WBR0508: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
m (refreshing WBR questions) |
||
| (11 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
{{WBRQuestion | {{WBRQuestion | ||
|QuestionAuthor= | |QuestionAuthor= {{SSK}}(Reviewed by Serge Korjian) | ||
|ExamType=USMLE Step 1 | |ExamType=USMLE Step 1 | ||
|MainCategory=Embryology, Pathology | |MainCategory=Embryology, Pathology | ||
| Line 8: | Line 8: | ||
|MainCategory=Embryology, Pathology | |MainCategory=Embryology, Pathology | ||
|SubCategory=Reproductive | |SubCategory=Reproductive | ||
|MainCategory=Embryology, Pathology | |||
|MainCategory=Embryology, Pathology | |MainCategory=Embryology, Pathology | ||
|MainCategory=Embryology, Pathology | |MainCategory=Embryology, Pathology | ||
| Line 20: | Line 21: | ||
|MainCategory=Embryology, Pathology | |MainCategory=Embryology, Pathology | ||
|SubCategory=Reproductive | |SubCategory=Reproductive | ||
|Prompt=A | |Prompt=A 43-year-old man with history of chronic gastritis presents to the emergency department for several episodes of bloody emesis that started a few hours after his last meal. On admission, the patient is alert and oriented but complains of severe, continuous epigastric pain. His blood pressure is 90/62 mm Hg, heart rate is 130/min, and temperature is 36.7 ᵒC (98 ᵒF). After initial fluid resuscitation, the patient improves and his vitals stabilize. Gastroduodenoscopy reveals a 2.5 cm crusted ulcer in the duodenal bulb. The following day, the patient's hematocrit drops to 6.7 g/dL. He is typed and cross-matched to receives 2 units of red blood cells. Within 10 minutes of initiating the transfusion, the patient complains of generalized pruritus. Physical exam reveals a skin rash apparent mostly on the trunk and upper extremities (shown below). The transfusion is discontinued and vitals remain stable. The patient does not develop fever over the next 4 hours. Which of the following most likely etiology of the transfusion reaction in this patient? | ||
<br> | <br> | ||
[[File:WBR0508.jpg|600px]] | |||
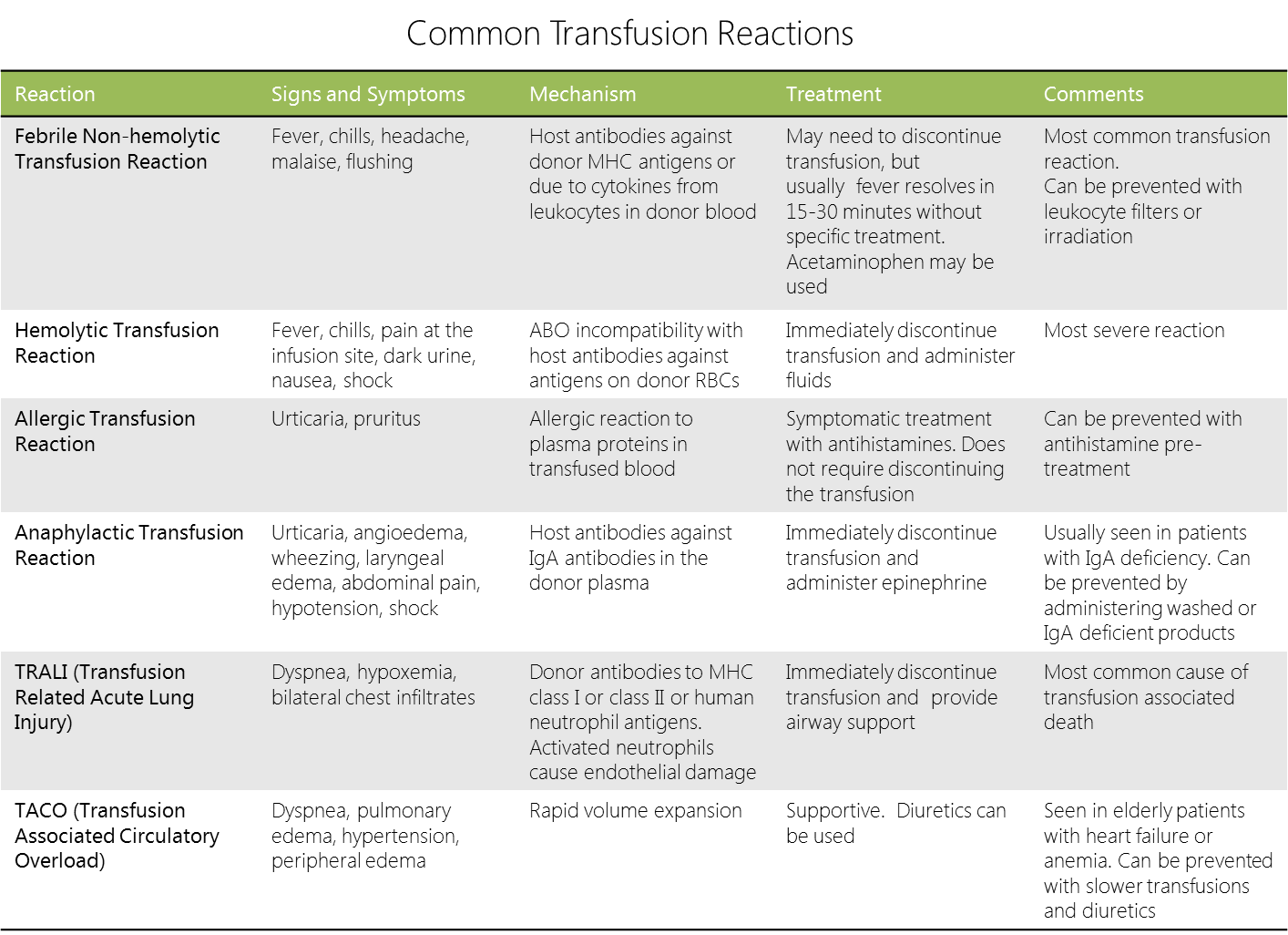
|Explanation=Acute transfusion reactions classically present during or within 24 hours of a blood transfusion. They require instant recognition and intervention to prevent further injury. The most severe form of transfusion reaction is ABO mismatch causing hemolysis and possibly disseminated intravascular coagulopathy. More benign forms include non-hemolytic febrile reactions and non-anaphylactic allergic reactions. Simple allergic transfusion reactions, such as in this patient, usually present with isolated urticaria (hives) and pruritus similar to most food and drug allergies. These reactions are good examples of type I hypersensitivity reactions. Allergic transfusion reactions are IgE-mediated reactions to plasma protein products and antibodies in the donor blood. These proteins activate IgE-primed mast cell that release histamine and other vasoactive mediators. In patients with allergic transfusion reactions, the transfusion can be continued (unlike this patient), and symptomatic treatment with rapid-acting antihistamines should be initiated. To prevent recurrence, pretreatment with antihistamines may be warranted in these patients. A more severe form of allergic transfusion reaction is anaphylaxis secondary to anti-IgA immunoglobulin found in recipients who are natively IgA deficient. These patients require washed or IgA-deficient blood products. In case of suspected anaphylaxis, immediate discontinuation of the transfusion and epinephrine administration is recommended. | |||
[[File:Transfusion_reactions.png|1000px]] | |||
