Testicular cancer natural history, complications and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
*Tends to metastasize to lungs, brain, liver, peritoneum, and others | *Tends to metastasize to lungs, brain, liver, peritoneum, and others | ||
*Affects most male patients in the second and third decade of their life<ref name="pmid20057969">{{cite journal |vauthors=Lee SC, Kim KH, Kim SH, Lee NS, Park HS, Won JH |title=Mixed testicular germ cell tumor presenting as metastatic pure choriocarcinoma involving multiple lung metastases that was effectively treated with high-dose chemotherapy |journal=Cancer Res Treat |volume=41 |issue=4 |pages=229–32 |date=December 2009 |pmid=20057969 |pmc=2802842 |doi=10.4143/crt.2009.41.4.229 |url=}}</ref> | *Affects most male patients in the second and third decade of their life<ref name="pmid20057969">{{cite journal |vauthors=Lee SC, Kim KH, Kim SH, Lee NS, Park HS, Won JH |title=Mixed testicular germ cell tumor presenting as metastatic pure choriocarcinoma involving multiple lung metastases that was effectively treated with high-dose chemotherapy |journal=Cancer Res Treat |volume=41 |issue=4 |pages=229–32 |date=December 2009 |pmid=20057969 |pmc=2802842 |doi=10.4143/crt.2009.41.4.229 |url=}}</ref> | ||
Yolk Sac tumor | |||
*Mostly seen in children less than 2 years old | |||
* | |||
Revision as of 20:15, 9 April 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gertrude Djouka, M.D.[2],Rim Halaby, M.D. [3] Shanshan Cen, M.D. [4]
|
Testicular cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Testicular cancer natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Testicular cancer natural history, complications and prognosis |
|
FDA on Testicular cancer natural history, complications and prognosis |
|
CDC on Testicular cancer natural history, complications and prognosis |
|
Testicular cancer natural history, complications and prognosis in the news |
|
Blogs on Testicular cancer natural history, complications and prognosis |
|
Risk calculators and risk factors for Testicular cancer natural history, complications and prognosis |
Overview
Prognosis of testicular cancer is generally good, and the 5-year survival rate is approximately 96.6% (2004-2010).Common complications of testicular cancer include metastasis, bleeding, infection, and infertility.
Natural History
Seminoma
- Seminoma tends to occur in middle aged people
- Rarely metastasize[1]
- Affects people in their 15 and 35 years old
Embryonal Carcinoma
- Median age is 30 years old[1]
- Has most of the component of mixed non seminoma germ tumor[1]
- Tend to metastasize early to lungs, retroperitomeun, and liver[2]
Choriocarcinoma
- Patient presents with early symptoms if there are metastatic lesions[3]
- Early metastasis through hematogenous route
- Tends to metastasize to lungs, brain, liver, peritoneum, and others
- Affects most male patients in the second and third decade of their life[4]
Yolk Sac tumor
- Mostly seen in children less than 2 years old
Complications
Common complications of testicular cancer include:
- Abdomen
- Lungs
- Retroperitoneal area
- Brain
- Post-surgery complications
Prognosis
- Between 2004 and 2010, the 5-year relative survival of patients with testicular cancer was 96.6%.[5]
- When stratified by age, the 5-year relative survival of patients with testicular cancer was 95.4% and 86.4% for patients <65 and ≥ 65 years of age respectively.[5]
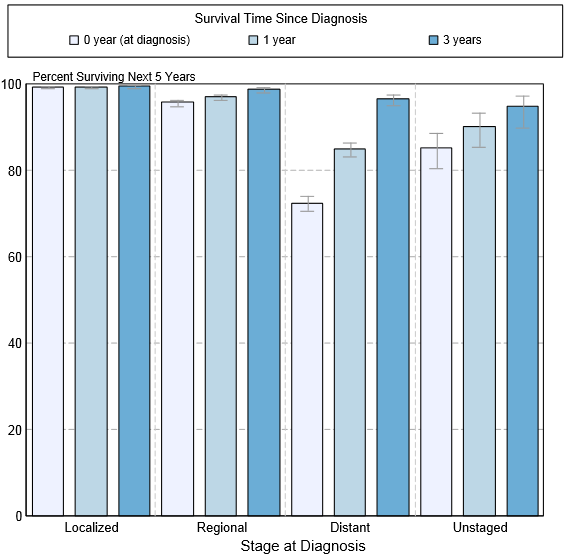
- The survival of patients with testicular cancer varies with the stage of the disease. Shown below is a table depicting the 5-year relative survival by the stage of testicular cancer:[5]
| Stage | 5-year relative survival (%), (2004-2010) |
| All stages | 95.3% |
| Localized | 99.2% |
| Regional | 96% |
| Distant | 73.1% |
| Unstaged | 78.8% |
- Shown below is an image depicting the 5-year conditional relative survival (probability of surviving in the next 5-years given the cohort has already survived 0, 1, 3 years) between 1998 and 2010 of testicular cancer by stage at diagnosis according to SEER. These graphs are adapted from SEER: The Surveillance, Epidemiology, and End Results Program of the National Cancer Institute.[5]
References
- ↑ 1.0 1.1 1.2 Howitt BE, Berney DM (December 2015). "Tumors of the Testis: Morphologic Features and Molecular Alterations". Surg Pathol Clin. 8 (4): 687–716. doi:10.1016/j.path.2015.07.007. PMID 26612222.
- ↑ Ishida M, Hasegawa M, Kanao K, Oyama M, Nakajima Y (February 2009). "Non-palpable testicular embryonal carcinoma diagnosed by ultrasound: a case report". Jpn. J. Clin. Oncol. 39 (2): 124–6. doi:10.1093/jjco/hyn141. PMID 19066212.
- ↑ Lowe K, Paterson J, Armstrong S, Walsh S, Groome M, Mowat C (October 2015). "Metastatic Testicular Choriocarcinoma: A Rare Cause of Upper GI Bleeding". ACG Case Rep J. 3 (1): 36–8. doi:10.14309/crj.2015.94. PMC 4612755. PMID 26504875.
- ↑ Lee SC, Kim KH, Kim SH, Lee NS, Park HS, Won JH (December 2009). "Mixed testicular germ cell tumor presenting as metastatic pure choriocarcinoma involving multiple lung metastases that was effectively treated with high-dose chemotherapy". Cancer Res Treat. 41 (4): 229–32. doi:10.4143/crt.2009.41.4.229. PMC 2802842. PMID 20057969.
- ↑ 5.0 5.1 5.2 5.3 Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, Kosary CL, Yu M, Ruhl J, Tatalovich Z,Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2011, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2011/, based on November 2013 SEER data submission, posted to the SEER web site, April 2014.