Carotid endarterectomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{CMG}} | {{CMG}} | ||
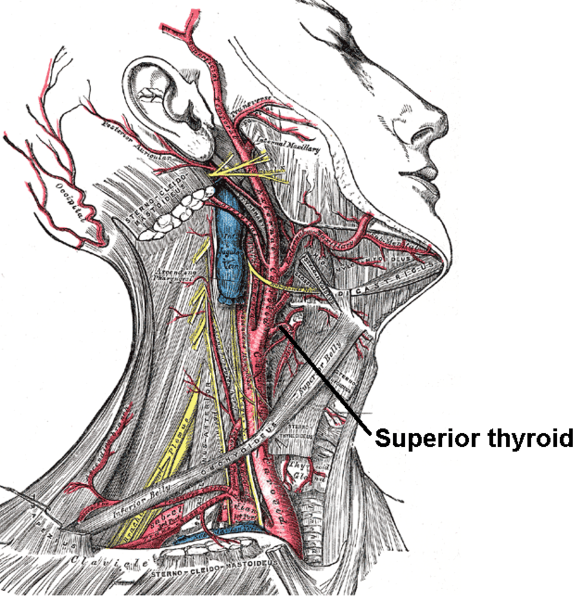
[[Image:Gray513.png|thumbnail|250px|right|The [[carotid artery]] and other arteries of the neck.]] | [[Image:Gray513.png|thumbnail|250px|right|The [[carotid artery]] and other arteries of the neck.]] | ||
==Overview== | ==Overview== | ||
'''Carotid endarterectomy (CEA)''' is a [[surgery|surgical]] procedure used to correct [[carotid stenosis]] (narrowing of the [[carotid artery]] lumen by [[atheroma]]), used particularly when this causes medical problems, such as [[transient ischemic attack]]s (TIAs) or [[cerebrovascular accident]]s (CVAs, strokes). [[Endarterectomy]] is the removal of material on the inside (''end-'') of an [[artery]]. [[Angioplasty]] and [[stent]]ing of the carotid artery are undergoing investigation as alternatives to carotid endarterectomy. | '''Carotid endarterectomy (CEA)''' is a [[surgery|surgical]] procedure used to correct [[carotid stenosis]] (narrowing of the [[carotid artery]] lumen by [[atheroma]]), used particularly when this causes medical problems, such as [[transient ischemic attack]]s (TIAs) or [[cerebrovascular accident]]s (CVAs, strokes). [[Endarterectomy]] is the removal of material on the inside (''end-'') of an [[artery]]. [[Angioplasty]] and [[stent]]ing of the carotid artery are undergoing investigation as alternatives to carotid endarterectomy. | ||
==Indications== | ==Indications== | ||
| Line 21: | Line 17: | ||
===Asymptomatic Patients=== | ===Asymptomatic Patients=== | ||
The European asymptomatic carotid surgery trial (ACST) found that asymptomatic patients may also benefit from the procedure, but only the group with a high grade stenosis (greater than 75%). For maximum benefit patients should be operated on soon after a TIA or stroke, preferably within the first month. | The European asymptomatic carotid surgery trial (ACST) found that asymptomatic patients may also benefit from the procedure, but only the group with a high grade stenosis (greater than 75%). For maximum benefit patients should be operated on soon after a TIA or stroke, preferably within the first month. | ||
==Procedure== | |||
The internal, common and external carotid arteries are clamped, the lumen of the internal carotid artery is opened, and the atheromatous plaque substance removed. The artery is closed, hemostasis achieved, and the overlying layers closed. Many surgeons lay a temporary [[shunt]] to ensure blood supply to the [[brain]] during the procedure. The procedure may be performed under general or local anaesthesia. The latter allows for direct monitoring of neurological status by intra-operative verbal contact and testing of grip strength. With general anaesthesia indirect methods of assessing cerebral perfusion must be used, such as [[electroencephalography]] (EEG), transcranial doppler analysis and carotid artery stump pressure monitoring. At present there is no good evidence to show any major difference in outcome between local and general anaesthesia. | |||
Non-invasive procedures have been developed, by threading catheters through the femoral artery, up through the aorta, then inflating a balloon to dilate the carotid artery, with or without a wire-mesh shunt. The safety and effectiveness of these procedures is controversial. In the SAPPHIRE study, Yadav concluded that this procedure, known as [[carotid stenting]], was non-inferior to carotid endarterectomy in total adverse events, and lowered event rates for major stroke, cranial nerve palsy, and myocardial infarction, in patients at high risk for surgery.<ref>Yadav et al., Protected Carotid Artery Stenting versus Endarterectomy in High-Risk Patients, N Engl J Med . 2004 October 7;351:1493-1501 PMID 15470212.</ref> However, Cambria concluded that the study was not sufficiently powered to detect differences in stroke and death, and final conclusions must await larger trials.<ref>Cambria RP. Stenting for carotid-artery stenosis. N Engl J Med. 2004 Oct 7;351:1565-7. PMID 15470220</ref> | |||
==Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease: Periprocedural Management of Patients Undergoing Carotid Endarterectomy<ref name="pmid21282505">{{cite journal| author=Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL et al.| title=2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery. | journal=Circulation | year= 2011 | volume= 124 | issue= 4 | pages= 489-532 | pmid=21282505 | doi=10.1161/CIR.0b013e31820d8d78 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21282505 }} </ref> (DO NOT EDIT)== | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LightGreen"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class I]] | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''1.''' Aspirin (81 to 325 mg daily) is recommended before CEA and may be continued indefinitely postoperatively. (Level of Evidence: A)'' <nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''2.''' Beyond the first month after CEA, aspirin (75 to 325 mg daily), clopidogrel (75 mg daily), or the combination of low-dose aspirin plus extended-release dipyridamole (25 and 200 mg twice daily, respectively) should be administered for long-term prophylaxis against ischemic cardiovascular events. (Level of Evidence: B)'' <nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''3.''' Administration of antihypertensive medication is recommended as needed to control blood pressure before and after CEA. (Level of Evidence: C)'' <nowiki>"</nowiki> | |||
|- | |||
| bgcolor="LightGreen"|<nowiki>"</nowiki>'''3.''' The findings on clinical neurological examination should be documented within 24 hours before and after CEA. (Level of Evidence: C)'' <nowiki>"</nowiki> | |||
|} | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background:LemonChiffon"|[[ACC AHA guidelines classification scheme#Classification of Recommendations|Class IIa]] | |||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''1.''' Patch angioplasty can be beneficial for closure of the arteriotomy after CEA.62,63 (Level of Evidence: B)'' <nowiki>"</nowiki> | |||
|- | |||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''2.''' Administration of statin lipid-lowering medication for prevention of ischemic events is reasonable for patients who have undergone CEA irrespective of serum lipid levels, although the optimum agent and dose and the efficacy for prevention of restenosis have not been established. (Level of Evidence: B)'' <nowiki>"</nowiki> | |||
= | |- | ||
|bgcolor="LemonChiffon"|<nowiki>"</nowiki>'''3.''' Noninvasive imaging of the extracranial carotid arteries is reasonable 1 month, 6 months, and annually after CEA to assess patency and exclude the development of new or contralateral lesions. Once stability has been established over an extended period, surveillance at longer intervals may be appropriate. Termination of surveillance is reasonable when the patient is no longer a candidate for intervention. (Level of Evidence: C)'' <nowiki>"</nowiki> | |||
|} | |||
==Contra-indications== | ==Contra-indications== | ||
| Line 37: | Line 63: | ||
About 3% of patients will suffer neurological complications as a result of the procedure. [[Hemorrhage]] of the wound bed is potentially life-threatening, as swelling of the neck due to [[hematoma]] could compress the [[Vertebrate trachea|trachea]]. Rarely, the [[hypoglossal nerve]] can be damaged during surgery. This is likely to result in fasiculations developing on the tongue and paralysis of the affected side: on sticking it out, the patients tongue will deviate toward the affected side. | About 3% of patients will suffer neurological complications as a result of the procedure. [[Hemorrhage]] of the wound bed is potentially life-threatening, as swelling of the neck due to [[hematoma]] could compress the [[Vertebrate trachea|trachea]]. Rarely, the [[hypoglossal nerve]] can be damaged during surgery. This is likely to result in fasiculations developing on the tongue and paralysis of the affected side: on sticking it out, the patients tongue will deviate toward the affected side. | ||
Another rare but potentially serious complication is hyperperfusion syndrome due to the sudden increase in perfusion of the vasculature distal to stenosis.<ref>{{cite journal |author=van Mook WN, Rennenberg RJ, Schurink GW, ''et al'' |title=Cerebral hyperperfusion syndrome |journal=Lancet Neurol |volume=4 |issue=12 |pages=877–88 |year=2005 |pmid=16297845 |doi=10.1016/S1474-4422(05)70251-9}}</ref> | Another rare but potentially serious complication is hyperperfusion syndrome due to the sudden increase in perfusion of the vasculature distal to stenosis.<ref>{{cite journal |author=van Mook WN, Rennenberg RJ, Schurink GW, ''et al'' |title=Cerebral hyperperfusion syndrome |journal=Lancet Neurol |volume=4 |issue=12 |pages=877–88 |year=2005 |pmid=16297845 |doi=10.1016/S1474-4422(05)70251-9}}</ref> | ||
