Rheumatic fever pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 32: | Line 32: | ||
Image:Rheumatic fever 004.jpg|Aschoff bodies in rheumatic heart disease | Image:Rheumatic fever 004.jpg|Aschoff bodies in rheumatic heart disease | ||
Image:ARF mitral valve.jpg|Rheumatic Mitral Valvulitis: Gross; an excellent example of acute rheumatic fever lesion along line of closure of mitral valve | |||
</gallery> | </gallery> | ||
Revision as of 17:54, 12 October 2015
|
Rheumatic fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Rheumatic fever pathophysiology On the Web |
|
American Roentgen Ray Society Images of Rheumatic fever pathophysiology |
|
Risk calculators and risk factors for Rheumatic fever pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Lance Christiansen, D.O.; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2] Anthony Gallo, B.S. [3]
Pathophysiology
Rheumatic fever is the result of an autoimmunological sequela to a virulent Streptococcus pyogenes infection in a patient who was immunologically sensitized from prior infections. The systemic disease affects the periarteriolar connective tissue and can occur after an untreated Group A streptococcal pharyngeal infection. It is believed to be caused by antibody cross-reactivity which is a Type II hypersensitivity reaction, often termed molecular mimicry.
Usually, self reactive B cells remain anergic in the periphery without T cell co-stimulation. During a streptococcal infection, activated antigen presenting cells, such as macrophages, present the bacterial antigen to helper T cells. Helper T cells subsequently activate B cells and induce the production of antibodies against the cell wall of streptococcus. However the antibodies may also act against the myocardium and joints, producing the symptoms of rheumatic fever.
Contrary to the immunological protection developed during most infections, infections by Streptococcus pyogenes cause both a protective immunological and pathological autoimmunological stimulation. Repeated infections by Streptococcus pyogenes will cause both a heightened protective and pathological immune response. The immune response helps in combating the streptococcal infection. However, the autoimmunological response causes an inflammatory, systemic, disease process, rheumatic fever.
Group A streptococcus pyogenes have a cell wall composed of branched polymers which sometimes contain M proteins that are highly antigenic. The antibodies which the immune system generates against the M proteins may cross-react with cardiac myofiber sarcolemma and smooth muscle cells of arteries, inducing cytokine r
In acute rheumatic fever, these lesions may occur in endocardium, myocardium or pericardium. The inflammation may cause a serofibrinous pericardial exudates described as “bread-and-butter” pericarditis, which usually resolves without sequelae. Involvement of the endocardium typically results in fibrinoid necrosis and verrucae formation along the lines of closure of the left heart valves. Warty projections arise from the deposition, while subendothelial lesions may induce irregular thickenings called MacCallum plaques.
Pathological Findings
-
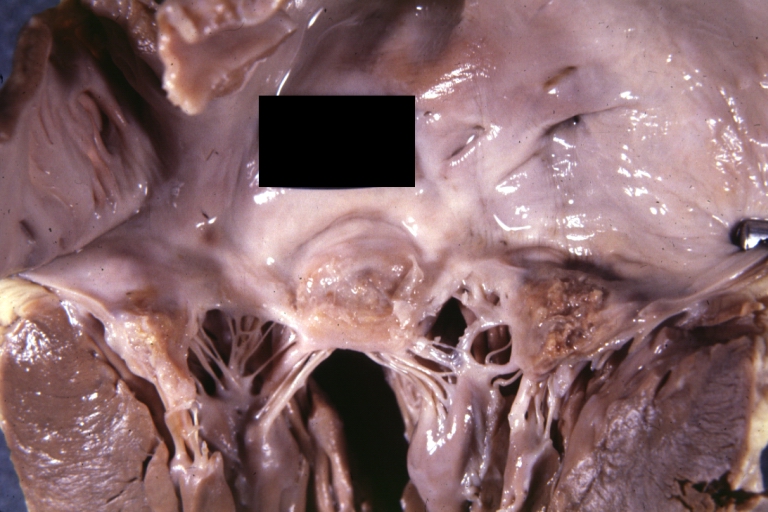
Aortic Stenosis (Tricuspid aorta): Gross, good example of aortic stenosis due to rheumatic fever
-
Gross, an excellent example of mitral scarring due to rheumatic fever (healing phase of an infectious lesion).
