Tabes Dorsalis physical examination: Difference between revisions
No edit summary |
No edit summary |
||
| Line 58: | Line 58: | ||
===Skin=== | ===Skin=== | ||
* In patients with tabes dorsalis some granulomatous skin lesions may be seen called gumma. Gummas, are granulomatous reactions to long-term smoldering infection with Treponema pallidum and its residual antigens. | * In patients with tabes dorsalis some granulomatous skin lesions may be seen called gumma. Gummas, are granulomatous reactions to long-term smoldering infection with Treponema pallidum and its residual antigens. | ||
*[[Jaundice]] may be seen. | *[[Jaundice]] may be seen. | ||
</ | [[Image:Tertiary syphilis gumma.JPG|500px|thumb|center|Tertiary syphilis gumma <br> Source:By NearEMPTiness (Wie Schönes Wissen schafft im MUT) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons, rID: 51340]] | ||
===HEENT=== | ===HEENT=== | ||
Revision as of 18:54, 30 January 2018
|
Tabes Dorsalis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tabes Dorsalis physical examination On the Web |
|
American Roentgen Ray Society Images of Tabes Dorsalis physical examination |
|
Risk calculators and risk factors for Tabes Dorsalis physical examination |
Physical Examination
Physical examination may show:
- Damage to the spinal cord (myelopathy)
- Pupils that react abnormally to light
- Reduced or absent reflexes due to nerve damage
References
s s s s
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Mohamadmostafa Jahansouz M.D.[2]
Overview
Patients with [disease name] usually appear [general appearance]. Physical examination of patients with [disease name] is usually remarkable for [finding 1], [finding 2], and [finding 3].
OR
Common physical examination findings of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
The presence of [finding(s)] on physical examination is diagnostic of [disease name].
OR
The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Physical Examination
- Physical examination of patients with [disease name] is usually normal.
OR
- Physical examination of patients with [disease name] is usually remarkable for:[finding 1], [finding 2], and [finding 3].
- The presence of [finding(s)] on physical examination is diagnostic of [disease name].
- The presence of [finding(s)] on physical examination is highly suggestive of [disease name].
Appearance of the Patient
- Patients with [disease name] usually appear [general appearance].
Vital Signs
- Usually vital ital signs are normal in tabes dorsal.
Skin
- In patients with tabes dorsalis some granulomatous skin lesions may be seen called gumma. Gummas, are granulomatous reactions to long-term smoldering infection with Treponema pallidum and its residual antigens.
- Jaundice may be seen.
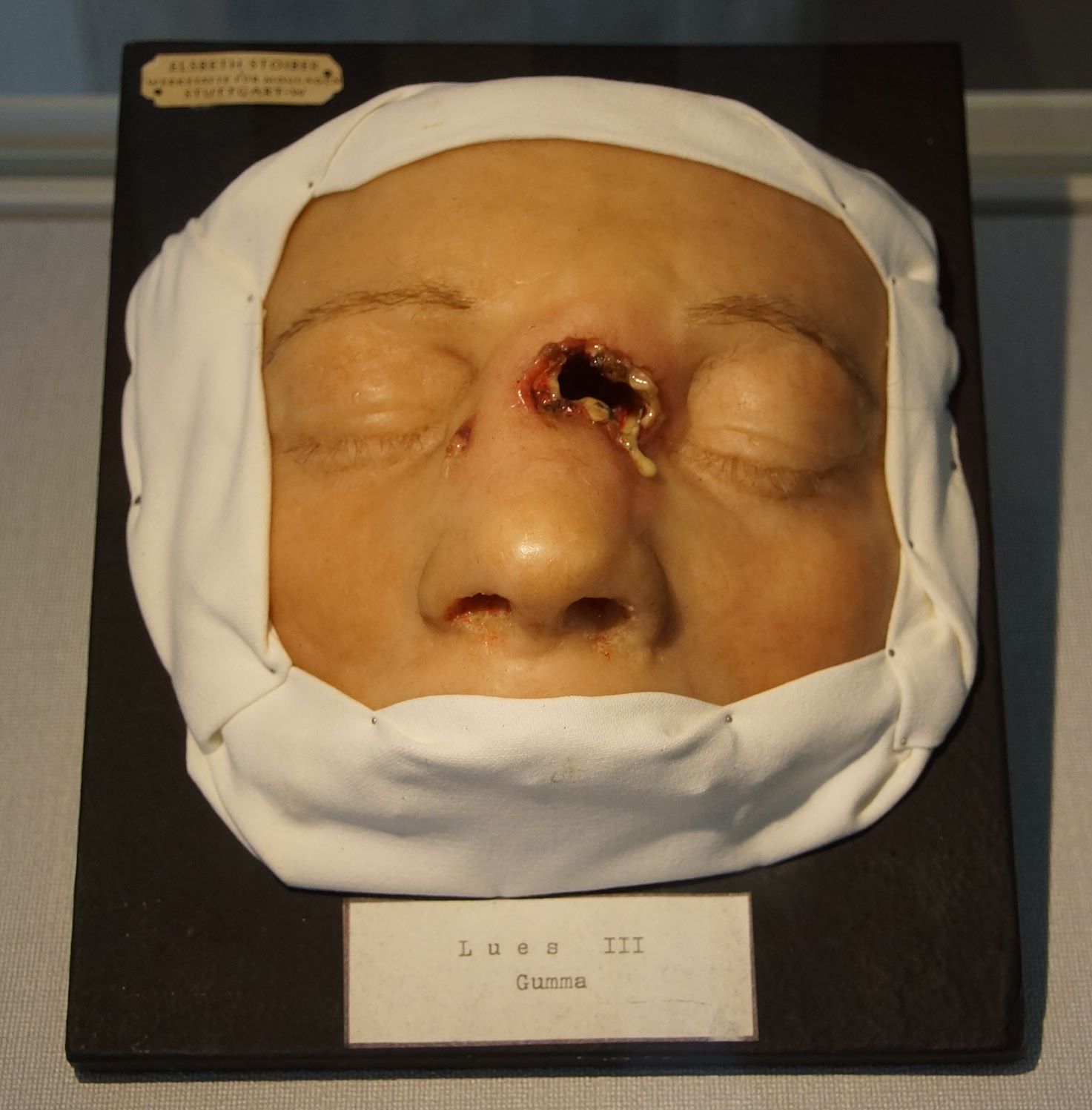
Source:By NearEMPTiness (Wie Schönes Wissen schafft im MUT) [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], via Wikimedia Commons, rID: 51340
HEENT
- HEENT examination of patients with [disease name] is usually normal.
