Goodpasture syndrome pathophysiology: Difference between revisions
| Line 9: | Line 9: | ||
== Genetics == | == Genetics == | ||
There is | There is strong correlation of anti-glomerular basement membrane disease with allele HLA DRB1-1501. This allele is associated in causing renal injury. <ref name="pmid26200622">{{cite journal| author=Xie LJ, Cui Z, Jia XY, Chen Z, Liu XR, Zhao MH| title=Coexistence of Anti-Glomerular Basement Membrane Antibodies and Anti-Neutrophil Cytoplasmic Antibodies in a Child With Human Leukocyte Antigen Susceptibility and Detailed Antibody Description: A Case Report. | journal=Medicine (Baltimore) | year= 2015 | volume= 94 | issue= 29 | pages= e1179 | pmid=26200622 | doi=10.1097/MD.0000000000001179 | pmc=4603008 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26200622 }}</ref> This allele is present in 80% of patients with Goodpasture syndrome.<ref name="pmid27049372">{{cite journal| author=Couser WG| title=Pathogenesis and treatment of glomerulonephritis-an update. | journal=J Bras Nefrol | year= 2016 | volume= 38 | issue= 1 | pages= 107-22 | pmid=27049372 | doi=10.5935/0101-2800.20160016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27049372 }}</ref> | ||
== Associated Conditions == | == Associated Conditions == | ||
Revision as of 21:43, 2 November 2016
|
Goodpasture syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Goodpasture syndrome pathophysiology On the Web |
|
American Roentgen Ray Society Images of Goodpasture syndrome pathophysiology |
|
Risk calculators and risk factors for Goodpasture syndrome pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Ali Poyan Mehr, M.D. [2]Associate Editor(s)-in-Chief: Krzysztof Wierzbicki M.D. [3]
Overview
Pathogenesis
The pathogenesis of Goodpasture syndrome is the presence of autoantibodies against the glomerular or alveolar basement membranes. The target antigen that has the strongest pathogenic effect on anti-GBM disease is the non-collagenous 1 domain of alpha-3 type IV collagen.[1] There are 2 dominant epitopes, they are epitope A and epitope B. These epitopes are seen in the alpha-3 non-collagenous 1 domain of type IV collagen and antibodies do not normally bind unless a change has occurred in the non-cross linked hexamers or trimers. In Goodpasture syndrome these epitopes undergo a transitional change in the non-cross linked hexamers or trimers. This allows antibodies to be bound to the epitopes. The pathogenic role of epitopes such as epitope A, has been shown to affect the function of the renals, especially of the alpha-3 type IV collagen of non-collagenous 1 domain. Epitope B however is not able to induce Goodpasture syndrome by itself.[2] The cause of renal injury is due to anti-glomerular basement membrane antibodies ability to bind and activate complements and proteases. This processes causes an interruption between the filtration barrier and the Bowman’s capsule to occur. When the filtration barrier and the Bowman's capsule are interrupted, this process induces a crescent formation of the renal as well as proteinuria. Injury to the renal induces T cells (CD4+ and CD8+), macrophages, and neutrophils.[3]
Factors that are associated with these process are due to oxidation, nitrosylation, glycation, increases in body temperature, or proteolytic cleavage. For example, it has been shown that proteolytic cleavage of disulfide bonds in non-cross linked hexamers has shown greater affinity for Goodpasture syndrome antibodies to bind. Environmental factors are also said to attribute to the disease such as exposures to hydrocarbons, exposure to formaldehyde or smoking tobacco. Smoking tobacco for instance causes sulfilimine bond substances to be inhibited. Inhibition of the sulfilimine bond substances cause non-cross linked hexamers to form.[4]
Genetics
There is strong correlation of anti-glomerular basement membrane disease with allele HLA DRB1-1501. This allele is associated in causing renal injury. [5] This allele is present in 80% of patients with Goodpasture syndrome.[6]
Associated Conditions
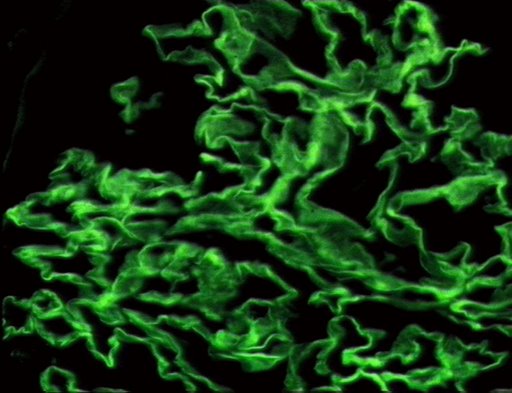
Gross Pathology
Macroscopic Pathology
Pathophysiology
As with many autoimmune conditions, the precise cause of Goodpasture’s Syndrome is not yet known. It is believed to be a type II hypersensitivity reaction to Goodpasture’s antigens on the cells of the glomeruli of the kidneys and the pulmonary alveoli, specifically the basement membrane's (including a-3 chain of type IV collagen), whereby the immune system wrongly recognizes these cells as foreign and attacks and destroys them, as it would an invading pathogen.
Pathology
References
- ↑ Zhao J, Cui Z, Yang R, Jia XY, Zhang Y, Zhao MH (2009). "Anti-glomerular basement membrane autoantibodies against different target antigens are associated with disease severity". Kidney Int. 76 (10): 1108–15. doi:10.1038/ki.2009.348. PMID 19741587.
- ↑ Chen JL, Hu SY, Jia XY, Zhao J, Yang R, Cui Z; et al. (2013). "Association of epitope spreading of antiglomerular basement membrane antibodies and kidney injury". Clin J Am Soc Nephrol. 8 (1): 51–8. doi:10.2215/CJN.05140512. PMC 3531658. PMID 23085731.
- ↑ Hudson BG, Tryggvason K, Sundaramoorthy M, Neilson EG (2003). "Alport's syndrome, Goodpasture's syndrome, and type IV collagen". N Engl J Med. 348 (25): 2543–56. doi:10.1056/NEJMra022296. PMID 12815141.
- ↑ Pedchenko V, Bondar O, Fogo AB, Vanacore R, Voziyan P, Kitching AR; et al. (2010). "Molecular architecture of the Goodpasture autoantigen in anti-GBM nephritis". N Engl J Med. 363 (4): 343–54. doi:10.1056/NEJMoa0910500. PMC 4144421. PMID 20660402.
- ↑ Xie LJ, Cui Z, Jia XY, Chen Z, Liu XR, Zhao MH (2015). "Coexistence of Anti-Glomerular Basement Membrane Antibodies and Anti-Neutrophil Cytoplasmic Antibodies in a Child With Human Leukocyte Antigen Susceptibility and Detailed Antibody Description: A Case Report". Medicine (Baltimore). 94 (29): e1179. doi:10.1097/MD.0000000000001179. PMC 4603008. PMID 26200622.
- ↑ Couser WG (2016). "Pathogenesis and treatment of glomerulonephritis-an update". J Bras Nefrol. 38 (1): 107–22. doi:10.5935/0101-2800.20160016. PMID 27049372.
- ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages