Autism causes: Difference between revisions
| Line 4: | Line 4: | ||
==Overview== | ==Overview== | ||
[[Autism]] and [[autism spectrum disorder]]s are complex [[neurodevelopmental disorder]]s. Many ''causes of autism'' have been proposed, but its [[Etiology|theory of causation]] is still incomplete<ref name=Trottier>{{cite journal|author=Trottier G, Srivastava L, Walker CD|title=Etiology of infantile autism: a review of recent advances in genetic and neurobiological research|journal=J Psychiatry Neurosci|date=1999|volume=24|issue=2|pages=103–115|pmid=10212552|url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?pubmedid=10212552|accessdate=2007-07-16}}</ref> | [[Autism]] and [[autism spectrum disorder]]s are complex [[neurodevelopmental disorder]]s. Many ''causes of autism'' have been proposed, but its [[Etiology|theory of causation]] is still incomplete.<ref name=Trottier>{{cite journal|author=Trottier G, Srivastava L, Walker CD|title=Etiology of infantile autism: a review of recent advances in genetic and neurobiological research|journal=J Psychiatry Neurosci|date=1999|volume=24|issue=2|pages=103–115|pmid=10212552|url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?pubmedid=10212552|accessdate=2007-07-16}}</ref> [[Heritability]] contributes about 90% of the risk of a child developing autism, but the [[Heritability of autism|genetics of autism]] are complex and typically it is unclear which genes are responsible.<ref name=Freitag>{{cite journal|author=Freitag CM|title=The genetics of autistic disorders and its clinical relevance: a review of the literature|journal=Mol Psychiatry|volume=12|issue=1|pages=2–22|date=2007|doi=10.1038/sj.mp.4001896|pmid=17033636|url=http://www.nature.com/mp/journal/v12/n1/full/4001896a.html}}</ref> In rare cases, autism is strongly associated with [[Teratology|agents that cause birth defects]].<ref name=Arndt>{{cite journal|journal=Int J Dev Neurosci|date=2005|volume=23|issue=2–3|pages=189–99|title=The teratology of autism|author=Arndt TL, Stodgell CJ, Rodier PM|doi=10.1016/j.ijdevneu.2004.11.001|pmid=15749245}}</ref> Many other causes have been proposed, such as exposure of children to vaccines; these proposals are [[Controversies in autism|controversial]] and the vaccine hypotheses have no [[Evidence-based medicine|convincing scientific evidence]].<ref name=Rutter>{{cite journal|author=[[Michael Rutter|Rutter M]]|title=Incidence of autism spectrum disorders: changes over time and their meaning|journal=Acta Paediatr|volume=94|issue=1|date=2005|pages=2–15|pmid=15858952}}</ref> | ||
==Causes== | ==Causes== | ||
Revision as of 16:49, 11 February 2013
|
Autism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Autism causes On the Web |
|
American Roentgen Ray Society Images of Autism causes |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Autism and autism spectrum disorders are complex neurodevelopmental disorders. Many causes of autism have been proposed, but its theory of causation is still incomplete.[1] Heritability contributes about 90% of the risk of a child developing autism, but the genetics of autism are complex and typically it is unclear which genes are responsible.[2] In rare cases, autism is strongly associated with agents that cause birth defects.[3] Many other causes have been proposed, such as exposure of children to vaccines; these proposals are controversial and the vaccine hypotheses have no convincing scientific evidence.[4]
