Relapsing fever pathophysiology: Difference between revisions
| Line 9: | Line 9: | ||
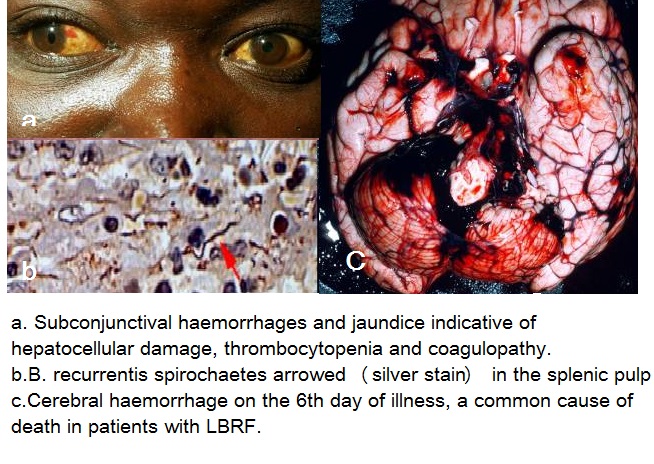
*Following transmission, the [[spirochetes]] replicate [[extracellularly]] and remain predominantly the [[plasma]] space. Some organisms are found within circulating polymorphonuclear cells or [[Reticuloendothelial|reticuloendothelial cell]]s, or occasionally can be found in tissues such as the [[liver]], [[spleen]], [[kidney]], [[heart]], or [[brain]], with foci of perivascular [[inflammation]], [[hemorrhage]], and [[infarction]] at autopsy. Organisms are cleared predominantly by opsonizing [[antibodies]] with the resolution of symptoms ( [[afebrile]] period), followed several days or weeks later by the reemergence of a new [[antigenic]] strain, high-level spirochetemia, when high-level [[spirochetemia]] (104-108 organisms m!) develops, at which time symptoms begin abruptly. During episodes of [[spirochetemia]], the [[organisms]] may invade the brain, eye, inner ear, heart, liver. Splenic [[abscesses]] and infarcts, and hemorrhages within the central nervous system, a perivascular histiocytic interstitial [[myocarditis]], conduction defects, [[arrhythmias]], and [[myocardial]] failure, [[splenic rupture]] with massive hemorrhage, [[cerebral hemorrhage]], and [[hepatic failure]] are seen in LBRF which can result in sudden death.Hepatitis with patchy [[hemorrhages]] and [[necrosis]], [[meningitis]], and [[perisplenitis]], thrombi in small [[vessels]] also are found. [[Thrombi]] are occasionally found occluding [[small vessel]]s.<ref name="pmid30869050">{{cite journal |vauthors=Warrell DA |title=Louse-borne relapsing fever (Borrelia recurrentis infection) |journal=Epidemiol. Infect. |volume=147 |issue= |pages=e106 |date=January 2019 |pmid=30869050 |pmc=6518520 |doi=10.1017/S0950268819000116 |url=}}</ref> | *Following transmission, the [[spirochetes]] replicate [[extracellularly]] and remain predominantly the [[plasma]] space. Some organisms are found within circulating polymorphonuclear cells or [[Reticuloendothelial|reticuloendothelial cell]]s, or occasionally can be found in tissues such as the [[liver]], [[spleen]], [[kidney]], [[heart]], or [[brain]], with foci of perivascular [[inflammation]], [[hemorrhage]], and [[infarction]] at autopsy. Organisms are cleared predominantly by opsonizing [[antibodies]] with the resolution of symptoms ( [[afebrile]] period), followed several days or weeks later by the reemergence of a new [[antigenic]] strain, high-level spirochetemia, when high-level [[spirochetemia]] (104-108 organisms m!) develops, at which time symptoms begin abruptly. During episodes of [[spirochetemia]], the [[organisms]] may invade the brain, eye, inner ear, heart, liver. Splenic [[abscesses]] and infarcts, and hemorrhages within the central nervous system, a perivascular histiocytic interstitial [[myocarditis]], conduction defects, [[arrhythmias]], and [[myocardial]] failure, [[splenic rupture]] with massive hemorrhage, [[cerebral hemorrhage]], and [[hepatic failure]] are seen in LBRF which can result in sudden death.Hepatitis with patchy [[hemorrhages]] and [[necrosis]], [[meningitis]], and [[perisplenitis]], thrombi in small [[vessels]] also are found. [[Thrombi]] are occasionally found occluding [[small vessel]]s.<ref name="pmid30869050">{{cite journal |vauthors=Warrell DA |title=Louse-borne relapsing fever (Borrelia recurrentis infection) |journal=Epidemiol. Infect. |volume=147 |issue= |pages=e106 |date=January 2019 |pmid=30869050 |pmc=6518520 |doi=10.1017/S0950268819000116 |url=}}</ref> | ||
*CNS involvement is more common in TBRF than LBRF, however eschars, ARDS, cranial nerve palsies, focal neurologic deficits, uveitis, iritis or iridocyclitis, splenic rupture and myocarditis may be seen in both TBRF and LBRF.<ref name="pmid18646588">{{cite journal |vauthors=Blevins SM, Greenfield RA, Bronze MS |title=Blood smear analysis in babesiosis, ehrlichiosis, relapsing fever, malaria, and Chagas disease |journal=Cleve Clin J Med |volume=75 |issue=7 |pages=521–30 |date=July 2008 |pmid=18646588 |doi=10.3949/ccjm.75.7.521 |url=}}</ref><ref name="pmid18755384">{{cite journal |vauthors=Dworkin MS, Schwan TG, Anderson DE, Borchardt SM |title=Tick-borne relapsing fever |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=3 |pages=449–68, viii |date=September 2008 |pmid=18755384 |pmc=3725823 |doi=10.1016/j.idc.2008.03.006 |url=}}</ref>Most information on the pathophysiologic aspects of fatal cases comes from autopsy data of louse-borne disease in humans or experimental animals.