Infectious disease laboratory findings: Difference between revisions
Saumya Easaw (talk | contribs) |
m (Bot: Removing from Primary care) |
||
| (13 intermediate revisions by one other user not shown) | |||
| Line 8: | Line 8: | ||
==Laboratory Findings== | ==Laboratory Findings== | ||
====Microbial Culture==== | ====Microbial Culture==== | ||
[[Image:K pneumoniae M morganii providencia styphimuriuma.JPG| | [[Image:K pneumoniae M morganii providencia styphimuriuma.JPG|left|200px|Four nutrient agar plates growing colonies of common Gram negative bacteria.]] | ||
[[Microbiological culture]] is a principal tool used to diagnose infectious disease. In a microbial culture, a [[growth medium]] is provided for a specific agent. A sample taken from potentially diseased tissue or fluid is then tested for the presence of an infectious agent able to grow within that medium. Most pathogenic bacteria are easily grown on nutrient [[agar]], a form of solid medium that supplies carbohydrates and proteins necessary for growth of a bacterium, along with copious amounts of water. A single bacterium will grow into a visible mound on the surface of the plate called a [[Colony (biology)|colony]], which may be separated from other colonies or melded together into a "lawn". The size, color, shape and form of a colony is characteristic of the bacterial species, its specific genetic makeup (its strain), and the environment which supports its growth. Other ingredients are often added to the plate to aid in identification. Plates may contain substances that permit the growth of some bacteria and not others, or that change color in response to certain bacteria and not others. Bacteriological plates such as these are commonly used in the clinical identification of infectious [[bacterium|bacteria]]. Microbial culture may also be used in the identification of [[virus]]es: the medium in this case being cells grown in culture that the virus can infect, and then alter or kill. In the case of viral identification, a region of dead cells results from viral growth, and is called a "plaque". [[Eukaryotic]][[parasites]] may also be grown in culture as a means of identifying a particular agent. | [[Microbiological culture]] is a principal tool used to diagnose infectious disease. In a microbial culture, a [[growth medium]] is provided for a specific agent. A sample taken from potentially diseased tissue or fluid is then tested for the presence of an infectious agent able to grow within that medium. Most pathogenic bacteria are easily grown on nutrient [[agar]], a form of solid medium that supplies carbohydrates and proteins necessary for growth of a bacterium, along with copious amounts of water. A single bacterium will grow into a visible mound on the surface of the plate called a [[Colony (biology)|colony]], which may be separated from other colonies or melded together into a "lawn". The size, color, shape and form of a colony is characteristic of the bacterial species, its specific genetic makeup (its strain), and the environment which supports its growth. Other ingredients are often added to the plate to aid in identification. Plates may contain substances that permit the growth of some bacteria and not others, or that change color in response to certain bacteria and not others. Bacteriological plates such as these are commonly used in the clinical identification of infectious [[bacterium|bacteria]]. Microbial culture may also be used in the identification of [[virus]]es: the medium in this case being cells grown in culture that the virus can infect, and then alter or kill. In the case of viral identification, a region of dead cells results from viral growth, and is called a "plaque". [[Eukaryotic]][[parasites]] may also be grown in culture as a means of identifying a particular agent. | ||
| Line 25: | Line 26: | ||