Causes
Genetics
Genetic factors are the most significant cause for autism spectrum disorders. Early studies of twins estimated heritability to be over 90%, in other words, that genetics explains over 90% of whether a child will develop autism.[2] This may be an overestimate; new twin data and models with structural genetic variation are needed.[6] Many of the non-autistic co-twins had learning or social disabilities. For adult siblings the risk for having one or more features of the broader autism phenotype might be as high as 30%.[7]
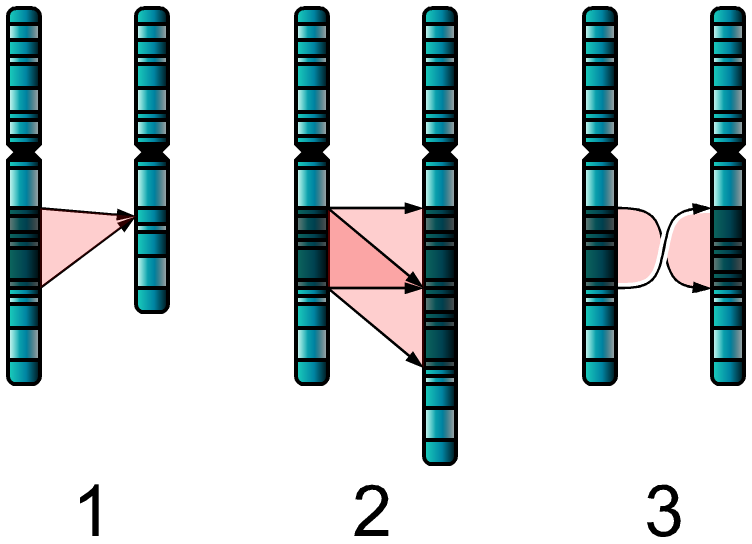
The genetics of autism is complex.[2] Typically, autism cannot be traced to a Mendelian (single-gene) mutation or to single chromosome abnormalities such as Angelman syndrome or fragile X syndrome, and none of the genetic syndromes associated with ASDs has been shown to selectively cause ASD. There may be significant interactions among mutations in several genes, or between the environment and mutated genes. Numerous candidate genes have been located, with only small effects attributable to any particular gene. The large number of autistic individuals with unaffected family members may result from copy number variations (CNVs)—spontaneous deletions or duplications in genetic material during meiosis.[8] Hence, a substantial fraction of autism may be highly heritable but not inherited: that is, the mutation that causes the autism is not present in the parental genome.[5] Linkage analysis has been inconclusive; many association analyses have had inadequate power.[6] More than one gene may be implicated, different genes may be involved in different individuals, and the genes may interact with each other or with environmental factors. Several candidate genes have been located,[9] but the mutations that increase autism risk have not been identified for most candidate genes.
Though autism's genetic factors explain most of autism risk, they do not explain all of it. A common hypothesis is that autism is caused by the interaction of a genetic predisposition and an early environmental insult.[1] Several theories based on environmental factors have been proposed to address the remaining risk. Some of these theories focus on prenatal environmental factors, such as agents that cause birth defects; others focus on the environment after birth, such as children's diets.
A 2007 review of risk factors found associated parental characteristics that included advanced maternal age, advanced paternal age, and maternal place of birth outside Europe or North America. It is not known whether these associations reflect genetic, epigenetic, or environmental factors.[10]
Prenatal Environment
The risk of autism is associated with several prenatal risk factors. Autism has been linked to birth defect agents acting during the first eight weeks from conception, though these cases are rare. Other potential prenatal environmental factors do not have convincing scientific evidence.