-
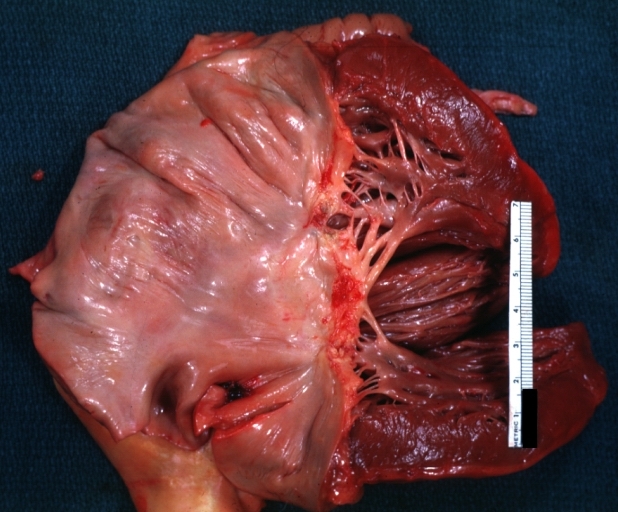
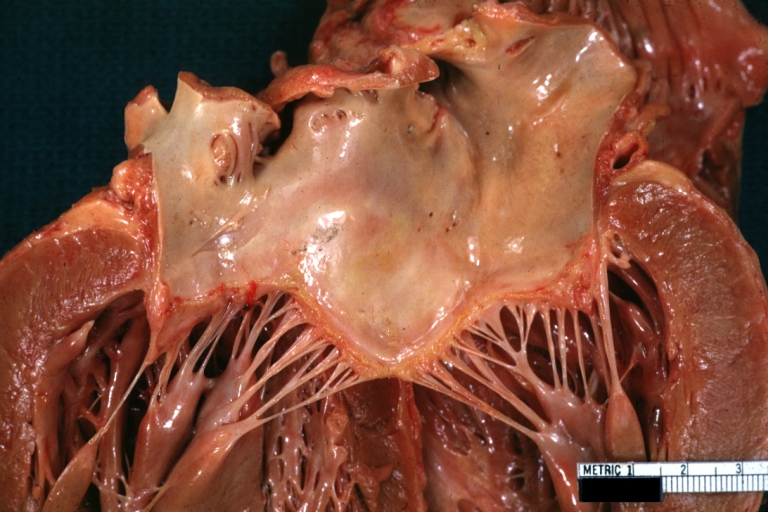
Rheumatic mitral valvulitis: Gross, an excellent example of fibrosis, chorda thickening and shortening has thrombus around the large left atrium
-
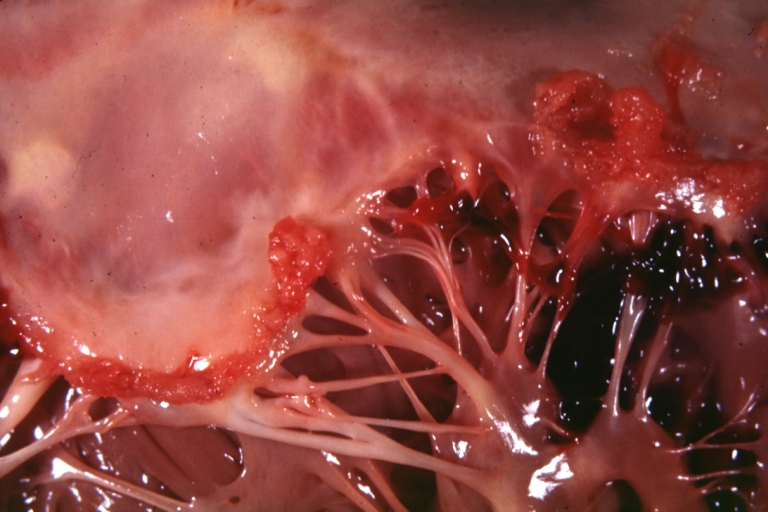
Mitral valve: acute rheumatic fever
-
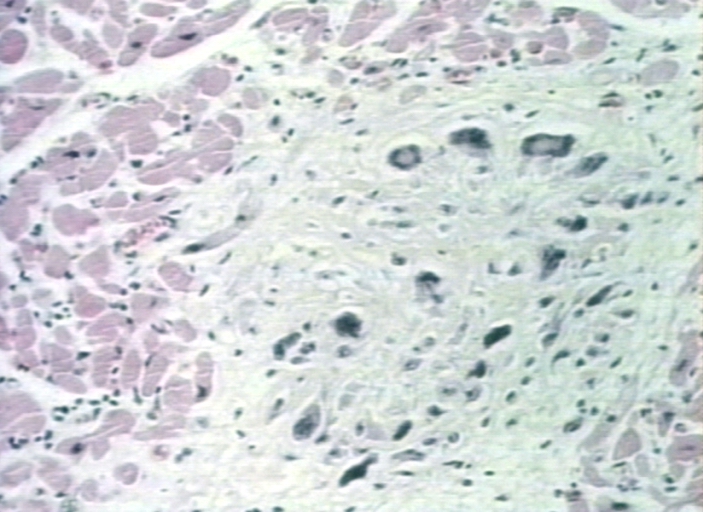
Aschoff bodies in rheumatic heart disease
-
Rheumatic Mitral Valvulitis: Gross; an excellent example of acute rheumatic fever lesion along line of closure of mitral valve