Lindane: Difference between revisions
No edit summary |
No edit summary |
||
| Line 22: | Line 22: | ||
'''Proper Use'''<br> | '''Proper Use'''<br> | ||
Instruct patients on the proper use of Lindane Lotion, the amount to apply, how long to leave it on, and avoiding retreatment. Inform patients that itching occurs after the successful killing of scabies and is not necessarily an indication for retreatment with Lindane Lotion. | Instruct patients on the proper use of Lindane Lotion, the amount to apply, how long to leave it on, and avoiding retreatment. Inform patients that itching occurs after the successful killing of scabies and is not necessarily an indication for retreatment with Lindane Lotion. | ||
|fdaLIADAdult=Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat. | |fdaLIADAdult=Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat. | ||
Patients should be provided specific information on use of product. | Patients should be provided specific information on use of product. Patients should be instructed on proper use of Lindane Lotion, especially the amount to apply, how long to leave on and the need to avoid retreatment. Patients should be informed that itching occurs after the successful killing of scabies (mites) and continued itching is not necessarily an indication for retreatment with Lindane Lotion. | ||
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient. | A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Lindane in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Lindane in adult patients. | ||
|offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Lindane in adult patients. | |offLabelAdultNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Lindane in adult patients. | ||
|fdaLIADPed=Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat. | |fdaLIADPed=Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat. | ||
Patients should be provided specific information on use of product. | |||
Patients should be instructed on proper use of Lindane Lotion, especially the amount to apply, how long to leave on and the need to avoid retreatment. Patients should be informed that itching occurs after the successful killing of scabies (mites) and continued itching is not necessarily an indication for retreatment with Lindane Lotion. | |||
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient. | A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient. | ||
| Line 48: | Line 49: | ||
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. | A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. | ||
|clinicalTrials=Lindane Lotion has been reported to cause central nervous system stimulation ranging from dizziness to seizures. Although seizures were almost always associated with ingestion or misuse of the product (to include repeat treatment), seizures and deaths have been reported when Lindane Lotion was used according to directions. Irritant dermatitis from contact with this product has also been reported | |clinicalTrials=Lindane Lotion has been reported to cause [[central nervous system stimulation]] ranging from [[dizziness]] to [[seizures]]. Although [[seizures]] were almost always associated with ingestion or misuse of the product (to include repeat treatment), [[seizures]] and deaths have been reported when Lindane Lotion was used according to directions. Irritant [[dermatitis]] from contact with this product has also been reported | ||
|postmarketing=The following adverse reactions reflect additional postmarketing experience of Lindane Lotion. These events include alopecia, dermatitis, headache, pain, paresthesia, pruritus and urticaria. The relationship of some of these events to Lindane therapy is unknown. | |postmarketing=The following adverse reactions reflect additional postmarketing experience of Lindane Lotion. These events include [[alopecia]], [[dermatitis]], [[headache]], [[pain]], [[paresthesia]], [[pruritus]] and [[urticaria]]. The relationship of some of these events to Lindane therapy is unknown. | ||
|drugInteractions=Oils may enhance absorption of Lindane, therefore, patients or caregivers applying Lindane Lotion should be warned about simultaneous use of creams, ointments, or oils. In addition, there are many drugs that may lower the seizure threshold, and Lindane Lotion should be prescribed with caution in patients taking these medications. Drugs that may lower the seizure threshold include, but are not limited to the following: | |drugInteractions=Oils may enhance absorption of Lindane, therefore, patients or caregivers applying Lindane Lotion should be warned about simultaneous use of creams, ointments, or oils. In addition, there are many drugs that may lower the seizure threshold, and Lindane Lotion should be prescribed with caution in patients taking these medications. Drugs that may lower the seizure threshold include, but are not limited to the following: | ||
*[[Antipsychotics]] | *[[Antipsychotics]] | ||
| Line 67: | Line 68: | ||
|useInPregnancyFDA=All pregnancies have a risk of birth defect, loss, or other adverse event regardless of drug exposure. Predictions of fetal risk from drug exposure rely heavily on animal data. However, animal studies may fail to predict effects in humans or may overstate such risks. Even if human data are available, the data may not be sufficient to determine whether there is an increased risk to the fetus, and individual reports of adverse outcomes in pregnancy in association with a drug may not reflect a causal relationship. | |useInPregnancyFDA=All pregnancies have a risk of birth defect, loss, or other adverse event regardless of drug exposure. Predictions of fetal risk from drug exposure rely heavily on animal data. However, animal studies may fail to predict effects in humans or may overstate such risks. Even if human data are available, the data may not be sufficient to determine whether there is an increased risk to the fetus, and individual reports of adverse outcomes in pregnancy in association with a drug may not reflect a causal relationship. | ||
Lindane Lotion should be given to pregnant women only if clearly needed. There are no adequate and well-controlled studies of Lindane Lotion in pregnant women. There are no known maternal or fetal health risks if the scabies is not treated. Lindane is lipophilic and may accumulate in the placenta. There has been a single case report of a stillborn infant following multiple maternal exposures to lindane during pregnancy. The relationship of the maternal exposures to the fetal outcome is unknown. | Lindane Lotion should be given to pregnant women only if clearly needed. There are no adequate and well-controlled studies of Lindane Lotion in pregnant women. There are no known maternal or fetal health risks if the [[scabies]] is not treated. Lindane is lipophilic and may accumulate in the placenta. There has been a single case report of a stillborn infant following multiple maternal exposures to lindane during pregnancy. The relationship of the maternal exposures to the fetal outcome is unknown. | ||
Animal data suggest that lindane exposure of the fetus may increase the likelihood of neurologic developmental abnormalities | Animal data suggest that lindane exposure of the fetus may increase the likelihood of neurologic developmental abnormalities, based on findings at systemic exposures close to that expected in humans when Lindane Lotion is used to treat scabies. The immature central nervous system (as in the fetus) may have increased susceptibility to the effects of the drug. | ||
