Sandbox:Sahar: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
==Images== | ==Images== | ||
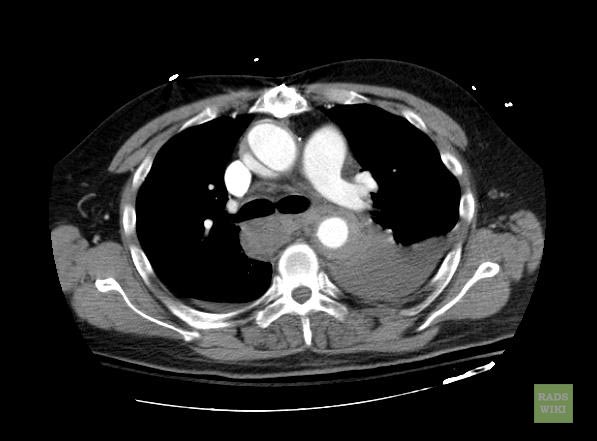
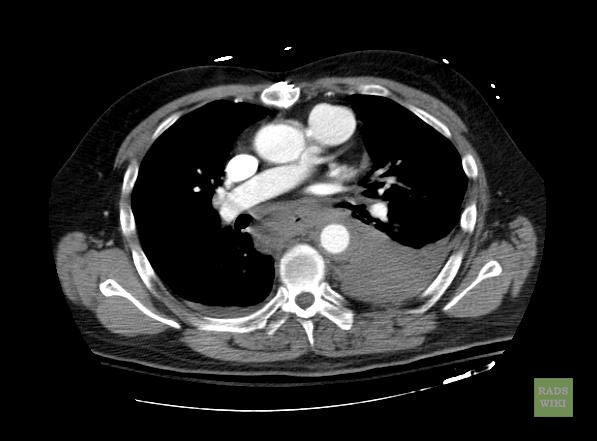
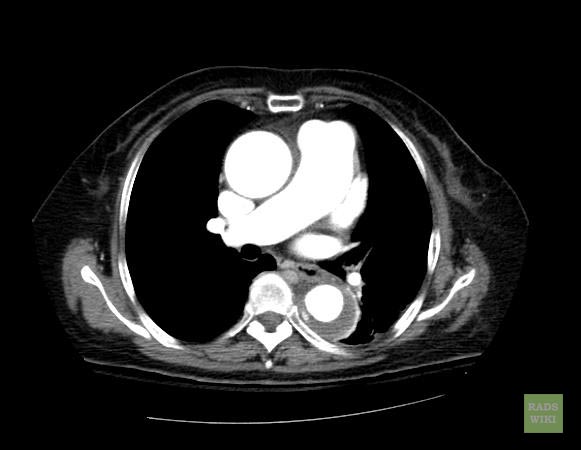
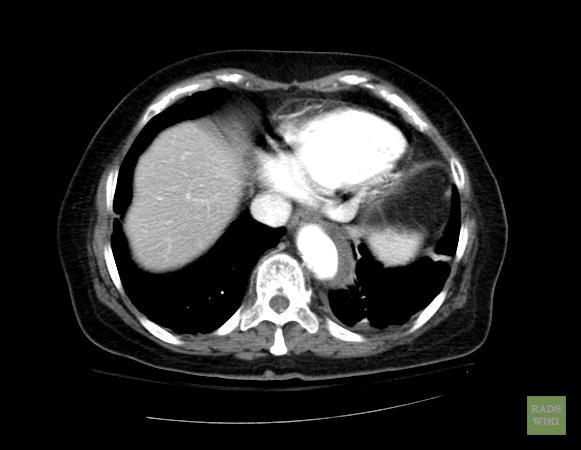
[[Image:Intramural-hematoma-006.jpg|thumb|350px|left|Contrast enhanced CT: Aortic intramural hematoma, Courtesy of radiopaedia]] | [[Image:Intramural-hematoma-006.jpg|thumb|350px|left|Contrast enhanced CT: Aortic intramural hematoma, Courtesy of radiopaedia]] | ||
<br clear="left" /> | <br clear="left" /> | ||
| Line 24: | Line 16: | ||
* [http://www.ajronline.org/cgi/content/short/181/2/309 Macura, Katarzyna J., Corl, Frank M., Fishman, Elliot K., Bluemke, David A. Pathogenesis in Acute Aortic Syndromes: Aortic Dissection, Intramural Hematoma, and Penetrating Atherosclerotic Aortic Ulcer. Am. J. Roentgenol. 2003 181: 309-316.] | * [http://www.ajronline.org/cgi/content/short/181/2/309 Macura, Katarzyna J., Corl, Frank M., Fishman, Elliot K., Bluemke, David A. Pathogenesis in Acute Aortic Syndromes: Aortic Dissection, Intramural Hematoma, and Penetrating Atherosclerotic Aortic Ulcer. Am. J. Roentgenol. 2003 181: 309-316.] | ||
* [http://www.emedicine.com/radio/topic43.htm Gomez-Jorge, Jackeline. E-medicine rads article] | * [http://www.emedicine.com/radio/topic43.htm Gomez-Jorge, Jackeline. E-medicine rads article] | ||
{| border="3" | {| border="3" | ||
| Line 113: | Line 23: | ||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG Characteristics}} | ! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG Characteristics}} | ||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG view}} | ! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG view}} | ||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC; " align="left"|Ventricular tachycardia | ! style="padding: 5px 5px; background: #DCDCDC; " align="left"| Ventricular tachycardia | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC; " align="left"|Ventricular fibrillation | ! style="padding: 5px 5px; background: #DCDCDC; " align="left"| Ventricular fibrillation | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Asystole | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Asystole | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Pulseless electrical activity | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Pulseless electrical activity<ref name=ACLS_2003_H_T>''ACLS: Principles and Practice''. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.</ref><ref name=ACLS_2003_EP_HT>''ACLS for Experienced Providers''. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.</ref><ref name="ECC_2005_7.2">"2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." ''Circulation'' 2005; '''112''': IV-58 - IV-66.</ref><ref>Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007</ref> | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
*Hypovolemia | |||
*Hypoxia | |||
*Hydrogen ions (Acidosis) | |||
*Hypothermia | |||
*Hyperkalemia or Hypokalemia | |||
*Hypoglycemia | |||
*Tablets or Toxins (Drug overdose) such as beta blockers, tricyclic antidepressants, or calcium channel blockers | |||
*Tamponade | |||
*Tension pneumothorax | |||
*Thrombosis (Myocardial infarction) | |||
*Thrombosis (Pulmonary embolism) | |||
*Trauma (Hypovolemia from blood loss) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
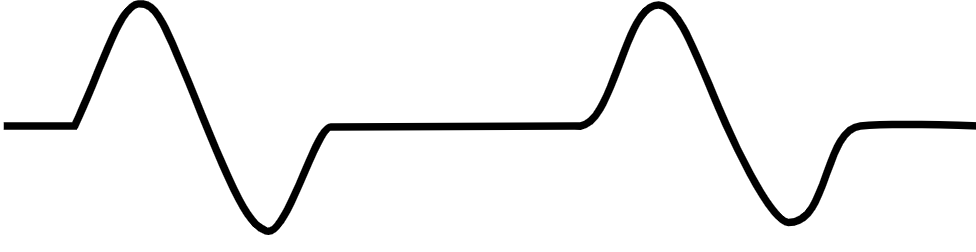
*Several ppattern are possible including: | |||
**Normal sinus rhythm | |||
**Sinus tachycardia, with discernible P waves and QRS complexes | |||
**Bradycardia, with or without P waves | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
[[File:Capture PEA.PNG|center|300px]] | |||
|- | |- | ||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |Pulmonary embolism | ! style="padding: 5px 5px; background: #DCDCDC;" align="left" | Pulmonary embolism | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* | |||
|} | |} | ||
<references /> | <references /> | ||
Revision as of 19:33, 28 January 2020
Images


- Macura, Katarzyna J., Corl, Frank M., Fishman, Elliot K., Bluemke, David A. Pathogenesis in Acute Aortic Syndromes: Aortic Dissection, Intramural Hematoma, and Penetrating Atherosclerotic Aortic Ulcer. Am. J. Roentgenol. 2003 181: 309-316.
- Gomez-Jorge, Jackeline. E-medicine rads article
| Disease Name | Causes | ECG Characteristics | ECG view |
|---|---|---|---|
| Ventricular tachycardia |
|
|
|
| Ventricular fibrillation |
|
|
|
| Asystole |
|
|
|
| Pulseless electrical activity[1][2][3][4] |
|
|
 |
| Pulmonary embolism |
|
|
|
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
- ↑ Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | ECG view |
|---|---|---|---|---|---|---|---|---|---|