Teratogens
Teratogens are environmental agents that cause birth defects. Some agents that are known to cause other birth defects have also been found to be related to autism risk. These include exposure of the embryo to thalidomide, valproic acid, or misoprostol, or to rubella infection in the mother. These cases are rare.[11] Questions have also been raised whether ethanol (grain alcohol) increases autism risk, as part of fetal alcohol syndrome or alcohol-related birth defects, but current evidence is insufficient to determine whether autism risk is actually elevated with ethanol.[12] All known teratogens appear to act during the first eight weeks from conception, and though this does not exclude the possibility that autism can be initiated or affected later, it is strong evidence that autism arises very early in development.[3] Infection-associated immunological events in early pregnancy may affect neural development more than infections in late pregnancy, not only for autism, but also for other psychiatric disorders of presumed neurodevelopmental origin, notably schizophrenia.[13]
Pesticides
A 2007 study by the California Department of Public Health found that women in the first eight weeks of pregnancy who live near farm fields sprayed with the organochlorine pesticides dicofol and endosulfan are several times more likely to give birth to children with autism. The association appeared to increase with dose and decrease with distance from field site to residence. The study's findings suggest that on the order of 7% of autism cases in the California Central Valley might have been connected to exposure to the insecticides drifting off fields into residential areas. These results are highly preliminary due to the small number of women and children involved and lack of evidence from other studies.[14] It is not known whether these pesticides are human teratogens, though endosulfan has significant teratogenic effects in laboratory rats.[15]
A 2005 study showed indirect evidence that prenatal exposure to organophosphate pesticides such as diazinon and chlorpyrifos may contribute to autism in genetically vulnerable children.[16] Several other studies demonstrate the neurodevelopmental toxicity of these agents at relatively low exposure levels.[17]
Folic acid
Folic acid taken during pregnancy might play an important role in causing autism by modulating gene expression through epigenetic mechanism. This hypothesis is untested.[18]
Fetal Testosterone
The fetal testosterone theory hypothesizes that higher levels of testosterone in the amniotic fluid of mothers pushes brain development towards improved ability to see patterns and analyze complex systems while diminishing communication and empathy, emphasizing "male" traits over "female", or in EQ SQ Theory terminology, emphasizing "systemizing" over "empathizing".[19] One project has published several reports suggesting that high levels of fetal testosterone could produce behaviors relevant to those seen in autism.[20] The theory and findings are controversial and many studies contradict the idea that baby boys and girls respond differently to people and objects.[21]
Ultrasound
A 2006 study found that sustained exposure of mouse embryos to ultrasound waves caused a small but statistically significant number of neurons to fail to acquire their proper position during neuronal migration.[22] It is highly unlikely that this result speaks directly to risks of fetal ultrasound as practiced in competent and responsible medical centers.[23] There is no scientific evidence of an association between prenatal ultrasound exposure and autism, but there are very little data on human fetal exposure during diagnostic ultrasound, and the lack of recent epidemiological research and human data in the field has been called "appalling".[24]
Perinatal Environment
Autism is associated with some perinatal and obstetric conditions. A 2007 review of risk factors found associated obstetric conditions that included low birth weight and gestation duration, and hypoxia during childbirth. This association does not demonstrate a causal relationship; an underlying cause could explain both autism and these associated conditions.[10] A 2007 study of premature infants found that those who survived cerebellar hemorrhagic injury (bleeding in the brain that injures the cerebellum) were significantly more likely to show symptoms of autism than controls without the injury.[25]
Postnatal Environment
A wide variety of postnatal contributors to autism have been proposed, including gastrointestinal or immune system abnormalities, allergies, and exposure of children to drugs, vaccines, infection, certain foods, or heavy metals. The evidence for these risk factors is anecdotal and has not been confirmed by reliable studies.[4] The subject remains controversial and extensive further searches for environmental factors are underway.[11]
Leaky Gut Syndrome
Parents have reported gastrointestinal (GI) disturbances in autistic children, and several studies have investigated possible associations between autism and the gut.[26] The controversial Wakefield et al. vaccine paper discussed in "MMR vaccine" below also suggested that some bowel disorders may allow antigens to pass from food into the bloodstream and then to contribute to brain dysfunction.[27] This produced several lines of investigation.