|useInNursing=Lindane is lipophilic and is present in human breast milk, but exact quantities are not known. There may be a risk of toxicity if lindane is ingested from breast milk, or from skin absorption from mother to baby in the course of breast-feeding when Lindane Lotion is applied topically to the chest area. Nursing mothers who require treatment with Lindane Lotion should be advised of the potential risks and be counseled to avoid large areas of skin-to-skin contact with the infant while Lindane Lotion is applied, as well as to interrupt breast-feeding, with expression and discarding of milk, for at least 24 hours following use. | |useInNursing=Lindane is lipophilic and is present in human breast milk, but exact quantities are not known. There may be a risk of toxicity if lindane is ingested from breast milk, or from skin absorption from mother to baby in the course of breast-feeding when Lindane Lotion is applied topically to the chest area. Nursing mothers who require treatment with Lindane Lotion should be advised of the potential risks and be counseled to avoid large areas of skin-to-skin contact with the infant while Lindane Lotion is applied, as well as to interrupt breast-feeding, with expression and discarding of milk, for at least 24 hours following use. | ||
|useInPed=Animal data demonstrated increased risk of adverse events in the young across species. Pediatric patients have a higher surface to volume ratio and may be at risk of greater systemic exposure when Lindane Lotion is applied to the body. Infants and children may be at an even higher risk due to immaturity of organ systems such as skin and liver. Lindane Lotion should be used with extreme caution in patients who weigh less than approximately 110 lbs (50 kg) and especially in infants. Lindane Lotion is indicated only for the treatment of scabies; patients with lice should use Lindane Shampoo according to the labeled instructions. | |useInPed=Animal data demonstrated increased risk of adverse events in the young across species. Pediatric patients have a higher surface to volume ratio and may be at risk of greater systemic exposure when Lindane Lotion is applied to the body. Infants and children may be at an even higher risk due to immaturity of organ systems such as skin and liver. Lindane Lotion should be used with extreme caution in patients who weigh less than approximately 110 lbs (50 kg) and especially in infants. Lindane Lotion is indicated only for the treatment of scabies; patients with lice should use Lindane Shampoo according to the labeled instructions. | ||
| Line 136: | Line 137: | ||
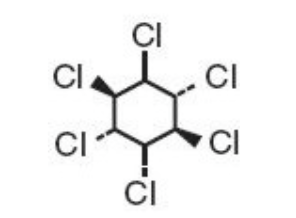
|structure=Lindane is the gamma isomer of 1,2,3,4,5,6-hexachlorocyclohexane having the following structural formula: | |structure=Lindane is the gamma isomer of 1,2,3,4,5,6-hexachlorocyclohexane having the following structural formula: | ||
[[file:Lindane Structure.png|none|400px]] | [[file:Lindane Structure.png|none|400px]] | ||
|PK=Lindane Lotion, USP 1%, is an ectoparasiticide and ovicide effective against Sarcoptes scabiei (scabies). Lindane exerts its parasiticidal action by being directly absorbed into the parasites and their ova. Feldmann and Maibach1 reported approximately 10% systemic absorption of a lindane acetone solution when applied to the forearm of human subjects and left in place for 24 hours. This vehicle was different from the approved product and the percutaneous penetration of lindane is dependent on the vehicle. Therefore, the clinical significance of these observations is unknown. Dale, et al2 reported a blood level of 290 ng/mL associated with convulsions following the accidental ingestion of a lindane-containing product. Ginsburg 3 found the greatest peak blood level of 64 ng/mL, 6 hours after total body application of Lindane Lotion in 1 of 8 non-scabietic pediatric patients. The half-life in blood was determined to be approximately 18 hours. | |PK=Lindane Lotion, USP 1%, is an ectoparasiticide and ovicide effective against Sarcoptes scabiei (scabies). Lindane exerts its parasiticidal action by being directly absorbed into the parasites and their ova. Feldmann and Maibach1 reported approximately 10% systemic absorption of a lindane acetone solution when applied to the forearm of human subjects and left in place for 24 hours. This vehicle was different from the approved product and the percutaneous penetration of lindane is dependent on the vehicle. Therefore, the clinical significance of these observations is unknown. Dale, et al2 reported a blood level of 290 ng/mL associated with convulsions following the accidental ingestion of a lindane-containing product. Ginsburg 3 found the greatest peak blood level of 64 ng/mL, 6 hours after total body application of Lindane Lotion in 1 of 8 non-scabietic pediatric patients. The half-life in blood was determined to be approximately 18 hours. | ||
Revision as of 21:55, 19 January 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alberto Plate [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNINGS
See full prescribing information for complete Boxed Warning.
Condition Name:
Lindane Lotion should only be used in patients who cannot tolerate or have failed first-line treatment with safer medications for the treatment of scabies. Neurologic Toxicity Contraindications Proper Use |
Overview
Lindane is an ectoparasiticide and ovicide. that is FDA approved for the treatment of Scabies (infestations of Sarcoptes scabei ) only in patients who:
- cannot tolerate other approved therapies
- have failed treatment with other approved therapies.. There is a Black Box Warning for this drug as shown here. Common adverse reactions include pruritus, post-treatment, dizziness, insomnia, anxiety.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat.
Patients should be provided specific information on use of product. Patients should be instructed on proper use of Lindane Lotion, especially the amount to apply, how long to leave on and the need to avoid retreatment. Patients should be informed that itching occurs after the successful killing of scabies (mites) and continued itching is not necessarily an indication for retreatment with Lindane Lotion.
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lindane in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lindane in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Apply a thin layer of Lindane Lotion over all skin from the neck down. One ounce is sufficient for an average adult. Do not prescribe more than 2 ounces for larger adults. Apply only once. Wash off in 8 to 12 hours. Do not retreat. Patients should be provided specific information on use of product.
Patients should be instructed on proper use of Lindane Lotion, especially the amount to apply, how long to leave on and the need to avoid retreatment. Patients should be informed that itching occurs after the successful killing of scabies (mites) and continued itching is not necessarily an indication for retreatment with Lindane Lotion.
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law. The Lindane Lotion Medication Guide is an important part of the risk management program for the patient.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lindane in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lindane in pediatric patients.