<ref name="pmid18755384">{{cite journal |vauthors=Dworkin MS, Schwan TG, Anderson DE, Borchardt SM |title=Tick-borne relapsing fever |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=3 |pages=449–68, viii |date=September 2008 |pmid=18755384 |pmc=3725823 |doi=10.1016/j.idc.2008.03.006 |url=}}</ref>. Although [[spirochetes]] are [[pyrogenic]], they probably do not generate detectable [[endotoxins]] or [[exotoxins]]. Organisms are cleared predominantly by opsonizing [[antibodies]] with a resolution of symptoms ( [[afebrile]] period), followed several days or weeks later by the reemergence of a new [[antigenic]] strain, high-level [[spirochetemia]], and recurrence of symptoms. | *CNS involvement is more common in TBRF than LBRF, however eschars, ARDS, cranial nerve palsies, focal neurologic deficits, uveitis, iritis or iridocyclitis, splenic rupture and myocarditis may be seen in both TBRF and LBRF.<ref name="pmid18646588">{{cite journal |vauthors=Blevins SM, Greenfield RA, Bronze MS |title=Blood smear analysis in babesiosis, ehrlichiosis, relapsing fever, malaria, and Chagas disease |journal=Cleve Clin J Med |volume=75 |issue=7 |pages=521–30 |date=July 2008 |pmid=18646588 |doi=10.3949/ccjm.75.7.521 |url=}}</ref><ref name="pmid18755384">{{cite journal |vauthors=Dworkin MS, Schwan TG, Anderson DE, Borchardt SM |title=Tick-borne relapsing fever |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=3 |pages=449–68, viii |date=September 2008 |pmid=18755384 |pmc=3725823 |doi=10.1016/j.idc.2008.03.006 |url=}}</ref>Most information on the pathophysiologic aspects of fatal cases comes from autopsy data of louse-borne disease in humans or experimental animals.<ref name="pmid18755384">{{cite journal |vauthors=Dworkin MS, Schwan TG, Anderson DE, Borchardt SM |title=Tick-borne relapsing fever |journal=Infect. Dis. Clin. North Am. |volume=22 |issue=3 |pages=449–68, viii |date=September 2008 |pmid=18755384 |pmc=3725823 |doi=10.1016/j.idc.2008.03.006 |url=}}</ref>. Although [[spirochetes]] are [[pyrogenic]], they probably do not generate detectable [[endotoxins]] or [[exotoxins]]. Organisms are cleared predominantly by opsonizing [[antibodies]] with a resolution of symptoms ( [[afebrile]] period), followed several days or weeks later by the reemergence of a new [[antigenic]] strain, high-level [[spirochetemia]], and recurrence of symptoms. | ||
*Specific serotypes can recur within an individual. Infection with a given strain of [[Borrelia]] may cause partial protection against subsequent infection by the same strain. In some highly [[endemic]] areas, [[relapsing fever]] is more severe in newcomers than natives. | *Specific serotypes can recur within an individual. Infection with a given strain of [[Borrelia]] may cause partial protection against subsequent infection by the same strain. In some highly [[endemic]] areas, [[relapsing fever]] is more severe in newcomers than natives.<br> | ||
* | The symptoms of Relapsing fever usually develop within 3-7 days after exposure and start with sudden onset of high [[fever]], [[chills]], [[headache]], [[myalgias]], and [[weakness]], followed by afebrile periods. The afebrile interval usually lasts 1 week (up to 60 days) before relapse with symptoms similar to the first episode. Patients with louse-borne relapsing fever will typically have 1-2 relapses (range 0-6) with each subsequent relapse usually less severe than the previous one. Patients with tick-borne relapsing fever usually have 3-5 relapses (range 0-22). Most cases eventually resolve spontaneously. Occasionally, resolution ensues by Crisis. During the crisis, patients may develop cerebral edema with seizures, cardiac failure, or death. This stage may result in death in up to 10% of people.[[Louse-borne relapsing fever]] is more severe than the tick-borne variety. | ||
[[File:Relapsing Fever 2.jpg]] | |||