For example, employing secretin's effects on digestion, a 1998 study of three children with ASD treated with secretin infusion reported improved GI function and dramatic improvement in behavior, which suggested an association between GI and brain function in autistic children.[28] After this study, many parents sought secretin treatment and a black market for the hormone developed quickly.[26] However, later studies found secretin ineffective in treating autism.[29]
Leaky gut syndrome theories also inspired several dietary treatments, including gluten-free diets, casein-free diets, antifungal diets, low-sugar diets, as well as supplements that include nystatin, [[B12|BTemplate:Ssub]], and probiotics. Parents are more likely to get advice about these diets from other parents, the media, and the Internet than from medical experts. There is no solid research evidence that autistic children are more likely to have GI symptoms than typical children.[26] In particular, design flaws in studies of elimination diets mean that the currently available data are inadequate to guide treatment recommendations.[30]
Viral Infection
Many studies have presented evidence for and against association of autism with viral infection after birth. Laboratory rats infected with Borna disease virus show some symptoms similar to those of autism but blood studies of autistic children show no evidence of infection by this virus. Members of the herpes virus family may have a role in autism, but the evidence so far is anecdotal. Viruses have long been suspected as triggers for immune-mediated diseases such as multiple sclerosis but showing a direct role for viral causation is difficult in those diseases, and mechanisms whereby viral infections could lead to autism are speculative.[31]
Oxidative Stress
This theory hypothesizes that toxicity and oxidative stress may cause autism in some cases by damaging Purkinje cells in the cerebellum after birth. One possibility is that glutathione is involved.[32]
Amygdala Neurons
This theory hypothesizes that an early developmental failure involving the amygdala cascades on the development of cortical areas that mediate social perception in the visual domain. The fusiform face area of the ventral stream is implicated. The idea is that it is involved in social knowledge and social cognition, and that the deficits in this network are instrumental in causing autism.[33]
Vitamin D
This theory hypothesizes that autism is caused by vitamin D deficiency, and that recent increases in diagnosed cases of autism are due to medical advice to avoid the sun. The theory has not been studied scientifically.[34]
Lead
Lead poisoning has been suggested as a possible risk factor for autism, as the lead blood levels of autistic children has been reported to be significantly higher than typical. The atypical eating behaviors of autistic children, along with habitual mouthing and pica, make it hard to determine whether increased lead levels are a cause or a consequence of autism.[35]
Mercury and MMR Vaccine
This theory hypothesizes that autism is associated with mercury poisoning, based on perceived similarity of symptoms.[36] The principal source of human exposure to organic mercury is via fish consumption and for inorganic mercury is dental amalgams. Other forms of exposure, such as in cosmetics and vaccines, also occur. The evidence so far is indirect for the association between autism and mercury exposure after birth, as no direct test has been reported, and there is no evidence of an association between autism and postnatal exposure to any neurotoxicant.[37]
A 2003 study reported that mercury measurements of hair samples from autistic children's first haircuts were significantly lower than a matched group of normal children, declining as measures of severity increased,[38] but a later meta-analysis based on two studies found that there was not enough evidence to conclude that hair mercury level is lower in autistic children.[39] A 2006 study found an association between autism and environmental releases of mercury, primarily from coal power plants; this study used Texas county-wide data and did not distinguish between prenatal and postnatal exposure.[40]
Although parents may first become aware of autistic symptoms in their child around the time of a routine vaccination, and parental concern about vaccines has led to a decreasing uptake of childhood immunizations and an increasing likelihood of measles outbreaks, there is overwhelming scientific evidence showing no causal association between the measles-mumps-rubella vaccine and autism, and there is no scientific evidence that the vaccine preservative thiomersal helps cause autism.[41]
Television Watching
Three economists hypothesized that early childhood television viewing acts as an environmental trigger for an underlying genetic predisposition. They found that precipitation was associated with autism by examining county-level autism data for California, Oregon, and Washington. Precipitation is also associated with television watching, and their analysis concluded that just under 40% of autism diagnoses in the three states result from television watching due to precipitation.[42] This study has not been published in a refereed journal and its results have not been confirmed by others.