==Carotid Endarterectomy (CEA) vs Stenting== | |||
* The CREST study showed a higher rate of death/MI in patients treated with stenting vs CEA: 6.4% vs 4.7% | |||
* CEA is preferred in patients who impaired renal function who are at risk of [[contrast induced nephropathy]], tortuous calcified aortoas, complex eccentric calcified lesions | |||
* Stenting may be preferred in patients with high carotid bifurcations where it is hard for surgeons to technically perform the surgery | |||
* If an elderly patient has a [[transient ischemic attack]] and if there is a narrowing in the ipsilateral artery, then carotid endarterectomy should be performed within two weeks of the symptoms. | |||
==Related Chapters== | |||
*[[Carotid artery stenosis]] | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Vascular surgery procedures}} | {{Vascular surgery procedures}} | ||
Revision as of 14:37, 4 October 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Carotid endarterectomy (CEA) is a surgical procedure used to correct carotid stenosis (narrowing of the carotid artery lumen by atheroma), used particularly when this causes medical problems, such as transient ischemic attacks (TIAs) or cerebrovascular accidents (CVAs, strokes). Endarterectomy is the removal of material on the inside (end-) of an artery. Angioplasty and stenting of the carotid artery are undergoing investigation as alternatives to carotid endarterectomy.
Indications
Surgical intervention to relieve atherosclerotic obstruction of the carotid arteries was first performed at St. Mary’s Hospital, London, in 1954. Since then, evidence for its effectiveness in different patient groups has accumulated. In 2003 nearly 140,000 carotid endarterectomies were performed in the USA (Halm).
The aim of CEA is to prevent the adverse sequelae of carotid artery stenosis secondary to atherosclerotic disease, i.e. stroke. As with any prophylactic operation, careful evaluation of the relative benefits and risks of the procedure is required on an individual patient basis. Peri-operative combined mortality and major stroke risk is 2 – 5%.
Carotid stenosis is diagnosed with ultrasound doppler studies of the neck arteries or magnetic resonance arteriography (MRA). The circle of Willis typically provides a collateral blood supply. Symptoms have to affect the other side of the body; if they do not, they may not be caused by the stenosis, and arterectomy it will be of minimal benefit.
Symptomatic Patients
The North American Symptomatic Carotid Endarterectomy Trial (NASCET) and the European Carotid Surgery Trial (ECST) are both large randomized class 1 studies which have helped define current indications for carotid endarterectomy. The NASCET found that for every six patients treated, one major stroke would be prevented at two years (i.e. a “number needed to treat” (NNT) of six) for symptomatic patients with a 70 – 99% stenosis. Symptomatic patients with less severe carotid occlusion (50 – 69%) had a smaller benefit, with a NNT of 22 at five years (Barclay). In addition, co-morbidity adversely affects the outcome; patients with multiple medical problems have a higher post-operative mortality and hence benefit less from the procedure.
Asymptomatic Patients
The European asymptomatic carotid surgery trial (ACST) found that asymptomatic patients may also benefit from the procedure, but only the group with a high grade stenosis (greater than 75%). For maximum benefit patients should be operated on soon after a TIA or stroke, preferably within the first month.
Procedure
The internal, common and external carotid arteries are clamped, the lumen of the internal carotid artery is opened, and the atheromatous plaque substance removed. The artery is closed, hemostasis achieved, and the overlying layers closed. Many surgeons lay a temporary shunt to ensure blood supply to the brain during the procedure. The procedure may be performed under general or local anaesthesia. The latter allows for direct monitoring of neurological status by intra-operative verbal contact and testing of grip strength. With general anaesthesia indirect methods of assessing cerebral perfusion must be used, such as electroencephalography (EEG), transcranial doppler analysis and carotid artery stump pressure monitoring. At present there is no good evidence to show any major difference in outcome between local and general anaesthesia.
