Escherichia coli enteritis medical therapy: Difference between revisions
YazanDaaboul (talk | contribs) |
YazanDaaboul (talk | contribs) |
||
| Line 22: | Line 22: | ||
*Since the majority of cases of ''E. coli'' enteritis are self-limited and the exact infective strain is often not identified, empiric antimicrobial therapy is generally not recommended. | *Since the majority of cases of ''E. coli'' enteritis are self-limited and the exact infective strain is often not identified, empiric antimicrobial therapy is generally not recommended. | ||
*Antimicrobial therapy using either [[TMP-SMX]] or [[fluoroquinolone]] may be administered (but is not required) in ETEC infection (traveler's diarrhea), EPEC infection, and EIEC infection. | *Antimicrobial therapy using either [[TMP-SMX]] or [[fluoroquinolone]] may be administered (but is not required) in ETEC infection (traveler's diarrhea), EPEC infection, and EIEC infection. | ||
*In contrast, antimicrobial therapy is NOT recommended in EHEC (STEC or VTEC) infections due to possibly increased risk of hemolytic uremic syndrome and prolonged shedding of the organism and production of | *In contrast, antimicrobial therapy is NOT recommended in EHEC (STEC or VTEC) infections due to possibly increased risk of [[hemolytic uremic syndrome]] and prolonged shedding of the organism and production of enterotoxins. | ||
===Other Pharmacologic Agents=== | ===Other Pharmacologic Agents=== | ||
| Line 37: | Line 37: | ||
:::*'''1.4. Enterohemorrhagic ''E. coli'' (EHEC)''' | :::*'''1.4. Enterohemorrhagic ''E. coli'' (EHEC)''' | ||
::::*Preferred regimen: Antibiotic therapy is not recommended due to possibly increased risk of hemolytic uremic syndrome and prolonged shedding. | ::::*Preferred regimen: Antibiotic therapy is not recommended due to possibly increased risk of hemolytic uremic syndrome and prolonged shedding. | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
Revision as of 16:21, 22 December 2015
|
Escherichia coli enteritis Microchapters |
|
Differentiating Escherichia coli enteritis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Escherichia coli enteritis medical therapy On the Web |
|
American Roentgen Ray Society Images of Escherichia coli enteritis medical therapy |
|
Risk calculators and risk factors for Escherichia coli enteritis medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Yazan Daaboul, M.D.; Serge Korjian M.D.
Overview
Rehydration is the mainstay of therapy of E. coli enteritis. Oral rehydration fluids (e.g. oral rehydration solutions) are indicated among patients who can tolerate oral intake, otherwise IV rehydration is indicated. Since the majority of cases of E. coli enteritis are self-limited and the exact infective strain is often not identified, empiric antimicrobial therapy is generally not recommended. Antimicrobial therapy using either fluoroquinolone or TMP-SMX may be administered (but is not required) in ETEC infection (traveler's diarrhea), EPEC infection, and EIEC infection, but not in EHEC infection (due to increased risk of hemolytic uremic syndrome and prolonged shedding). In adults, additional pharmacologic therapies may include antiemetic agents (not recommended in pediatric patients). Antidiarrheal agents are generally not recommended during the acute infection phase.
Medical Therapy
Rehydration
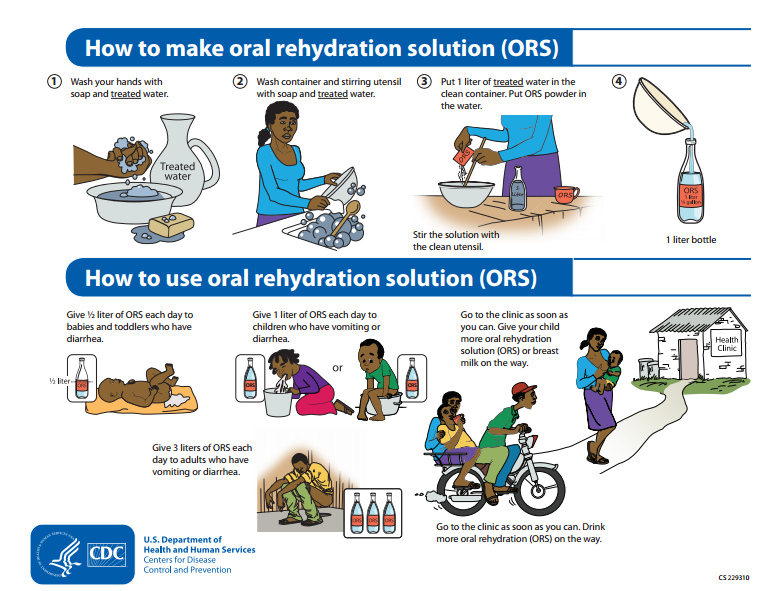
- The mainstay of therapy for E. coli enteritis is rehydration.
- Oral rehydration fluids are indicated among patients who can tolerate oral intake, otherwise IV rehydration is indicated.
- Over the counter oral rehydration solutions (ORS) are optimal options for oral rehydration and are usually available for both adults and children.
- Oral rehydration solutions may be home-made by mixing the following:
- Drinking water: 1 liter
- Salt: 0.5 teaspoon
- Sugar: 6 teaspoons
- Rehydration must be gradual until signs of dehydration (e.g. dry mouth, oliguria) are resolved. Drinking ORS must be slow (1 sip every 5 minutes).
- Children often require 1 liter of ORS, whereas adults often require 3 liters of ORS.
- Energy drinks with high concentrations of electrolytes (e.g. sports drinks) may be offered to adults, but not children.
- Fluids high in sugar content (e.g. soda) are not recommended because they may worsen the dehydration.
Antimicrobial Therapy
- Since the majority of cases of E. coli enteritis are self-limited and the exact infective strain is often not identified, empiric antimicrobial therapy is generally not recommended.
- Antimicrobial therapy using either TMP-SMX or fluoroquinolone may be administered (but is not required) in ETEC infection (traveler's diarrhea), EPEC infection, and EIEC infection.
- In contrast, antimicrobial therapy is NOT recommended in EHEC (STEC or VTEC) infections due to possibly increased risk of hemolytic uremic syndrome and prolonged shedding of the organism and production of enterotoxins.
Other Pharmacologic Agents
- 1. Escherichia coli species
- 1.1. Enterotoxigenic E. coli (ETEC)
- Preferred regimen: TMP-SMX, 160 and 800 mg, respectively, bid, for 3-7 days (if susceptible) OR Fluoroquinolone (e.g., 300 mg Ofloxacin, 400 mg Norfloxacin, or 500 mg Ciprofloxacin bid for 3-7 days)
- 1.2. Enteropathogenic E. coli (EPEC)
- Preferred regimen: TMP-SMX, 160 and 800 mg, respectively, bid, for 3-7 days (if susceptible) OR Fluoroquinolone (e.g., 300 mg Ofloxacin, 400 mg Norfloxacin, or 500 mg Ciprofloxacin bid for 3-7 days)
- 1.3. Enteroinvasive E. coli (EIEC)
- Preferred regimen: TMP-SMX, 160 and 800 mg, respectively, bid, for 3-7 days (if susceptible) OR Fluoroquinolone (e.g., 300 mg Ofloxacin, 400 mg Norfloxacin, or 500 mg Ciprofloxacin bid for 3-7 days)
- 1.4. Enterohemorrhagic E. coli (EHEC)
- Preferred regimen: Antibiotic therapy is not recommended due to possibly increased risk of hemolytic uremic syndrome and prolonged shedding.