Refrigerator Mother
Bruno Bettelheim believed that autism was linked to early childhood trauma, and his work was highly influential for decades both in the medical and popular spheres. Parents, especially mothers, of individuals with autism were blamed for having caused their child's condition through the withholding of affection.[43] Leo Kanner, who first described autism,[44] suggested that parental coldness might contribute to autism.[45] Although Kanner eventually renounced the theory, Bettelheim put an almost exclusive emphasis on it in both his medical and his popular books. Treatments based on these theories failed to help children with autism, and after Bettelheim's death it came out that his reported rates of cure (around 85%) were found to be fraudulent.[46]
Other Psychogenic Theories
Psychogenic theories in general have become increasingly unpopular, particularly since twin studies have shown that autism is highly heritable. Nevertheless, some case reports have found that deep institutional privation can result in "quasi-autistic" features without the neuroanatomical differences.[47][48] Other case reports have suggested that children predisposed genetically to autism can develop "autistic devices" in response to traumatic events such as the birth of a sibling.[49]
References
- ↑ 1.0 1.1 Trottier G, Srivastava L, Walker CD (1999). "Etiology of infantile autism: a review of recent advances in genetic and neurobiological research". J Psychiatry Neurosci. 24 (2): 103–115. PMID 10212552. Retrieved 2007-07-16.
- ↑ 2.0 2.1 2.2 Freitag CM (2007). "The genetics of autistic disorders and its clinical relevance: a review of the literature". Mol Psychiatry. 12 (1): 2–22. doi:10.1038/sj.mp.4001896. PMID 17033636.
- ↑ 3.0 3.1 Arndt TL, Stodgell CJ, Rodier PM (2005). "The teratology of autism". Int J Dev Neurosci. 23 (2–3): 189–99. doi:10.1016/j.ijdevneu.2004.11.001. PMID 15749245.
- ↑ 4.0 4.1 Rutter M (2005). "Incidence of autism spectrum disorders: changes over time and their meaning". Acta Paediatr. 94 (1): 2–15. PMID 15858952.
- ↑ 5.0 5.1 Beaudet AL (2007). "Autism: highly heritable but not inherited". Nat Med. 13 (5): 534–6. doi:10.1038/nm0507-534. PMID 17479094.
- ↑ 6.0 6.1 Sykes NH, Lamb JA (2007). "Autism: the quest for the genes". Expert Rev Mol Med. 9 (24): 1–15. doi:10.1017/S1462399407000452. PMID 17764594.
- ↑ Folstein SE, Rosen-Sheidley B (2001). "Genetics of autism: complex aetiology for a heterogeneous disorder". Nat Rev Genet. 2 (12): 943–55. doi:10.1038/35103559. PMID 11733747.
- ↑ Sebat J, Lakshmi B, Malhotra D; et al. (2007). "Strong association of de novo copy number mutations with autism". Science. 316 (5823): 445–9. doi:10.1126/science.1138659. PMID 17363630.
- ↑ Persico AM, Bourgeron T (2006). "Searching for ways out of the autism maze: genetic, epigenetic and environmental clues". Trends Neurosci. 29 (7): 349–58. doi:10.1016/j.tins.2006.05.010. PMID 16808981.
- ↑ 10.0 10.1 Kolevzon A, Gross R, Reichenberg A (2007). "Prenatal and perinatal risk factors for autism". Arch Pediatr Adolesc Med. 161 (4): 326–33. PMID 17404128.
- ↑ 11.0 11.1 Szpir M (2006). "Tracing the origins of autism: a spectrum of new studies". Environ Health Perspect. 114 (7): A412–8. PMID 16835042.
- ↑ Fombonne E (2002). "Is exposure to alcohol during pregnancy a risk factor for autism?". J Autism Dev Disord. 32 (3): 243. doi:10.1023/A:1015466100838. PMID 12108626.
- ↑ Meyer U, Yee BK, Feldon J (2007). "The neurodevelopmental impact of prenatal infections at different times of pregnancy: the earlier the worse?". Neuroscientist. 13 (3): 241–56. doi:10.1177/1073858406296401. PMID 17519367.
- ↑ Roberts EM, English PB, Grether JK, Windham GC, Somberg L, Wolff C (2007). "Maternal residence near agricultural pesticide applications and autism spectrum disorders among children in the California Central Valley". Environ Health Perspect. 115 (10): 1482–9. doi:10.1289/ehp.10168. PMID 17938740. Lay summary – EHP (2007).