Contraindications
Lindane Lotion is contraindicated for premature infants because their skin may be more permeable than that of full term infants and their liver enzymes may not be sufficiently developed to metabolize Lindane. Lindane Lotion is also contraindicated for patients with crusted (Norwegian) scabies and other skin conditions (e.g., atopic dermatitis, psoriasis) that may increase systemic absorption of the drug. Lindane Lotion is contraindicated for patients with known uncontrolled seizure disorders and for individuals with a known sensitivity to the product or any of its components.
Warnings
|
WARNINGS
See full prescribing information for complete Boxed Warning.
Condition Name:
Lindane Lotion should only be used in patients who cannot tolerate or have failed first-line treatment with safer medications for the treatment of scabies. Neurologic Toxicity Contraindications Proper Use |
Seizures and deaths have been reported following Lindane Lotion's use with repeat or prolonged application, but also in rare cases following a single application reportedly used according to directions. It is not known how soon after application of a single dose of Lindane Lotion that a second dose of Lindane Lotion can be safely applied.
There have been cases of adverse events reported for Lindane Lotion and Lindane Shampoo in which a serious outcome (hospitalization, disability or death) has occurred.4 In approximately 20% of the total reported cases, Lindane Lotion and Shampoo were reported to have been used according to the labeled directions. Of these cases, thirteen deaths were reported, many cases which were remote from the time of actual Lindane use. Lindane toxicity, verified by autopsy was the cause of one infant's death, was the cause of death reported for an adult who ingested it orally in a successful suicide. The direct causes of death for the other cases were attributed to reasons other than Lindane. Most of these adverse events occurred with Lindane Lotion.
Infants, children, the elderly, and individuals with other skin conditions and those who weigh < 110 lbs (50 kg) may be at greater risk of serious neurotoxicity. Animal studies have shown increased susceptibility to neurologic adverse events in younger animals. Children have a larger body surface area to volume ratio that may result in a proportionately larger systemic exposure.
Careful consideration should be given before prescribing Lindane Lotion to patients with conditions that may increase the risk of seizure, such as HIV infection, history of head trauma or a prior seizure, CNS tumor, the presence of severe hepatic cirrhosis, excessive use of alcohol, abrupt withdrawal from alcohol or sedatives, as well as concomitant use of medications known to lower seizure threshold.
Patients should be instructed on proper use of Lindane Lotion, especially the amount to apply, how long to leave the lotion on, and the need to avoid retreatment. Patients should be informed that itching may occur, and even worsen, after the successful killing of scabies. Repeat treatment is usually not necessary.
A Lindane Lotion Medication Guide must be given to the patient each time Lindane Lotion is dispensed, as required by law.
Adverse Reactions
Clinical Trials Experience
Lindane Lotion has been reported to cause central nervous system stimulation ranging from dizziness to seizures. Although seizures were almost always associated with ingestion or misuse of the product (to include repeat treatment), seizures and deaths have been reported when Lindane Lotion was used according to directions. Irritant dermatitis from contact with this product has also been reported
Postmarketing Experience
The following adverse reactions reflect additional postmarketing experience of Lindane Lotion. These events include alopecia, dermatitis, headache, pain, paresthesia, pruritus and urticaria. The relationship of some of these events to Lindane therapy is unknown.
Drug Interactions
Oils may enhance absorption of Lindane, therefore, patients or caregivers applying Lindane Lotion should be warned about simultaneous use of creams, ointments, or oils. In addition, there are many drugs that may lower the seizure threshold, and Lindane Lotion should be prescribed with caution in patients taking these medications. Drugs that may lower the seizure threshold include, but are not limited to the following:
- Antipsychotics
- Antidepressants
- Theophylline
- Cyclosporine
- Mycophenolate mofetil
- Tacrolimus capsules
- Penicillins, imipenem, quinolone antibiotics
- Chloroquine sulfate, pyrimethamine
- Isoniazid
- Meperidine
- Radiographic contrast agents
- Centrally active anticholinesterases
- Methocarbamol
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C All pregnancies have a risk of birth defect, loss, or other adverse event regardless of drug exposure. Predictions of fetal risk from drug exposure rely heavily on animal data. However, animal studies may fail to predict effects in humans or may overstate such risks. Even if human data are available, the data may not be sufficient to determine whether there is an increased risk to the fetus, and individual reports of adverse outcomes in pregnancy in association with a drug may not reflect a causal relationship.
Lindane Lotion should be given to pregnant women only if clearly needed. There are no adequate and well-controlled studies of Lindane Lotion in pregnant women. There are no known maternal or fetal health risks if the scabies is not treated. Lindane is lipophilic and may accumulate in the placenta. There has been a single case report of a stillborn infant following multiple maternal exposures to lindane during pregnancy. The relationship of the maternal exposures to the fetal outcome is unknown.
Animal data suggest that lindane exposure of the fetus may increase the likelihood of neurologic developmental abnormalities, based on findings at systemic exposures close to that expected in humans when Lindane Lotion is used to treat scabies. The immature central nervous system (as in the fetus) may have increased susceptibility to the effects of the drug.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lindane in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Lindane during labor and delivery.
Nursing Mothers
Lindane is lipophilic and is present in human breast milk, but exact quantities are not known. There may be a risk of toxicity if lindane is ingested from breast milk, or from skin absorption from mother to baby in the course of breast-feeding when Lindane Lotion is applied topically to the chest area. Nursing mothers who require treatment with Lindane Lotion should be advised of the potential risks and be counseled to avoid large areas of skin-to-skin contact with the infant while Lindane Lotion is applied, as well as to interrupt breast-feeding, with expression and discarding of milk, for at least 24 hours following use.
Pediatric Use
Animal data demonstrated increased risk of adverse events in the young across species. Pediatric patients have a higher surface to volume ratio and may be at risk of greater systemic exposure when Lindane Lotion is applied to the body. Infants and children may be at an even higher risk due to immaturity of organ systems such as skin and liver. Lindane Lotion should be used with extreme caution in patients who weigh less than approximately 110 lbs (50 kg) and especially in infants. Lindane Lotion is indicated only for the treatment of scabies; patients with lice should use Lindane Shampoo according to the labeled instructions.