OR
- Abnormalities of the head/hair may include ___
- Evidence of trauma
- Icteric sclera
- Nystagmus
- Extra-ocular movements may be abnormal
- Pupils non-reactive to light / non-reactive to accommodation / non-reactive to neither light nor accommodation
- Ophthalmoscopic exam may be abnormal with findings of ___
- Hearing acuity may be reduced
- Weber test may be abnormal (Note: A positive Weber test is considered a normal finding / A negative Weber test is considered an abnormal finding. To avoid confusion, you may write "abnormal Weber test".)
- Rinne test may be positive (Note: A positive Rinne test is considered a normal finding / A negative Rinne test is considered an abnormal finding. To avoid confusion, you may write "abnormal Rinne test".)
- Exudate from the ear canal
- Tenderness upon palpation of the ear pinnae/tragus (anterior to ear canal)
- Inflamed nares / congested nares
- Purulent exudate from the nares
- Facial tenderness
- Erythematous throat with/without tonsillar swelling, exudates, and/or petechiae
Neck
- Neck examination of patients with [disease name] is usually normal.
OR
- Jugular venous distension
- Carotid bruits may be auscultated unilaterally/bilaterally using the bell/diaphragm of the otoscope
- Lymphadenopathy (describe location, size, tenderness, mobility, and symmetry)
- Thyromegaly / thyroid nodules
- Hepatojugular reflux
Lungs
- Pulmonary examination of patients with [disease name] is usually normal.
OR
- Asymmetric chest expansion / Decreased chest expansion
- Lungs are hypo/hyperresonant
- Fine/coarse crackles upon auscultation of the lung bases/apices unilaterally/bilaterally
- Rhonchi
- Vesicular breath sounds / Distant breath sounds
- Expiratory/inspiratory wheezing with normal / delayed expiratory phase
- Wheezing may be present
- Egophony present/absent
- Bronchophony present/absent
- Normal/reduced tactile fremitus
Heart
- Cardiovascular examination of patients with [disease name] is usually normal.
OR
- Chest tenderness upon palpation
- PMI within 2 cm of the sternum (PMI) / Displaced point of maximal impulse (PMI) suggestive of ____
- Heave / thrill
- Friction rub
- S1
- S2
- S3
- S4
- Gallops
- A high/low grade early/late systolic murmur / diastolic murmur best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the otoscope
Abdomen
Abdominal examination of patients with [disease name] is usually normal.
OR
- Abdominal distention
- Abdominal tenderness in the right/left upper/lower abdominal quadrant
- Rebound tenderness (positive Blumberg sign)
- A palpable abdominal mass in the right/left upper/lower abdominal quadrant
- Guarding may be present
- Hepatomegaly / splenomegaly / hepatosplenomegaly
- Additional findings, such as obturator test, psoas test, McBurney point test, Murphy test
Back
- Back examination of patients with [disease name] is usually normal.
OR
- Point tenderness over __ vertebrae (e.g. L3-L4)
- Sacral edema
- Costovertebral angle tenderness bilaterally/unilaterally
- Buffalo hump
Genitourinary
- Genitourinary examination of patients with [disease name] is usually normal.
OR
- A pelvic/adnexal mass may be palpated
- Inflamed mucosa
- Clear/(color), foul-smelling/odorless penile/vaginal discharge
Neuromuscular
- Neuromuscular examination of patients with [disease name] is usually normal.
OR
- Patient is usually oriented to persons, place, and time
- Altered mental status
- Glasgow coma scale is ___ / 15
- Clonus may be present
- Hyperreflexia / hyporeflexia / areflexia
- Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally
- Muscle rigidity
- Proximal/distal muscle weakness unilaterally/bilaterally
- ____ (finding) suggestive of cranial nerve ___ (roman numerical) deficit (e.g. Dilated pupils suggestive of CN III deficit)
- Unilateral/bilateral upper/lower extremity weakness
- Unilateral/bilateral sensory loss in the upper/lower extremity
- Positive straight leg raise test
- Abnormal gait (describe gait: e.g. ataxic (cerebellar) gait / steppage gait / waddling gait / choeiform gait / Parkinsonian gait / sensory gait)
- Positive/negative Trendelenburg sign
- Unilateral/bilateral tremor (describe tremor, e.g. at rest, pill-rolling)
- Normal finger-to-nose test / Dysmetria
- Absent/present dysdiadochokinesia (palm tapping test)
Extremities
- Extremities examination of patients with [disease name] is usually normal.
OR
- Clubbing
- Cyanosis
- Pitting/non-pitting edema of the upper/lower extremities
- Muscle atrophy
- Fasciculations in the upper/lower extremity