- ↑ Singh ND, Sharma AK, Dwivedi P, Patil RD, Kumar M (2007). "Citrinin and endosulfan induced teratogenic effects in Wistar rats". J Appl Toxicol. 27 (2): 143–51. doi:10.1002/jat.1185. PMID 17186572.
- ↑ D'Amelio M, Ricci I, Sacco R; et al. (2005). "Paraoxonase gene variants are associated with autism in North America, but not in Italy: possible regional specificity in gene-environment interactions". Mol Psychiatry. 10 (11): 1006–16. doi:10.1038/sj.mp.4001714. PMID 16027737.
- ↑ Karr CJ, Solomon GM, Brock-Utne AC (2007). "Health effects of common home, lawn, and garden pesticides". Pediatr Clin North Am. 54 (1): 63–80. doi:10.1016/j.pcl.2006.11.005. PMID 17306684.
- ↑ Muskiet FA, Kemperman RF (2006). "Folate and long-chain polyunsaturated fatty acids in psychiatric disease". J Nutr Biochem. 17 (11): 717–27. doi:10.1016/j.jnutbio.2006.02.001. PMID 16650750.
- ↑ Baron-Cohen S (2004). The Essential Difference: Male and Female Brains and the Truth About Autism. Basic Books. ISBN 046500556X.
- ↑ Fetal testosterone studies:
- Knickmeyer RC, Baron-Cohen S (2006). "Fetal testosterone and sex differences". Early Hum Dev. 82 (12): 755–60. doi:10.1016/j.earlhumdev.2006.09.014. PMID 17084045.
- Morelle R (2007-09-11). "Hormone linked to autistic traits". BBC. Retrieved 2007-09-11.
- ↑ Rivers C (2006-09-28). "Discrimination against the female brain". AlterNet. Retrieved 2006-12-10.
- ↑ Ang ES Jr, Gluncic V, Duque A, Schafer ME, Rakic P (2006). "Prenatal exposure to ultrasound waves impacts neuronal migration in mice". Proc Natl Acad Sci U S A. 103 (34): 12903–10. doi:10.1073/pnas.0605294103. PMID 16901978.
- ↑ Caviness VS, Grant PE (2006). "Our unborn children at risk?". Proc Natl Acad Sci U S A. 103 (34): 12661–2. doi:10.1073/pnas.0605505103.
- ↑ Abramowicz JS (2007). "Prenatal exposure to ultrasound waves: is there a risk?". Ultrasound Obstet Gynecol. 29 (4): 363–7. doi:10.1002/uog.3983. PMID 17352453.
- ↑ Limperopoulos C, Bassan H, Gauvreau K; et al. (2007). "Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors?". Pediatrics. 120 (3): 584–93. doi:10.1542/peds.2007-1041. PMID 17766532.
- ↑ 26.0 26.1 26.2 Johnson TW (2006). "Dietary considerations in autism: identifying a reasonable approach". Top Clin Nutr. 21 (3): 212–25.
- ↑ Wakefield A, Murch S, Anthony A; et al. (1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/S0140-6736(97)11096-0. PMID 9500320. Retrieved 2007-09-05.
- ↑ Horvath K, Stefanatos G, Sokolski KN, Wachtel R, Nabors L, Tildon JT (1998). "Improved social and language skills after secretin administration in patients with autistic spectrum disorders". J Assoc Acad Minor Phys. 9 (1): 9–15. PMID 9585670.
- ↑ Sturmey P (2005). "Secretin is an ineffective treatment for pervasive developmental disabilities: a review of 15 double-blind randomized controlled trials". Res Dev Disabil. 26 (1): 87–97. PMID 15590241.
- ↑ Christison GW, Ivany K (2006). "Elimination diets in autism spectrum disorders: any wheat amidst the chaff?". J Dev Behav Pediatr. 27 (2 Suppl 2): S162–71. PMID 16685183.