Geriatic Use
There have been no studies of Lindane Lotion in the elderly. There are four postmarketing reports of deaths in elderly patients who were treated for scabies with Lindane Lotion. Two patients died within 24 hours of Lindane Lotion application, and the third patient died 41 days after application of Lindane Lotion, having suffered a seizure on the day of death. A fourth patient died of an unreported cause of death on the same day that Lindane Lotion treatment for scabies was administered.
Gender
There is no FDA guidance on the use of Lindane with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lindane with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Lindane in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Lindane in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Lindane in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Lindane in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Lindane Administration in the drug label.
Monitoring
There is limited information regarding Lindane Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Lindane and IV administrations.
Overdosage
Contact the closest Poison Control Center in the event of suspected overdosage with Lindane Lotion.
If accidental ingestion occurs, prompt gastric lavage should be instituted. However, since oils enhance absorption, saline cathartics for intestinal evacuation should be given rather than oil laxatives. If central nervous system (CNS) manifestations occur, they may be antagonized by the administration of pentobarbital, phenobarbital, or diazepam.
Pharmacology
Mechanism of Action
There is limited information regarding Lindane Mechanism of Action in the drug label.
Structure
Lindane is the gamma isomer of 1,2,3,4,5,6-hexachlorocyclohexane having the following structural formula:
Pharmacodynamics
There is limited information regarding Lindane Pharmacodynamics in the drug label.
Pharmacokinetics
Lindane Lotion, USP 1%, is an ectoparasiticide and ovicide effective against Sarcoptes scabiei (scabies). Lindane exerts its parasiticidal action by being directly absorbed into the parasites and their ova. Feldmann and Maibach1 reported approximately 10% systemic absorption of a lindane acetone solution when applied to the forearm of human subjects and left in place for 24 hours. This vehicle was different from the approved product and the percutaneous penetration of lindane is dependent on the vehicle. Therefore, the clinical significance of these observations is unknown. Dale, et al2 reported a blood level of 290 ng/mL associated with convulsions following the accidental ingestion of a lindane-containing product. Ginsburg 3 found the greatest peak blood level of 64 ng/mL, 6 hours after total body application of Lindane Lotion in 1 of 8 non-scabietic pediatric patients. The half-life in blood was determined to be approximately 18 hours.
Data available in the literature suggest that lindane has a rapid distribution phase followed by a longer β-elimination phase.1, 2, 3
Nonclinical Toxicology
There is limited information regarding Lindane Nonclinical Toxicology in the drug label.
Clinical Studies
There is limited information regarding Lindane Clinical Studies in the drug label.
How Supplied
Lindane Lotion, USP 1% is supplied in patient-size 2 fl oz (60 mL) bottles.
Storage
Store at 20° to 25°C (68° to 77°F)
Images
Drug Images
{{#ask: Page Name::Lindane |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
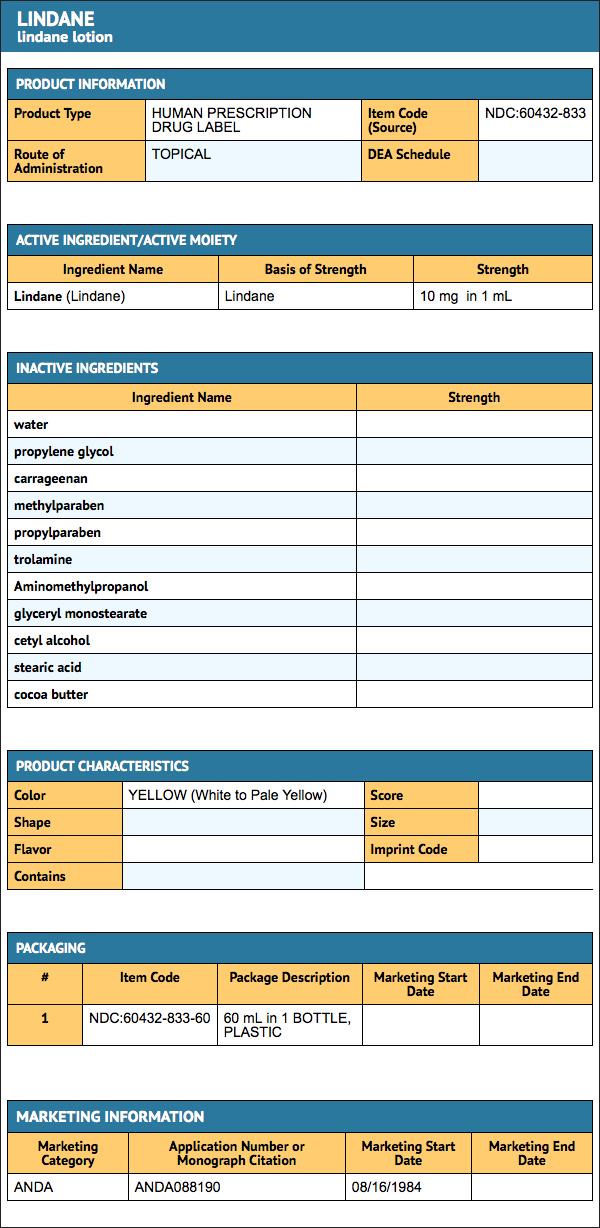
{{#ask: Label Page::Lindane |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Lindane Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Lindane interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Lindane Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Lindane Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Report of the Conference of the Parties of the Stockholm Convention on Persistent Organic Pollutants on the work of its fourth meeting. Convention on Persistent Organic Pollutants. Fourth meeting, Geneva, 4–8 May 2009. http://chm.pops.int/Portals/0/Repository/COP4/UNEP-POPS-COP.4-38.English.pdf
{{#subobject:
|Label Page=Lindane |Label Name=Lindane box.png
}}
| File:Lindane.svg | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | Topical |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 91% |
| Metabolism | Hepatic cytochrome P-450 oxygenase system |
| Elimination half-life | 18 hours |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C6H6Cl6 |
| Molar mass | 290.828 g/mol |
Lindane is a synthetic chemical that was initially developed as an agricultural insecticide and then formulated for medical use due to its antiparasitic efficacy against scabies and lice.