*sudden onset of high [[fever]], [[chills]], [[headache]], [[myalgias]], and [[weakness]], occur within 3-7 days (up to 18 days) after exposure. Less common symptoms include [[anorexia]], [[nausea]], [[vomiting]], [[abdominal pain]], [[arthralgias]], neck or back pain, [[confusion]], [[lethargy]], cough, [[rash]], sore throat, and swollen lymph nodes. In LBRF, the fever usually lasts 3-6 days and is usually followed by a single, milder episode. In TRBF, multiple episodes of fever occur and each may last up to 3 days. If left untreated, rapid defervescence usually occurs in 2-6 days (range 1-13 days), often with dramatic improvement in symptoms. Chronic relapsing fever may produce a clinical illness analogous to chronic Lyme disease. | |||
'''Crisis''' | |||
* Occasionally, resolution ensues by '''crisis''' which is a classic series of stages that a person will go through: | |||
* 1. Phase one is the chill phase, with the person experiencing high [[fever]]s up to 41.5°C (106.7°F). With this high temperature, a person can develop delirium, agitation, and [[confusion]]. In addition, other signs of an increased [[metabolic rate]] are noted, such as a fast heart rate and breathing rate. This phase lasts between 10 and 30 minutes. | |||
* 2. Phase two is the flush phase. This is where the body temperature decreases rapidly and the person has drenching sweats. During this phase, the person's blood pressure can drop dramatically<ref>http://www.cdc.gov/ncidod/dvbid/RelapsingFever/RF_biology.htm http://www.cdc.gov/ncidod/dvbid/RelapsingFever/index.htmhttp://www.cdc.gov/ncidod/dvbid/RelapsingFever/RF_Symptoms.htm</ref> | |||
*During the crisis, patients may develop cerebral edema with seizures, cardiac failure, or death. This stage may result in death in up to 10% of people. | |||
*After several cycles of fever, some people may develop dramatic central nervous system signs such as seizures, stupor, and coma. The Borrelia organism may also invade heart and liver tissues, causing inflammation of the heart muscle (myocarditis) and liver (hepatitis). Widespread bleeding and pneumonia are other complications. | |||
*The clinical manifestations of tick-borne and louse-borne relapsing fever are similar but can be quite variable, depending on the infecting strain of Borrelia and the host's immunity. Patients typically present 3-7 days (up to 18 days) after exposure with sudden onset of high fever, chills, headache, myalgias, and weakness. | |||
*The afebrile interval usually lasts 1 week (up to 60 days) before relapse with symptoms similar to the first episode. Patients with louse-borne relapsing fever will typically have 1-2 relapses | |||
(range 0-6) with each subsequent relapse usually less severe than the previous one. Patients with tick-borne relapsing fever usually have 3-5 relapses (range 0-22). Most cases eventually resolve spontaneously. Serious complications are more common with louse-borne than tick-borne disease and include iridocyclitis, meningitis, encephalitis, myocarditis, endocarditis, pneumonia, abnormal coagulation with hemorrhage, and spontaneous abortion or transplacental transmission [13]. | |||
[[File:Pathophysiology LBRF.jpg]] | [[File:Pathophysiology LBRF.jpg]] | ||
Revision as of 20:57, 23 September 2020
|
Relapsing fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Relapsing fever pathophysiology On the Web |
|
American Roentgen Ray Society Images of Relapsing fever pathophysiology |
|
Risk calculators and risk factors for Relapsing fever pathophysiology |
keywords:VMP:Variable membrane proteins
Overview
Borrelia is usually transmitted via the tick bite or body louse to the human host. After entering the bloodstream, spirochetes replicate extracellularly and remain predominantly in the plasma space. Patients generally remain asymptomatic until high-level spirochetemia (104-108 organisms m!) develops, at which time symptoms begin abruptly. Organisms are cleared predominantly by opsonizing antibodies with the resolution of symptoms ( afebrile period), followed several days or weeks later by the reemergence of a new antigenic strain, high-level spirochetemia, and recurrence of symptoms. There are multiple genes in the spirochete encoding variable membrane proteins( VMPs). These VMPs determine the antigenic serotype of the organism. At any given time, each spirochete has VMP genes that are expressed and others that are silent. An antigenic switch occurs when a given VMP gene transposes from silent to an expressed locus. This cyclical process of initially effective immune response followed by antigenic variation and immunologic escape is responsible for the relapsing nature of this illness.