- ↑ Libbey JE, Sweeten TL, McMahon WM, Fujinami RS (2005). "Autistic disorder and viral infections". J Neurovirol. 11 (1): 1–10. doi:10.1080/13550280590900553. PMID 15804954.
- ↑ Kern JK, Jones AM (2006). "Evidence of toxicity, oxidative stress, and neuronal insult in autism". J Toxicol Environ Health B Crit Rev. 9 (6): 485–99. doi:10.1080/10937400600882079. PMID 17090484.
- ↑ Schultz RT (2005). "Developmental deficits in social perception in autism: the role of the amygdala and fusiform face area". Int J Dev Neurosci. 23 (2–3): 125–41. doi:10.1016/j.ijdevneu.2004.12.012. PMID 15749240.
- ↑ Cannell JJ (2007). "Autsim and vitamin D". Med Hypotheses. PMID 17920208.
- ↑ Zafeiriou DI, Ververi A, Vargiami E (2007). "Childhood autism and associated comorbidities". Brain Dev. 29 (5): 257–72. doi:10.1016/j.braindev.2006.09.003. PMID 17084999.
- ↑ Bernard S, Enayati A, Redwood L, Roger H, Binstock T (2001). "Autism: a novel form of mercury poisoning". Med Hypotheses. 56 (4): 462–71. doi:10.1054/mehy.2000.1281. PMID 11339848.
- ↑ Davidson PW, Myers GJ, Weiss B (2004). "Mercury exposure and child development outcomes". Pediatrics. 113 (4 Suppl): 1023–9. PMID 15060195.
- ↑ Holmes AS, Blaxill MF, Haley BE (2003). "Reduced levels of mercury in first baby haircuts of autistic children". Int J Toxicol. 22 (4): 277–85. PMID 12933322.
- ↑ Ng DK, Chan CH, Soo MT, Lee RS (2007). "Low-level chronic mercury exposure in children and adolescents: meta-analysis". Pediatr Int. 49 (1): 80–7. doi:10.1111/j.1442-200X.2007.02303.x. PMID 17250511.
- ↑ Palmer RF, Blanchard S, Stein Z, Mandell D, Miller C (2006). "Environmental mercury release, special education rates, and autism disorder: an ecological study of Texas". Health Place. 12 (2): 203–9. doi:10.1016/j.healthplace.2004.11.005. PMID 16338635.
- ↑ Vaccines and autism:
- ↑ Template:Cite paper
- ↑ Bettelheim B (1967). The Empty Fortress: Infantile Autism and the Birth of the Self. Free Press. ISBN 0029031400.
- ↑ Kanner L (1943). "Autistic disturbances of affective contact". Nerv Child. 2: 217–50. Reprint (1968) Acta Paedopsychiatr 35 (4): 100–36. PMID 4880460.
- ↑ Kanner L (1949). "Problems of nosology and psychodynamics in early childhood autism". Am J Orthopsychiatry. 19 (3): 416–26. PMID 18146742.
- ↑ Gardner M (2000). "The brutality of Dr. Bettelheim". Skeptical Inquirer. 24 (6): 12–4.
- ↑ Rutter ML, Kreppner JM, O'Connor TG, English and Romanian Adoptees (ERA) study team (2001). "Specificity and heterogeneity in children's responses to profound institutional privation". Br J Psychiatry. 179 (2): 97–103. PMID 11483469.
- ↑ Hoksbergen R, ter Laak J, Rijk K, van Dijkum C, Stoutjesdijk F (2005). "Post-Institutional Autistic Syndrome in Romanian adoptees". J Autism Dev Disord. 35 (5): 615–23. doi:10.1007/s10803-005-0005-x. PMID 16167089.
- ↑ Gomberoff M, De Gomberoff LP (2000). "Autistic devices in small children in mourning". Int J Psychoanal. 81 (5): 907–20. PMID 11109576.