[[Serological]] methods are highly sensitive, specific and often extremely rapid tests used to identify microorganisms. These tests are based upon the ability of an antibody to bind specifically to an antigen. The antigen, usually a protein or carbohydrate made by an infectious agent, is bound by the antibody. This binding then sets off a chain of events that can be visibly obvious in various ways, dependent upon the test. For example, "[[Strep throat]]" is often diagnosed within minutes, and is based on the appearance of antigens made by the causative agent, ''[[Streptococcus pyogenes]]'', that is retrieved from a patients throat with a cotton swab. Serological tests, if available, are usually the preferred route of identification, however the tests are costly to develop and the reagents used in the test often require refrigeration. Some serological methods are extremely costly, although when commonly used, such as with the "strep test", they can be inexpensive. | [[Serological]] methods are highly sensitive, specific and often extremely rapid tests used to identify microorganisms. These tests are based upon the ability of an antibody to bind specifically to an antigen. The antigen, usually a protein or carbohydrate made by an infectious agent, is bound by the antibody. This binding then sets off a chain of events that can be visibly obvious in various ways, dependent upon the test. For example, "[[Strep throat]]" is often diagnosed within minutes, and is based on the appearance of antigens made by the causative agent, ''[[Streptococcus pyogenes]]'', that is retrieved from a patients throat with a cotton swab. Serological tests, if available, are usually the preferred route of identification, however the tests are costly to develop and the reagents used in the test often require refrigeration. Some serological methods are extremely costly, although when commonly used, such as with the "strep test", they can be inexpensive. | ||
====Molecular | ====Molecular Diagnostics==== | ||
Technologies based upon the [[polymerase chain reaction]] (PCR) will become nearly ubiquitous gold standards of diagnostics of the near future, for several reasons. First, the catalog of infectious agents has grown to the point that virtually all of the significant infectious agents of the human population have been identified. Second, an infectious agent must grow within the human body to cause disease; essentially it must amplify its own nucleic acids in order to cause a disease. This amplification nucleic acid in infected tissue offers an opportunity to detect the infectious agent by using [[PCR]]. Third, the essential tools for generating PCR (primers) are defined by the genomes of the infectious agents, and with time those genomes will be known, if they are not already. | Technologies based upon the [[polymerase chain reaction]] (PCR) will become nearly ubiquitous gold standards of diagnostics of the near future, for several reasons. First, the catalog of infectious agents has grown to the point that virtually all of the significant infectious agents of the human population have been identified. Second, an infectious agent must grow within the human body to cause disease; essentially it must amplify its own nucleic acids in order to cause a disease. This amplification nucleic acid in infected tissue offers an opportunity to detect the infectious agent by using [[PCR]]. Third, the essential tools for generating PCR (primers) are defined by the genomes of the infectious agents, and with time those genomes will be known, if they are not already. | ||
| Line 32: | Line 33: | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[Category:Infectious disease|*]] | [[Category:Infectious disease|*]] | ||
[[Category:Disease]] | [[Category:Disease]] | ||
Latest revision as of 22:23, 29 July 2020
|
Infectious disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Infectious disease laboratory findings On the Web |
|
American Roentgen Ray Society Images of Infectious disease laboratory findings |
|
Risk calculators and risk factors for Infectious disease laboratory findings |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [3]
Overview
Diagnosis of infectious disease is nearly always initiated by medical history and physical examination. More detailed identification techniques involve the culture of infectious agents isolated from a patient. Culture allows identification of infectious organisms by examining their microscopic features, by detecting the presence of substances produced by pathogens, and by directly identifying an organism by its genotype. The benefits of identification, however, are often greatly outweighed by the cost, as often there is no specific treatment, the cause is obvious, or the outcome of an infection is benign.
Laboratory Findings
Microbial Culture
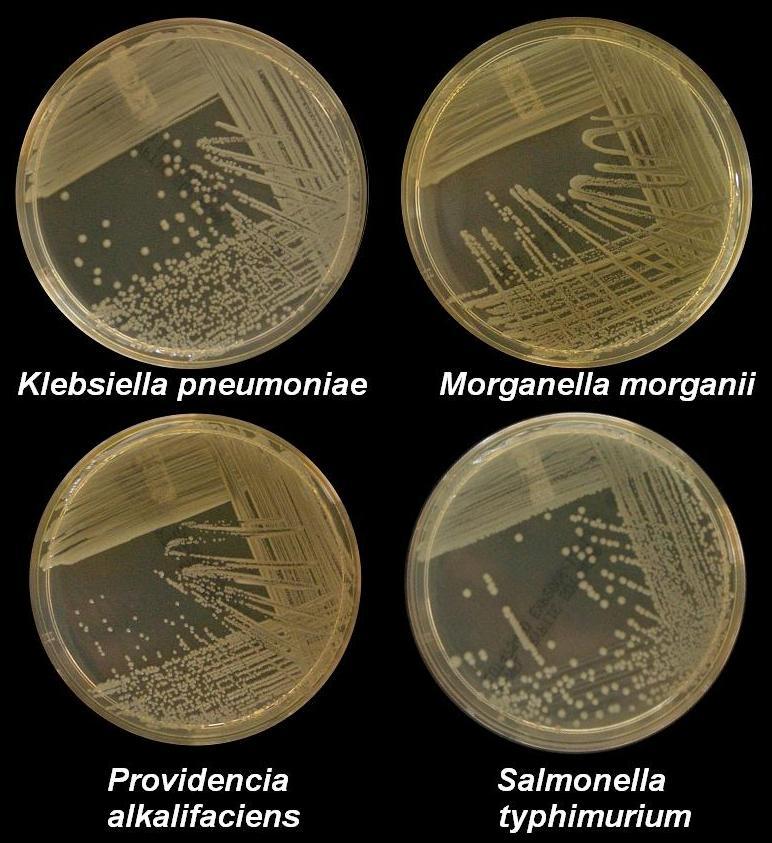
Microbiological culture is a principal tool used to diagnose infectious disease. In a microbial culture, a growth medium is provided for a specific agent. A sample taken from potentially diseased tissue or fluid is then tested for the presence of an infectious agent able to grow within that medium. Most pathogenic bacteria are easily grown on nutrient agar, a form of solid medium that supplies carbohydrates and proteins necessary for growth of a bacterium, along with copious amounts of water. A single bacterium will grow into a visible mound on the surface of the plate called a colony, which may be separated from other colonies or melded together into a "lawn". The size, color, shape and form of a colony is characteristic of the bacterial species, its specific genetic makeup (its strain), and the environment which supports its growth. Other ingredients are often added to the plate to aid in identification. Plates may contain substances that permit the growth of some bacteria and not others, or that change color in response to certain bacteria and not others. Bacteriological plates such as these are commonly used in the clinical identification of infectious bacteria. Microbial culture may also be used in the identification of viruses: the medium in this case being cells grown in culture that the virus can infect, and then alter or kill. In the case of viral identification, a region of dead cells results from viral growth, and is called a "plaque". Eukaryoticparasites may also be grown in culture as a means of identifying a particular agent.
In the absence of suitable plate culture techniques, some microbes require culture within live animals. Bacteria such as Mycobacterium leprae and T. pallidum can be grown in animals, although serological and microscopic techniques make the use of live animals unnecessary. Viruses are also usually identified using alternatives to growth in culture or animals. Some viruses may be grown in embryonated eggs. Another useful identification method is Xenodiagnosis, or the use of a vector to support the growth of an infectious agent. Chagas disease is the most significant example, because it is difficult to directly demonstrate the presence of the causative agent,Trypanosoma cruzi in a patient, which therefore makes it difficult to definitively make a diagnosis. In this case, xenodiagnosis involves the use of the vector of the Chaga's agent T. cruzi, an uninfected triatomine bug (subfamily Triatominae), which takes a blood meal from a person suspected of having been infected. The bug is later inspected for growth of T. cruzi within its gut.
Microscopy
Another principle tool in the diagnosis of infectious disease is microscopy. Virtually all of the culture techniques discussed above rely, at some point, on microscopic examination for definitive identification of the infectious agent. Microscopy may be carried out with simple instruments, such as the compound light microscope, or with instruments as complex as an electron microscope. Samples obtained from patients may be viewed directly under the light microscope, and can often rapidly lead to identification. Microscopy is often also used in conjunction with biochemical staining techniques, and can be made exquisitely specific when used in combination withantibody based techniques. For example, the use of antibodies made artificially fluorescent (fluorescently labeled antibodies) can be directed to bind to and identify a specific antigens present on a pathogen. A fluorescence microscope is then used to detect fluorescently labeled antibodies bound to internalized antigens within clinical samples or cultured cells. This technique is especially useful in the diagnosis of viral diseases, where the light microscope is incapable of identifying a virus directly.