Non-invasive procedures have been developed, by threading catheters through the femoral artery, up through the aorta, then inflating a balloon to dilate the carotid artery, with or without a wire-mesh shunt. The safety and effectiveness of these procedures is controversial. In the SAPPHIRE study, Yadav concluded that this procedure, known as carotid stenting, was non-inferior to carotid endarterectomy in total adverse events, and lowered event rates for major stroke, cranial nerve palsy, and myocardial infarction, in patients at high risk for surgery.[1] However, Cambria concluded that the study was not sufficiently powered to detect differences in stroke and death, and final conclusions must await larger trials.[2]
Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease: Periprocedural Management of Patients Undergoing Carotid Endarterectomy[3] (DO NOT EDIT)
| Class I |
| "1. Aspirin (81 to 325 mg daily) is recommended before CEA and may be continued indefinitely postoperatively. (Level of Evidence: A) " |
| "2. Beyond the first month after CEA, aspirin (75 to 325 mg daily), clopidogrel (75 mg daily), or the combination of low-dose aspirin plus extended-release dipyridamole (25 and 200 mg twice daily, respectively) should be administered for long-term prophylaxis against ischemic cardiovascular events. (Level of Evidence: B) " |
| "3. Administration of antihypertensive medication is recommended as needed to control blood pressure before and after CEA. (Level of Evidence: C) " |
| "3. The findings on clinical neurological examination should be documented within 24 hours before and after CEA. (Level of Evidence: C) " |
| Class IIa |
| "1. Patch angioplasty can be beneficial for closure of the arteriotomy after CEA.62,63 (Level of Evidence: B) " |
| "2. Administration of statin lipid-lowering medication for prevention of ischemic events is reasonable for patients who have undergone CEA irrespective of serum lipid levels, although the optimum agent and dose and the efficacy for prevention of restenosis have not been established. (Level of Evidence: B) " |
| "3. Noninvasive imaging of the extracranial carotid arteries is reasonable 1 month, 6 months, and annually after CEA to assess patency and exclude the development of new or contralateral lesions. Once stability has been established over an extended period, surveillance at longer intervals may be appropriate. Termination of surveillance is reasonable when the patient is no longer a candidate for intervention. (Level of Evidence: C) " |
Contra-indications
The procedure cannot be performed in case of:
- Complete internal carotid artery obstruction (because the intraluminal thrombus then extends too far downstream, well into the intracranial portion of the artery, for endarterectomy to be successful).
- Previous stroke on the ipsilateral side with heavy sequelae, because there is no point in preventing what has already happened.
- Patient deemed unfit for the operation by the anaesthesiologist.
Complications
About 3% of patients will suffer neurological complications as a result of the procedure. Hemorrhage of the wound bed is potentially life-threatening, as swelling of the neck due to hematoma could compress the trachea. Rarely, the hypoglossal nerve can be damaged during surgery. This is likely to result in fasiculations developing on the tongue and paralysis of the affected side: on sticking it out, the patients tongue will deviate toward the affected side. Another rare but potentially serious complication is hyperperfusion syndrome due to the sudden increase in perfusion of the vasculature distal to stenosis.[4]
Carotid Endarterectomy (CEA) vs Stenting
- The CREST study showed a higher rate of death/MI in patients treated with stenting vs CEA: 6.4% vs 4.7%
- CEA is preferred in patients who impaired renal function who are at risk of contrast induced nephropathy, tortuous calcified aortoas, complex eccentric calcified lesions
- Stenting may be preferred in patients with high carotid bifurcations where it is hard for surgeons to technically perform the surgery
- If an elderly patient has a transient ischemic attack and if there is a narrowing in the ipsilateral artery, then carotid endarterectomy should be performed within two weeks of the symptoms.
Related Chapters
References
- ↑ Yadav et al., Protected Carotid Artery Stenting versus Endarterectomy in High-Risk Patients, N Engl J Med . 2004 October 7;351:1493-1501 PMID 15470212.
- ↑ Cambria RP. Stenting for carotid-artery stenosis. N Engl J Med. 2004 Oct 7;351:1565-7. PMID 15470220
- ↑ Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL; et al. (2011). "2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons, American College of Radiology, American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery, Society for Vascular Medicine, and Society for Vascular Surgery". Circulation. 124 (4): 489–532. doi:10.1161/CIR.0b013e31820d8d78. PMID 21282505.
- ↑ van Mook WN, Rennenberg RJ, Schurink GW; et al. (2005). "Cerebral hyperperfusion syndrome". Lancet Neurol. 4 (12): 877–88. doi:10.1016/S1474-4422(05)70251-9. PMID 16297845.