Lindane is the gamma isomer of hexachlorocyclohexane (“gamma-HCH”), formerly known as benzene hexachloride or BHC, and more broadly belongs to the organochlorine class of compounds. Its mechanism of action is by interfering with the GABA neurotransmitter function of parasites, specifically by interacting with the GABAA receptor-chloride channel complex at the picrotoxin binding site.[1] In animal models, lindane has a reported oral LD50 of 88 mg/kg and a dermal LD50 of 1000 mg/kg.[1] In humans, health effects have been described for oral, respiratory and dermal routes of lindane exposure, with varied clinical outcomes depending on the situation, setting and use application.[1]
Agricultural vs. Healthcare Applications
Lindane (i.e., gamma-HCH) has been available for use in the U.S. for more than 60 years, with applications in both healthcare and agriculture. In the 1940s, lindane was registered with the U.S. Department of Agriculture (USDA), and in 1951 it was approved by the U.S. Food and Drug Administration (FDA) for medical use in the treatment of scabies, head lice and pubic lice (crabs). During this time, the vast majority of lindane use―more than 99%―has been for agricultural purposes and much of the safety and environmental concerns have related to this application. [2][3] This is not unlike other medications where the active ingredient has other non-healthcare applications. For example, warfarin is used as a rodenticide to poison mice and rats (e.g., Kaput™, D-Con™) but is also formulated for medical use as an oral anticoagulant or "blood thinner" to treat patients with heart attacks, strokes and other clot-related disorders (e.g., Coumadin®).
In 2006, the U.S. Environmental Protection Agency (EPA) called for the voluntary cancellation of all agricultural uses of lindane, limited in recent years to pre-planting seed treatments.[4] (see also Regulatory Status) The FDA, however, continues to support the use of lindane prescription medications, noting that “The risk of occupational/environmental exposure should be assessed separately and independent of the risk related to the therapeutic use of a medication to treat a medical condition where there is direct benefit to the patient.” [5] (see also Regulatory History) Repeatedly, the FDA has concluded that lindane medications provide public health benefits at an acceptably low level of risk—a factor for all medications.[5]
In 1995, lindane medications were designated second-line and are now reserved for patients who are unable to tolerate or have failed first-line treatments—--a growing problem in the U.S. and elsewhere due to increased rates of resistance.[5][6][7] The U.S. Centers for Disease Control and Prevention also includes lindane medications in their Sexually Transmitted Disease Treatment Guidelines as viable treatment alternatives for the management of scabies and pubic lice, consistent with the approved prescription labeling for these products.[8] (see also Pharmaceutical Uses) Other countries, like Canada, similarly approve of pharmaceutical applications for lindane but no longer permit its broader use agriculturally. (see also Regulatory Status)
Pharmaceutical Uses
In the U.S., lindane medications are regulated and approved for clinical use in humans by the FDA. Lindane Lotion is approved for the treatment of scabies. Lindane Shampoo is approved for the treatment of pubic lice (crabs) and head lice.[9][10] Both medications contain 1% purified pharmaceutical-grade gamma-HCH and are formulated to the standards of the United States Pharmacopeia (USP)—the official public authority that sets quality standards for drugs manufactured and sold in the U.S.[11] They are available as prescription-only medications and are indicated second line, meaning they are prescribed when first-line therapies have failed, cannot be tolerated or are otherwise contraindicated.
Lindane lotion and lindane shampoo have been used clinically for more than 50 years in tens of millions of patients, if not more, and have been reviewed for safety on numerous occasions by experts working with the FDA who have consistently confirmed the safety and tolerability of these medicines when used properly. Although serious side effects have been reported (e.g. seizures), they are rare and have almost always resulted from improper use and oral ingestion.[3][5]
Adverse Reactions
The most common side effects associated with topical use of lindane medications are nonserious reactions of the skin, including burning, itching, dryness and rash.[12] Central nervous system stimulation ranging from dizziness to seizures, has also been reported; however, serious effects, like seizures, have almost always resulted from oral ingestion or misuse of medication (e.g., repeated treatments or prolonged applications). [13] Only rarely have seizures and even more rarely fatal reactions been reported when lindane medications were used (presumably) according to directions. [5] [9] [10]
In 2003, the FDA published a safety analysis of adverse events reported in association with the use of lindane medications received through its adverse event monitoring system (“AERS” database) between from 1974 through 2002. [13] The vast majority (85%) of these reports―488 total―were classified as nonserious, while serious events most often resulted from product misuse (80% of serious cases). The most common reports to the FDA were "drug ineffective," followed by convulsions, dermatitis and dizziness. (Note: These events represent the most common reported to the FDA and do not represent the most common events associated with the use of lindane lotion and lindane shampoo overall).