|AnswerA= | |AnswerA=Plasma proteins in transfused blood | ||
|AnswerAExp= | |AnswerAExp=Allergic transfusion reactions are due to activation of IgE-primed mast cells by plasma proteins found in the donor transfused blood. | ||
|AnswerB= | |AnswerB=Cytokines from leukocytes in donor blood | ||
|AnswerBExp= | |AnswerBExp=One of the mechanisms of non-hemolytic febrile transfusion reactions involves a reaction to cytokines produced by leukocytes in the donor blood. These cytokines do not invoke an allergic type I hypersensitivity reaction. | ||
|AnswerC= | |AnswerC=Host antibodies against antigens on donor RBCs | ||
|AnswerCExp= | |AnswerCExp=Transfusion ABO incompatibility is relatively uncommon, but still occurs due to medical errors. Hemolytic transfusion reactions due to ABO mismatch are caused by host antibodies against the main (A/B) antigens on donor RBCs. | ||
| | |AnswerD=Host antibodies against donor MHC antigens | ||
| | |AnswerDExp=Another main mechanism of non-hemolytic febrile transfusion reactions is host antibodies against donor MHC antigens found on leukocytes. This mechanism does not invoke an allergic reaction. It can be preveented by using leukocyte filters or blood irradiation. | ||
| | |AnswerE=Host antibodies against donor IgA molecules | ||
| | |AnswerEExp=The main etiology of anaphylaxis in patients undergoing transfusions is host antibodies against donor IgA molecules, particularly in patients who are IgA-deficient. These patients might have urticaria, but their symptoms are much more severe, and if untreated progress to cardiovascular collapse. | ||
|EducationalObjectives=Allergic transfusion reactions usually present with urticaria and pruritus similar to most food and drug allergies. These reactions are good examples of type I hypersensitivity reactions. Allergic transfusion reactions are IgE-mediated reactions to plasma protein products and antibodies in the donor blood. | |||
|References=Squires JE. Risks of transfusion. South Med J. 2011;104(11):762-9. | |||
|RightAnswer=A | |RightAnswer=A | ||
|WBRKeyword= | |WBRKeyword=transfusion, transfusion reactions, IgA, non-hemolytic febrile transfusion reaction, NHFTR, hypersensitivity reactions, hypersensitivity, blood transfusion | ||
|Approved=Yes | |Approved=Yes | ||
}} | }} | ||
Latest revision as of 00:48, 28 October 2020
| Author | [[PageAuthor::Serge Korjian M.D.(Reviewed by Serge Korjian)]] |
|---|---|
| Exam Type | ExamType::USMLE Step 1 |
| Main Category | MainCategory::Embryology, MainCategory::Pathology |
| Sub Category | SubCategory::Reproductive |
| Prompt | [[Prompt::A 43-year-old man with history of chronic gastritis presents to the emergency department for several episodes of bloody emesis that started a few hours after his last meal. On admission, the patient is alert and oriented but complains of severe, continuous epigastric pain. His blood pressure is 90/62 mm Hg, heart rate is 130/min, and temperature is 36.7 ᵒC (98 ᵒF). After initial fluid resuscitation, the patient improves and his vitals stabilize. Gastroduodenoscopy reveals a 2.5 cm crusted ulcer in the duodenal bulb. The following day, the patient's hematocrit drops to 6.7 g/dL. He is typed and cross-matched to receives 2 units of red blood cells. Within 10 minutes of initiating the transfusion, the patient complains of generalized pruritus. Physical exam reveals a skin rash apparent mostly on the trunk and upper extremities (shown below). The transfusion is discontinued and vitals remain stable. The patient does not develop fever over the next 4 hours. Which of the following most likely etiology of the transfusion reaction in this patient? |