Pathophysiology
- Borrelia is usually transmitted via the tick bite or body louse to the human host.
- Following transmission, the spirochetes replicate extracellularly and remain predominantly the plasma space. Some organisms are found within circulating polymorphonuclear cells or reticuloendothelial cells, or occasionally can be found in tissues such as the liver, spleen, kidney, heart, or brain, with foci of perivascular inflammation, hemorrhage, and infarction at autopsy. Organisms are cleared predominantly by opsonizing antibodies with the resolution of symptoms ( afebrile period), followed several days or weeks later by the reemergence of a new antigenic strain, high-level spirochetemia, when high-level spirochetemia (104-108 organisms m!) develops, at which time symptoms begin abruptly. During episodes of spirochetemia, the organisms may invade the brain, eye, inner ear, heart, liver. Splenic abscesses and infarcts, and hemorrhages within the central nervous system, a perivascular histiocytic interstitial myocarditis, conduction defects, arrhythmias, and myocardial failure, splenic rupture with massive hemorrhage, cerebral hemorrhage, and hepatic failure are seen in LBRF which can result in sudden death.Hepatitis with patchy hemorrhages and necrosis, meningitis, and perisplenitis, thrombi in small vessels also are found. Thrombi are occasionally found occluding small vessels.[1]
- CNS involvement is more common in TBRF than LBRF, however eschars, ARDS, cranial nerve palsies, focal neurologic deficits, uveitis, iritis or iridocyclitis, splenic rupture and myocarditis may be seen in both TBRF and LBRF.[2][3]Most information on the pathophysiologic aspects of fatal cases comes from autopsy data of louse-borne disease in humans or experimental animals.[3]. Although spirochetes are pyrogenic, they probably do not generate detectable endotoxins or exotoxins. Organisms are cleared predominantly by opsonizing antibodies with a resolution of symptoms ( afebrile period), followed several days or weeks later by the reemergence of a new antigenic strain, high-level spirochetemia, and recurrence of symptoms.
- Specific serotypes can recur within an individual. Infection with a given strain of Borrelia may cause partial protection against subsequent infection by the same strain. In some highly endemic areas, relapsing fever is more severe in newcomers than natives.
The symptoms of Relapsing fever usually develop within 3-7 days after exposure and start with sudden onset of high fever, chills, headache, myalgias, and weakness, followed by afebrile periods. The afebrile interval usually lasts 1 week (up to 60 days) before relapse with symptoms similar to the first episode. Patients with louse-borne relapsing fever will typically have 1-2 relapses (range 0-6) with each subsequent relapse usually less severe than the previous one. Patients with tick-borne relapsing fever usually have 3-5 relapses (range 0-22). Most cases eventually resolve spontaneously. Occasionally, resolution ensues by Crisis. During the crisis, patients may develop cerebral edema with seizures, cardiac failure, or death. This stage may result in death in up to 10% of people.Louse-borne relapsing fever is more severe than the tick-borne variety.