A review of the most serious cases described 15 deaths of which two were confirmed related to lindane misuse including a suicidal ingestion. The direct causes of death for the other cases were attributed to reasons other than lindane. In addition, there were 46 hospitalizations, and seven life-threatening outcomes—five from the same household. Six cases of congenital anomaly were also described–five for infants "possibly" exposed to lindane in utero and one paternal exposure—but no characteristic pattern of effect was noted.[5] [13]
In all age groups, reported adverse events occurred mainly in patients with contraindications to the use of lindane or in those who appeared to have misapplied or orally ingested medication [5]
Based on these findings, lindane lotion and lindane shampoo were limited to small unit-dose bottles in 2003 by the FDA to mitigate the risk of misuse and further enhance product safety. At the same time, a boxed warning was added to the prescription label to highlight to healthcare providers appropriate use criteria and rare treatment risks. A medication guide, written in plain English, was also developed and is now required by law to be dispensed with every lindane prescription dispensed in the U.S. to better educate patients and caregivers on safe application technique.[5][14] When used properly, lindane medications are safe and effective for the diseases they are approved. The most common side effects are nonserious reactions of the skin (e.g., burning, itching, dryness and rash).[12]
The current FDA-approved product labeling emphasizes that lindane medications are contraindicated for use in premature infants and individuals with known uncontrolled seizure disorders and should be used with caution in infants, children, the elderly, and individuals with other skin conditions (e.g., atopic dermatitis, psoriasis) and in those who weigh less than 110 lbs (50 kg) as they may be at risk of serious neurotoxicity. It also notes that careful consideration should be given before prescribing lindane medications to patients with conditions that may increase the risk of seizure, such as HIV infection, history of head trauma or a prior seizure, CNS tumor, the presence of severe hepatic cirrhosis, excessive use of alcohol, abrupt withdrawal from alcohol or sedatives, as well as concomitant use of medications known to lower seizure threshold.[9][10] Additional information on the benefits and risks of pharmaceutical lindane, including full prescribing information and patient medication guides for lindane lotion and lindane shampoo, can be found on the FDA’s website at: http://www.fda.gov/cder/drug/infopage/lindane/default.htm.
In the U.S., lindane medications are exclusively manufactured and distributed by Morton Grove Pharmaceuticals, Inc. The company’s promotion agreement with Alliant Pharmaceuticals, which commenced in 2005, was terminated May 2007.[15]
Human Health Effects
While adverse reactions can occur with use of low-dose topical pharmaceutical formulations, serious effects are rare and have most often resulted from the misuse of medication.[5][9][10] [13] (see also Pharmaceutical Uses) Indeed, most of the adverse human health effects reported for lindane have related to agricultural uses and chronic, occupational exposure of seed treatment workers to agricultural-grade lindane.[16] (see also Agricultural vs. Healthcare Applications)
Exposure to large amounts of lindane can negatively affect the nervous system, producing a range of symptoms from headache and dizziness to seizures, convulsions and more rarely death.[1] Adverse hematologic effects have also been reported with chronic occupational exposures and excessive dermal applications; however, a direct cause and effect has not been established.[1] Vomiting and nausea are usual symptoms associated with oral ingestions of lindane but serious neurologic effects can occur, albeit less frequently.[1][17] The most common side effects with topical use of lindane medications are nonserious reactions of the skin, including burning, itching, dryness and rash.
[12] (see also Pharmaceutical Uses) Lindane has not been shown to alter immunocompetence in humans and is not considered to be genotoxic.[1]
Studies of the carcinogenic effects of lindane have been inconclusive and often limited by study design; however, no major carcinogenic effects have been noted in human trials to date.[1]
For example, a meta-analysis of studies looking at the association between occupational exposure to agricultural lindane and non-Hodgkin’s lymphona among U.S. farmers found that lindane was not a primary factor in the development of the disease.[18] The majority of studies of the general population have also shown no association between serum or breast tissue levels of lindane and breast cancer.[1][19] Similarly, no increased cancer risk was noted in a large epidemiologic study of lindane medications involving a 143,594-patient database with up to 21 years of follow up, which concluded that “There is still no persuasive evidence from studies of humans that lindane, as ordinarily used clinically, is carcinogenic in humans.” [20]
In 1987, the International Agency for Research on Cancer (IARC) classified lindane as a possible human carcinogen.[21] However, more recent evaluations by subject matter experts do not support this rating. In 2001, the Environmental Protection Agency’s Cancer Assessment Review Committee for lindane downgraded the carcinogenic classification of lindane from “possible” to “suggestive evidence,” concluding that the data did not support the need for further study of the carcinogenic risks in humans.[22] The Joint Committee on Pesticide Residues (JMPR) of The World Health Organization and Food and Agricultural Organization of the United Nations similarly concluded in 2004 that “In the absence of genotoxicity and on the basis of the weight of the evidence from the studies of carcinogenicity, JMPR has concluded that lindane is not likely to pose a carcinogenic risk to humans.”[19]
Environmental Contamination
The issue of environmental contamination has largely revolved around extensive agricultural uses of lindane and chemical manufacturing, which have declined significantly in the last 20 years.[23] Indeed, trend analyses show a significant reduction in lindane levels in the U.S. from 1986 through 2003, consistent with decreasing agricultural usage patterns.[24]
In the U.S., more than 99% of lindane has been in the form of agricultural-grade products; less than 1% has been used for medicinal purposes.[2] (see also Agricultural vs. Healthcare Applications) Lindane is released into the environment during and after agricultural application through volatilization into the atmosphere (estimated at 12-30%), where it has long-range transport potential and can be deposited by rainfall.[4] Lindane in soil can leach to surface and even ground water, although the potential is low, and can bioaccumulate in the food chain.[4] In fact, the most widespread exposure of the general population to lindane results from agricultural uses and the intake of contaminated foods, such as produce, meats and milk.[1] Over time, lindane is broken down in soil, sediment and water into less harmful substances by algae, fungi and bacteria; however, the process is relatively slow and dependent on ambient environmental conditions.[1] The ecological impact of lindane’s environmental persistence continues to be debated.