Other microscopic procedures may also aid in identifying infectious agents. Almost all cells readily stain with a number of basic dyes due to the electrostatic attraction between negatively charged cellular molecules and the positive charge on the dye. A cell is normally transparent under a microscope, and using a stain increases the contrast of a cell with its background. Staining a cell with a dye such as Giemsa stain or crystal violet allows a microscopist to describe its size, shape, internal and external components and its associations with other cells. The response of bacteria to different staining procedures is used in the taxonomic classification of microbes as well. Two methods, the Gram stain and the acid-fast stain, are the standard approaches used to classify bacteria and to diagnosis of disease. The Gram stain identifies the bacterial groups Firmicutes and Actinobacteria, both of which contain many significant human pathogens. The acid-fast staining procedure identifies the Actinobacterial genera Mycobacterium and Nocardia.
Biochemical Tests
Biochemical tests used in the identification of infectious agents include the detection of metabolic or enzymatic products characteristic of a particular infectious agent. Since bacteria ferment carbohydrates in patterns characteristic of their genus and species, the detection of fermentationproducts is commonly used in bacterial identification. Acids, alcohols and gases are usually detected in these tests when bacteria are grown in selective liquid or solid media.
The isolation of enzymes from infected tissue can also provide the basis of a biochemical diagnosis of an infectious disease. For example, humans can make neither RNA replicases nor reverse transcriptase, and the presence of these enzymes are characteristic of specific types of viral infections. The ability of the viral proteinhemagglutinin to bind red blood cells together into a detectable matrix may also be characterized as a biochemical test for viral infection, although strictly speaking hemagglutinin is not an enzyme and has no metabolic function.
Serological methods are highly sensitive, specific and often extremely rapid tests used to identify microorganisms. These tests are based upon the ability of an antibody to bind specifically to an antigen. The antigen, usually a protein or carbohydrate made by an infectious agent, is bound by the antibody. This binding then sets off a chain of events that can be visibly obvious in various ways, dependent upon the test. For example, "Strep throat" is often diagnosed within minutes, and is based on the appearance of antigens made by the causative agent, Streptococcus pyogenes, that is retrieved from a patients throat with a cotton swab. Serological tests, if available, are usually the preferred route of identification, however the tests are costly to develop and the reagents used in the test often require refrigeration. Some serological methods are extremely costly, although when commonly used, such as with the "strep test", they can be inexpensive.
Molecular Diagnostics
Technologies based upon the polymerase chain reaction (PCR) will become nearly ubiquitous gold standards of diagnostics of the near future, for several reasons. First, the catalog of infectious agents has grown to the point that virtually all of the significant infectious agents of the human population have been identified. Second, an infectious agent must grow within the human body to cause disease; essentially it must amplify its own nucleic acids in order to cause a disease. This amplification nucleic acid in infected tissue offers an opportunity to detect the infectious agent by using PCR. Third, the essential tools for generating PCR (primers) are defined by the genomes of the infectious agents, and with time those genomes will be known, if they are not already.
Thus, the technological ability to detect any infectious agent rapidly and specifically are currently available. The only remaining blockades to the use of PCR as a standard tool of diagnosis are in its cost and application, neither of which is insurmountable. The diagnosis of a few diseases will not benefit from the development of PCR methods, such as some of the clostridial diseases (tetanus and botulism). These diseases are fundamentally biological poisonings by relatively small numbers of infectious bacteria that produce extremely potent neurotoxins. A significant proliferation of the infectious agent does not occur, this limits the ability of PCR to detect the presence of any bacteria.