Cavernous angioma pathophysiology: Difference between revisions
| Line 35: | Line 35: | ||
CCM can also be subdivided into two, according to its pattern of occurrence: <ref name="pmid28387823">{{cite journal| author=Akers A, Al-Shahi Salman R, A Awad I, Dahlem K, Flemming K, Hart B | display-authors=etal| title=Synopsis of Guidelines for the Clinical Management of Cerebral Cavernous Malformations: Consensus Recommendations Based on Systematic Literature Review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel. | journal=Neurosurgery | year= 2017 | volume= 80 | issue= 5 | pages= 665-680 | pmid=28387823 | doi=10.1093/neuros/nyx091 | pmc=5808153 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28387823 }} </ref> | CCM can also be subdivided into two, according to its pattern of occurrence: <ref name="pmid28387823">{{cite journal| author=Akers A, Al-Shahi Salman R, A Awad I, Dahlem K, Flemming K, Hart B | display-authors=etal| title=Synopsis of Guidelines for the Clinical Management of Cerebral Cavernous Malformations: Consensus Recommendations Based on Systematic Literature Review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel. | journal=Neurosurgery | year= 2017 | volume= 80 | issue= 5 | pages= 665-680 | pmid=28387823 | doi=10.1093/neuros/nyx091 | pmc=5808153 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28387823 }} </ref> | ||
*[[Familial]] or [[Hereditary]][[CCM]] | *[[Familial]] or [[Hereditary]] [[CCM]] | ||
**Constitutes 20% of all [[cavernous angioma]] cases | **Constitutes 20% of all [[cavernous angioma]] cases | ||
**Occurs as multiple lesions | **Occurs as multiple lesions | ||
Revision as of 12:17, 11 March 2022
| Cavernous angioma pathophysiology | |
 | |
|---|---|
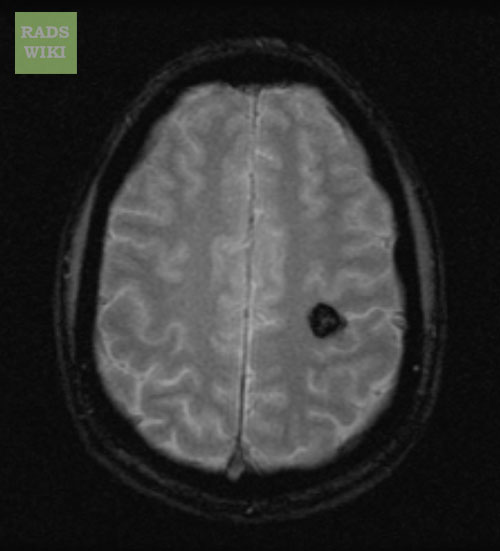
| MRI: Cavernous malformation. (Image courtesy of RadsWiki) |
|
Cavernous angioma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cavernous angioma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Cavernous angioma pathophysiology |
|
Risk calculators and risk factors for Cavernous angioma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Edzel Lorraine Co, D.M.D, M.D.
Overview
Developmental venous anomaly (DVA) can cause a chronic increase in intracranial pressure which can form microhemorrhages around DVA, leading to the development and growth of cavernous angioma. There are two patterns of cavernous angioma, the sporadic and the familial pattern.
Pathophysiology
In up to 30% there is a coincidence of cerebral cavernous malformation (CCM0 with a venous angioma, also known as a developmental venous anomaly (DVA). These lesions appear either as enhancing linear blood vessels or caput medusae, a radial orientation of small vessels that resemble the hair of Medusa from Greek mythology. These lesions are thought to represent developmental anomalies of normal venous drainage. These lesions should not be removed, as reports of venous infarcts have been reported. When found in association with a CCM that needs resection, great care should be taken not to disrupt the angioma.
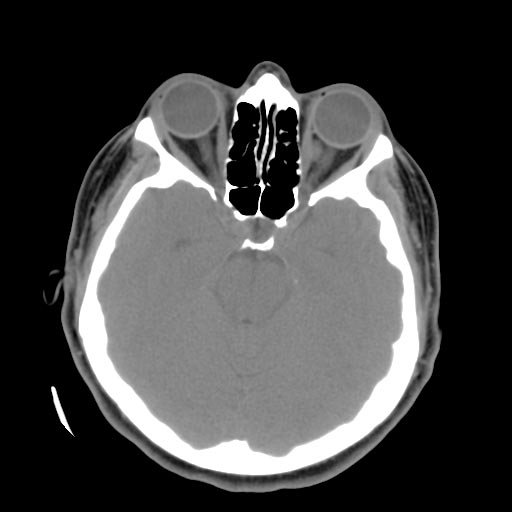
Left Orbital Cavernous Hemangioma
Frontal and temporal lobes are the most common sites of occurrence, and 80-90% of the lesions are supratentorial.
CCM can also be subdivided into two, according to its pattern of occurrence: [1]
- Familial or Hereditary CCM
- Constitutes 20% of all cavernous angioma cases
- Occurs as multiple lesions
- Can have frameshift, nonsense or splice-site mutations
- Can also have deletions or duplication of exons [1]
Genetics
Genes involved in the pathogenesis of cavernous angioma include: [3][4][5]
| Gene | Gene Locus | Chromosome Location | Function |
|---|---|---|---|
| CCM1 | KRIT1 | 7q | regulation of angiogenesis |
| CCM2 | CCM2 | 7p | regulation of angiogenesis, maintenance of vessel integrity, and stabilization of endothelial cell junction |
| CCM3 | PDCD10 | 3q | stimulation of cell proliferation, regulation of apoptosis, regulation of heart development, angiogenesis, vasculogenesis and hematopoiesis |
General Pathology
- Cavernous angioma is diagnosed using clinical imaging.
Microscopic Pathology
- Key feature: Absence of muscular layer in the vessel wall.
 |
References
- ↑ 1.0 1.1 Akers A, Al-Shahi Salman R, A Awad I, Dahlem K, Flemming K, Hart B; et al. (2017). "Synopsis of Guidelines for the Clinical Management of Cerebral Cavernous Malformations: Consensus Recommendations Based on Systematic Literature Review by the Angioma Alliance Scientific Advisory Board Clinical Experts Panel". Neurosurgery. 80 (5): 665–680. doi:10.1093/neuros/nyx091. PMC 5808153. PMID 28387823.
- ↑ Dalyai RT, Ghobrial G, Awad I, Tjoumakaris S, Gonzalez LF, Dumont AS; et al. (2011). "Management of incidental cavernous malformations: a review". Neurosurg Focus. 31 (6): E5. doi:10.3171/2011.9.FOCUS11211. PMID 22133177.
- ↑ Choquet H, Pawlikowska L, Lawton MT, Kim H (2015). "Genetics of cerebral cavernous malformations: current status and future prospects". J Neurosurg Sci. 59 (3): 211–20. PMC 4461471. PMID 25900426.
- ↑ Kim J (2016). "Introduction to cerebral cavernous malformation: a brief review". BMB Rep. 49 (5): 255–62. doi:10.5483/bmbrep.2016.49.5.036. PMC 5070704. PMID 26923303.
- ↑ 5.0 5.1 Zafar A, Quadri SA, Farooqui M, Ikram A, Robinson M, Hart BL; et al. (2019). "Familial Cerebral Cavernous Malformations". Stroke. 50 (5): 1294–1301. doi:10.1161/STROKEAHA.118.022314. PMC 6924279 Check
|pmc=value (help). PMID 30909834.