Lindane has not been shown to be a drinking water contaminant of concern in the U.S.[1] In 2003, the EPA reported on the results of large-scale water contaminant testing of 16,000 water systems serving 100 million people across the U.S. and found that none contained lindane levels above the maximum contaminant level standard considered safe.[25] Similar findings were noted by U.S. Geologic Survey teams in 1999 and 2000.[26] More specifically, the EPA conducted “down-the-drain” estimates of the amount of lindane reaching public water supplies from the use of lindane medications using data from California water treatment facilities, concluding that lindane levels from pharmaceutical sources were “extremely low” and not of concern.[3] Again, lindane medications have accounted for only a small fraction of the total amount of lindane used in the U.S.[2]
The current water safety standard, or maximum contaminant level (“MCL”) for the amount of lindane allowed in public drinking water reservoirs—established by the EPA in 1991—is 0.2 parts per billion (“ppb”).25 In 2003, the Agency found scientific justification to raise the MCL for lindane to 1.0 ppb based on new data of the health effects of lindane; however, this change was never implemented because states had no apparently difficulty in maintaining levels below the MCL standard previously set as noted above.[25]
Non-Gamma Isomers
Larger than the issue of lindane toxicity are concerns related to the non-gamma isomers of HCH, namely alpha-HCH and beta-HCH, which are notably more toxic than lindane.[1] Alpha- and beta-HCH were used agriculturally in the U.S. in the form of technical-grade HCH until 1976 and are also produced as manufacturing by-products but are void of insecticidal properties and have little to no use.[1] In the 1940s and 1950s lindane producers stockpiled these isomers in open heaps, which led to ground and water contamination. The International HCH and Pesticide Forum has since been established to bring together experts to address the clean-up and containment of these sites.[27] Modern manufacturing standards for lindane involve the treatment and conversion of waste isomers to less toxic industrial chemicals, a process known as “cracking.”[24][27] Today, only a few production plants remain active worldwide to accommodate public health uses of lindane and declining agricultural needs.[2] Lindane has not been manufactured in the U.S. since the mid-1970s but continues to be imported and formulated for restricted use.
Regulatory Status
Lindane is registered for use in 50 countries, with restricted-use status in 33 of these countries.[2][23] The latter includes the U.S. and Canada, which support public health uses of pharmaceutical lindane but no longer allow agricultural applications.[2][4] The US FDA continues to maintain that lindane medications have necessary health benefits that outweigh potential risks and should remain available for patients with head lice, scabies and pubic lice (crabs) who have few treatment alternatives.[5] These infectious diseases, two of which are sexually transmitted, affect tens of millions of Americans and hundreds of millions of people worldwide every year.[28][29] In the U.S., petitions to ban the use of pharmaceutical lindane have been rejected by the FDA and determined to be without merit by experts working with this regulatory agency.[5] Worldwide, effective treatment options for the control of scabies and lice are relatively limited.[16]
Canada’s Pest Management Regulatory Agency phased out of all agricultural uses of lindane between 2000 and 2005 due to concerns of chronic occupational exposure and risks to workers during seed treatment and planting. However, lindane medications remain available in Canada for public health purposes as non-prescription therapies.[23] In 2002, the EPA concluded that lindane agricultural products were eligible for re-registration given industry compliance with certain data and labeling requirements to mitigate occupational risks to workers.[3] However, in 2006, the Agency published an addendum to its initial decision and called for the voluntary cancellation of all agricultural uses by registered manufacturers (effective July 2007), citing a significant change in the costs and benefits of agricultural uses due to the recent introduction of seed-treatment alternatives to lindane. The EPA has approved the use of lindane stockpiles through 2009.[4] Lindane medications remain available for public health purposes in the U.S. but, unlike Canada, are prescription-only therapies.
Lindane is banned in 52 countries, including some European and developing countries, and is under review for addition to the Stockholm Convention On Persistent Organic Pollutants.[30][31] Mexico has committed to a structured, voluntary phase out of lindane through the North American Regional Action Plan (NARAP) but currently authorizes agricultural, veterinary and healthcare uses.[2]
California passed legislation banning pharmaceutical uses of lindane (effective 2002) and there is a bill in the New York State Assembly and Senate to ban its use in head lice products and limit its use on scabies, which had not passed as of September 2007. However, the FDA continues to support the use of lindane medications for the diseases they are indicated and approved.[5]
Morton Grove Lawsuit
In the face of negative publicity concerning lindane pharmaceutical products, the U.S. manufacturer, Morton Grove Pharmaceuticals, filed a legal complaint on February 6, 2007 in the U.S. District Court in Chicago, Illinois against the National Pediculosis Association, the Ecology Center, Inc., and two physicians for statements made and disseminated to healthcare providers and consumers using the internet and through a series of printed literature . As noted by the U.S. District Court, the case pleads that “[d]efendants swap agricultural and pharmaceutical research selectively quoting and/or misstating findings from studies relating to the agricultural use of lindane, and widely disseminate false, misleading, and defamatory statements about the safety profile and effectiveness of lindane.”[32] On June 18, 2007, Judge Elaine Bucklo issued a written decision denying defendant’s motion to dismiss and further held that Morton Grove had properly pled a case suitable for trial on the following counts: defamation, false advertising under the Federal Lanham Act, trade disparagement and violation of the Illinois Uniform Deceptive Trade Practice Act. The company seeks damages and injunctive relief against all of the defendants. [32]
In response to Morton Grove's complaint, the Ecology Center defendents moved to dismiss the case based on an alleged lack of personal jurisdiction. However, Morton Grove presented new facts supporting its case for jurisdiction in Illinois and the Court held that Morton Grove's "Second Amended Complaint would provide specific jurisdiction over the Center and Weil." (June 8, 2007 order)
See also
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services. Toxicologic profile for alpha-, beta, gamma- and delta-hexachlorocyclohenxane. August 2005. http://www.atsdr.cdc.gov/toxprofiles/tp43.pdf
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 Commission for Environmental Cooperation. North American Regional Action Plan (NARAP) on lindane and other hexachlorocyclohexane (HCH) isomers. November 30, 2006. http://www.cec.org/files/PDF/POLLUTANTS/LindaneNARAP-Nov06_en.pdf
- ↑ 3.0 3.1 3.2 3.3 U.S. Environmental Protection Agency (EPA). Lindane Reregistration Eligibility Decision (RED). 2002. http://www.epa.gov/espp/effects/lindane/attach-1.pdf
- ↑ 4.0 4.1 4.2 4.3 4.4 U.S. EPA. Addendum to the 2002 Lindane Reregistration Eligibility Decision (RED). July 2006. http://www.epa.gov/oppsrrd1/REDs/lindane_red_addendum.pdf
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 U.S. Food and Drug Administration (FDA). Lindane Assessment Memorandum. Posted 2003. http://www.fda.gov/cder/drug/infopage/lindane/lindanememoassessment.pdf.
- ↑ McCarthy JS, Kemp DJ, Walton SF, et al. Scabies: more than just an irritation. Postgrad. Med. J. 2004;80:382–387.