| Answer A | AnswerA::Plasma proteins in transfused blood |
| Answer A Explanation | AnswerAExp::Allergic transfusion reactions are due to activation of IgE-primed mast cells by plasma proteins found in the donor transfused blood. |
| Answer B | AnswerB::Cytokines from leukocytes in donor blood |
| Answer B Explanation | AnswerBExp::One of the mechanisms of non-hemolytic febrile transfusion reactions involves a reaction to cytokines produced by leukocytes in the donor blood. These cytokines do not invoke an allergic type I hypersensitivity reaction. |
| Answer C | AnswerC::Host antibodies against antigens on donor RBCs |
| Answer C Explanation | AnswerCExp::Transfusion ABO incompatibility is relatively uncommon, but still occurs due to medical errors. Hemolytic transfusion reactions due to ABO mismatch are caused by host antibodies against the main (A/B) antigens on donor RBCs. |
| Answer D | AnswerD::Host antibodies against donor MHC antigens |
| Answer D Explanation | [[AnswerDExp::Another main mechanism of non-hemolytic febrile transfusion reactions is host antibodies against donor MHC antigens found on leukocytes. This mechanism does not invoke an allergic reaction. It can be preveented by using leukocyte filters or blood irradiation.]] |
| Answer E | AnswerE::Host antibodies against donor IgA molecules |
| Answer E Explanation | [[AnswerEExp::The main etiology of anaphylaxis in patients undergoing transfusions is host antibodies against donor IgA molecules, particularly in patients who are IgA-deficient. These patients might have urticaria, but their symptoms are much more severe, and if untreated progress to cardiovascular collapse.]] |
| Right Answer | RightAnswer::A |
| Explanation | [[Explanation::Acute transfusion reactions classically present during or within 24 hours of a blood transfusion. They require instant recognition and intervention to prevent further injury. The most severe form of transfusion reaction is ABO mismatch causing hemolysis and possibly disseminated intravascular coagulopathy. More benign forms include non-hemolytic febrile reactions and non-anaphylactic allergic reactions. Simple allergic transfusion reactions, such as in this patient, usually present with isolated urticaria (hives) and pruritus similar to most food and drug allergies. These reactions are good examples of type I hypersensitivity reactions. Allergic transfusion reactions are IgE-mediated reactions to plasma protein products and antibodies in the donor blood. These proteins activate IgE-primed mast cell that release histamine and other vasoactive mediators. In patients with allergic transfusion reactions, the transfusion can be continued (unlike this patient), and symptomatic treatment with rapid-acting antihistamines should be initiated. To prevent recurrence, pretreatment with antihistamines may be warranted in these patients. A more severe form of allergic transfusion reaction is anaphylaxis secondary to anti-IgA immunoglobulin found in recipients who are natively IgA deficient. These patients require washed or IgA-deficient blood products. In case of suspected anaphylaxis, immediate discontinuation of the transfusion and epinephrine administration is recommended.
|
| Approved | Approved::Yes |
| Keyword | WBRKeyword::transfusion, WBRKeyword::transfusion reactions, WBRKeyword::IgA, WBRKeyword::non-hemolytic febrile transfusion reaction, WBRKeyword::NHFTR, WBRKeyword::hypersensitivity reactions, WBRKeyword::hypersensitivity, WBRKeyword::blood transfusion |
| Linked Question | Linked:: |
| Order in Linked Questions | LinkedOrder:: |