FNA has higher sensitivity and specificity and also less side effects than the core needle biopsy, but it has lower chances of differentiating between thymoma and thymic carcinoma which is important for the appropriate management plan. If both modalities failed to obtain the accurate diagnosis, mediastinoscopy, videothoracoscopy (VATS) or a diagnostic and therapeutic en bloc thymectomy might be considered.[2][2]
-
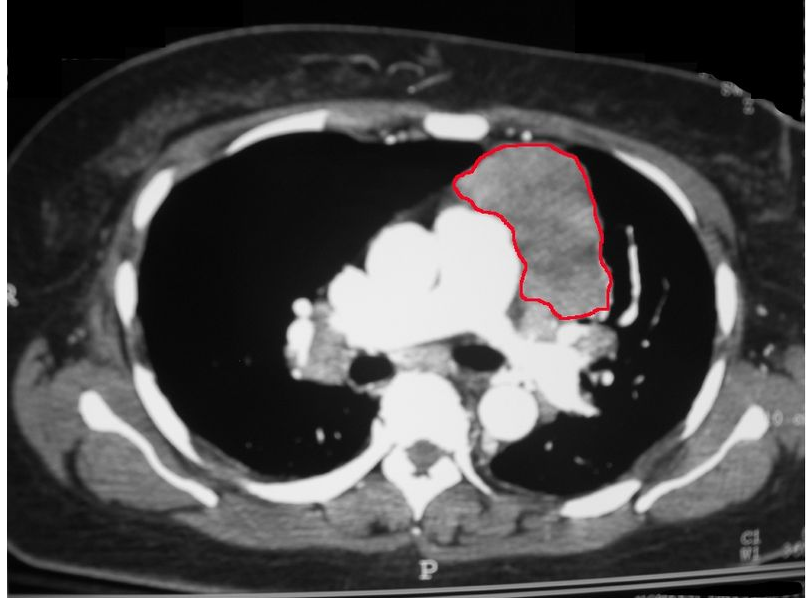
CT shows Thymoma ( CT scan of the chest revealing a large necrotic mass in the left anterior mediastinum (later proven to be a thymoma) and bilateral hilar lymphadenopathy (from concurrent sarcoidosis)
-
CT shows Thymoma (Thymoma, Stage IIA. CT scan, axial)
-
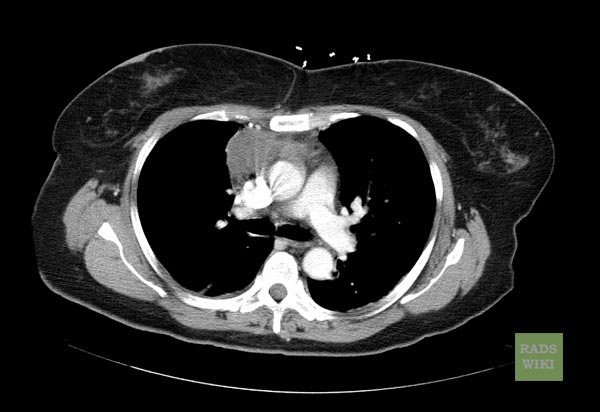
CT shows Thymoma (Image courtesy of RadsWiki and copylefted)
-
A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, axial
-
A 43-year-old female with myasthenia gravis. Chest CT demonstrate a small soft tissue mass at the anterior mediastinum, pathologically proven thymoma, coronal
-
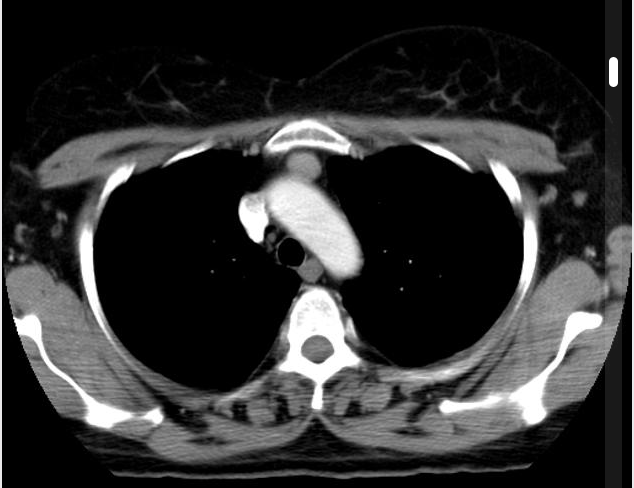
CT shows Thymoma
-
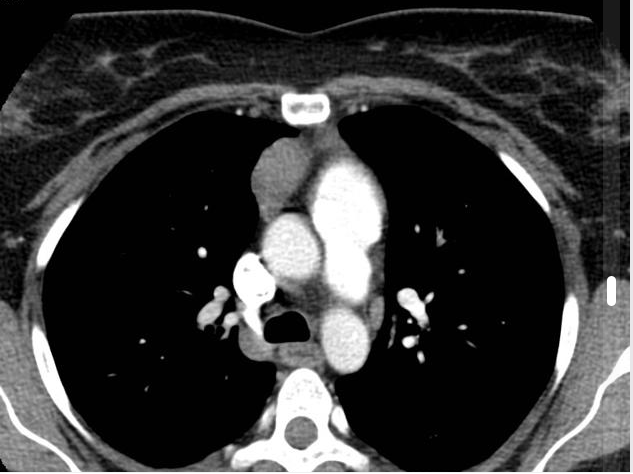
CT shows Invasive Thymoma
-
CT shows Invasive Thymoma
-
CT shows anterior mediastinal mass, pathologically shown to be a thymoma
-
CT demonstrates a well circumscribed soft tissue mass in the anterior mediastinum, proven to be thymoma
-
CT demonstrates a well circumscribed soft tissue mass in the anterior mediastinum, proven to be thymoma
-
CT demonstrates a well circumscribed soft tissue mass in the anterior mediastinum, proven to be thymoma
-
CT showing well defined solid lesion is seen in the anterior mediastinum. No calcification cystic or fat component is seen within
-
CT showing well defined solid lesion is seen in the anterior mediastinum. No calcification cystic or fat component is seen within
References
- ↑ Thomas CR, Wright CD, Loehrer PJ (1999). "Thymoma: state of the art". Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology. 17 (7): 2280–9. PMID 10561285. Retrieved 2012-01-18. Unknown parameter
|month=ignored (help) - ↑ 2.0 2.1 "Percutaneous needle biopsy of the mediastinum: review of 94 procedures".
- ↑ "thymoma". Text " Search " ignored (help); Text " Radiopaedia.org " ignored (help)