- ↑ Thomas DR, McCarroll L, Roberts R, et al. Surveillance of insecticide resistance in head lice using biochemical and molecular methods. Arch. Dis. Child. 2006; 91:777-778.
- ↑ U.S. Centers for Disease Control and Prevention (CDC). Ectoparasitic infections. Sexually transmitted diseases treatment guidelines. MMWR Recomm Rep. 2006, August 10;55 (No. RR-11):79-80. http://www.cdc.gov/std/treatment.
- ↑ 9.0 9.1 9.2 9.3 Lindane lotion, USP, 1% prescribing information. Updated March 28, 2003. http://www.fda.gov/cder/foi/label/2003/006309lotionlbl.pdf
- ↑ 10.0 10.1 10.2 10.3 Lindane shampoo, USP, 1% prescribing information. Updated March 28, 2003. http://www.fda.gov/cder/foi/label/2003/006309shampoolbl.pdf.
- ↑ U.S. Pharmacopeia. http://www.usp.org/aboutUSP/
- ↑ 12.0 12.1 12.2 U.S. FDA Centers for Drug Evaluation and Research. Lindane lotion and lindane shampoo questions and answers. Updated April 15, 2003. http://www.fda.gov/cder/drug/infopage/lindane/lindaneQA.htm
- ↑ 13.0 13.1 13.2 13.3 U.S. FDA. Lindane Post Marketing Safety Review. Posted 2003. http://www.fda.gov/cder/drug/infopage/lindane/lindaneaeredacted.pdf
- ↑ U.S. FDA. FDA talk paper on lindane. March 28, 2003. http://www.fda.gov/bbs/topics/ANSWERS/2003/ANS01205.html
- ↑ Sciele Pharma Completes Acquisition of Alliant Pharmaceuticals. Press Release; June 12, 2007. http://phx.corporate-ir.net/phoenix.zhtml?c=120763&p=irol-newsArticle&ID=1014610&highlight
- ↑ 16.0 16.1 Persistent Organic Pollutant Review Committee (POPRC). Draft risk management evaluation for lindane. May, 2007. http://www.pops.int/documents/meetings/poprc/drprofile/drme/DraftRME_Lindane.pdf
- ↑ U.S. CDC. Unintentional Topical Lindane Ingestions --- United States, 1998—2003. Morbidity and Mortality Weekly Report. 2005;54:533-535.
- ↑ Blair A, Cantor KP, Hoar Zahm S. Non-Hodgkin’s lymphoma and agricultural use of the insecticide lindane. Am. J. Ind. Med. 1998;33:82-87.
- ↑ 19.0 19.1 World Health Organization (WHO). Lindane in Drinking Water: Background Document for Development of WHO Guidelines for Drinking-Water Quality. 2004. http://www.who.int/water_sanitation_health/dwq/chemicals/lindane/en/print.html
- ↑ Friedman GD. Lindane and cancer in humans: A false alarm? Pharmacoepidemiol and Drug Saf. 1997;6:129-134.
- ↑ International Agency for Research on Cancer (IARC). Summaries & Evaluations: HEXACHLOROCYCLOHEXANES (Group 2B). Updated March 2, 1998. http://www.inchem.org/documents/iarc/suppl7/hexachlorocyclohexanes.html
- ↑ U.S. EPA. Evaluation of the Carcinogenic Potential of Lindane, PC. Code: 009001. 2001. http://www.lindane.com/pdf/EPA_Cancer_Assessment_of_Lindane2001.pdf
- ↑ 23.0 23.1 23.2 U.S. EPA. Assessment of lindane and other hexachlorocyclohexane isomers. February 8, 2006
- ↑ 24.0 24.1 United Nations Environment Programme. POPRC of the Stockholm Convention. Draft risk profile: Lindane. July 2006.
- ↑ 25.0 25.1 U.S. EPA. Announcement of completion of EPA’s review of existing drinking water standards. Federal Register. 68(138): July 18, 2003.
- ↑ Kolpin DW, Furlong ET, Meyer MT, et al. Pharmaceuticals, hormones, and other organic wastewater contaminants in U.S. streams, 1999–2000: A national reconnaissance. Environ Sci Technol. 2002;36(6):1202–1211.
- ↑ 27.0 27.1 International HCH & Pesticides Association. The legacy of lindane HCH isomer production. 2006. http://www.ihpa.info/docs/library/Lindane%20Main%20Report%20DEF20JAN06.pdf
- ↑ Guenther L, Maguiness S, Austin TW. Pediculosis. 2006. http://www.emedicine.com/med/topic1769.htm.
- ↑ Chosidow O. Scabies. N Engl J Med. 2006;354:1719-1727.
- ↑ Persistent Organic Pollutants Review Committee http://www.pops.int/documents/meetings/poprc/chemreview.htm
- ↑ Pesticide Action Network map of Lindane bans and restrictions http://www.panna.org/campaigns/docsLindane/lindaneBannedMap.pdf
- ↑ 32.0 32.1 Morton Grove Pharmaceuticals, Inc. v. The National Pediculosis Association, et al., No. 06 C 3815 (N.D. Ill. June 18, 2007) (Bucklo, J.)
- This article is based in part on the public domain US government document at FDA.gov.
External links
- Lindane Facts
- "Mom and Pros Tackle Lice"
- FDA Information on Lindane
- EPA Evaluation of Carcinogenic Potential of Lindane
- World Health Organization Background Document on Lindane for Drinking-Water Quality Guidelines
- Lindane Public Safety Considerations
- Scabies and Lice
- Medical and Scientific Opinions on Pharmaceutical Lindane
- Pepsi and Coca-Cola - Lindane in drinks in India
- India - Pesticides in Coke & Pepsi drinks
- Lindane Chemistry and Uses
- Time for the FDA to ban Lindane
- Gamma Hexachlorocyclohexane Fact Sheet
- Pages with script errors
- Pages with reference errors
- Pages with broken file links
- Drugs with non-standard legal status
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- Organochloride insecticides