- sudden onset of high fever, chills, headache, myalgias, and weakness, occur within 3-7 days (up to 18 days) after exposure. Less common symptoms include anorexia, nausea, vomiting, abdominal pain, arthralgias, neck or back pain, confusion, lethargy, cough, rash, sore throat, and swollen lymph nodes. In LBRF, the fever usually lasts 3-6 days and is usually followed by a single, milder episode. In TRBF, multiple episodes of fever occur and each may last up to 3 days. If left untreated, rapid defervescence usually occurs in 2-6 days (range 1-13 days), often with dramatic improvement in symptoms. Chronic relapsing fever may produce a clinical illness analogous to chronic Lyme disease.
Crisis
- Occasionally, resolution ensues by crisis which is a classic series of stages that a person will go through:
- 1. Phase one is the chill phase, with the person experiencing high fevers up to 41.5°C (106.7°F). With this high temperature, a person can develop delirium, agitation, and confusion. In addition, other signs of an increased metabolic rate are noted, such as a fast heart rate and breathing rate. This phase lasts between 10 and 30 minutes.
- 2. Phase two is the flush phase. This is where the body temperature decreases rapidly and the person has drenching sweats. During this phase, the person's blood pressure can drop dramatically[4]
- During the crisis, patients may develop cerebral edema with seizures, cardiac failure, or death. This stage may result in death in up to 10% of people.
- After several cycles of fever, some people may develop dramatic central nervous system signs such as seizures, stupor, and coma. The Borrelia organism may also invade heart and liver tissues, causing inflammation of the heart muscle (myocarditis) and liver (hepatitis). Widespread bleeding and pneumonia are other complications.
- The clinical manifestations of tick-borne and louse-borne relapsing fever are similar but can be quite variable, depending on the infecting strain of Borrelia and the host's immunity. Patients typically present 3-7 days (up to 18 days) after exposure with sudden onset of high fever, chills, headache, myalgias, and weakness.
- The afebrile interval usually lasts 1 week (up to 60 days) before relapse with symptoms similar to the first episode. Patients with louse-borne relapsing fever will typically have 1-2 relapses
(range 0-6) with each subsequent relapse usually less severe than the previous one. Patients with tick-borne relapsing fever usually have 3-5 relapses (range 0-22). Most cases eventually resolve spontaneously. Serious complications are more common with louse-borne than tick-borne disease and include iridocyclitis, meningitis, encephalitis, myocarditis, endocarditis, pneumonia, abnormal coagulation with hemorrhage, and spontaneous abortion or transplacental transmission [13].
Genetics
The development of the cyclical process is the result of antigenic variation and subsequent immunologic escape:
- There are multiple genes in the spirochete encoding variable membrane proteins( VMPs) which are the outer membrane of spirochetes contains surface proteins. Attacks of relapsing fever end abruptly when specific bactericidal immunoglobulin M antibodies generated by the B1b cell subset lyse spirochaetes in the blood, independently of complement and T cells. These VMPs determine the antigenic serotype of the organism and at any given time, each spirochete has VMP genes that are expressed and others that are silent. An antigenic switch occurs when a given VMP gene transposes from silent to an expressed locus. This mechanism of antigenic variation presumably leads to immunologic escape and relapse. Because of the organism’s ability to undergo antigenic variation, several serotypes may be present in the bloodstream at one time.
References
- ↑ Warrell DA (January 2019). "Louse-borne relapsing fever (Borrelia recurrentis infection)". Epidemiol. Infect. 147: e106. doi:10.1017/S0950268819000116. PMC 6518520 Check
|pmc=value (help). PMID 30869050. - ↑ Blevins SM, Greenfield RA, Bronze MS (July 2008). "Blood smear analysis in babesiosis, ehrlichiosis, relapsing fever, malaria, and Chagas disease". Cleve Clin J Med. 75 (7): 521–30. doi:10.3949/ccjm.75.7.521. PMID 18646588.
- ↑ 3.0 3.1 Dworkin MS, Schwan TG, Anderson DE, Borchardt SM (September 2008). "Tick-borne relapsing fever". Infect. Dis. Clin. North Am. 22 (3): 449–68, viii. doi:10.1016/j.idc.2008.03.006. PMC 3725823. PMID 18755384.
- ↑ http://www.cdc.gov/ncidod/dvbid/RelapsingFever/RF_biology.htm http://www.cdc.gov/ncidod/dvbid/RelapsingFever/index.htmhttp://www.cdc.gov/ncidod/dvbid/RelapsingFever/RF_Symptoms.htm