Total anomalous pulmonary venous connection pathophysiology: Difference between revisions
No edit summary |
|||
| (20 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Template:Total anomalous pulmonary venous connection}} | {{Template:Total anomalous pulmonary venous connection}} | ||
{{CMG}} | {{CMG}}; {{AE}} {{CZ}}; [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu]; [[Priyamvada Singh|Priyamvada Singh, MBBS]][mailto:psingh13579@gmail.com]; '''Assistant Editor-In-Chief:''' [[Kristin Feeney|Kristin Feeney, B.S.]] [mailto:kfeeney@elon.edu] | ||
==Overview== | ==Overview== | ||
In patients of total anomalous pulmonary venous connection (TAPVC) there is a mixing of oxygenated pulmonary venous blood with deoxygenated blood from systemic circulation. | |||
==Pathophysiology== | ==Pathophysiology== | ||
In | Mixing of [[blood]] could occur at three levels i.e. supracardiac, infracardiac and cardiac. In the former two the mixing occurs outside the heart and in latter inside the heart ([[right atrium]]). | ||
This mixed deoxygenated blood is shunted from right-to-left side of heart ([[patent foramen ovale]], [[atrial septal defect]] or [[patent ductus arteriosus]]). This right to left shunting causes [[cyanosis]] in the patient. | |||
Since, the right side of heart is receiving blood both from pulmonary and systemic circulation it leads to development of [[pulmonary hypertension]], right atrial and [[ventricular hypertrophy]]. | |||
Obstructive forms: In the supracardiac form of TAPVC, the obstruction can occur by compression of the ascending vertical vein between the left main stem bronchus and left pulmonary artery. It can also occur as narrowing at the insertion of the vertical vein into the innominate vein. Obstruction is present in almost all cases of infracardiac TAPVC but is uncommon in the cardiac form. | |||
===Images=== | |||
{| align="left" | |||
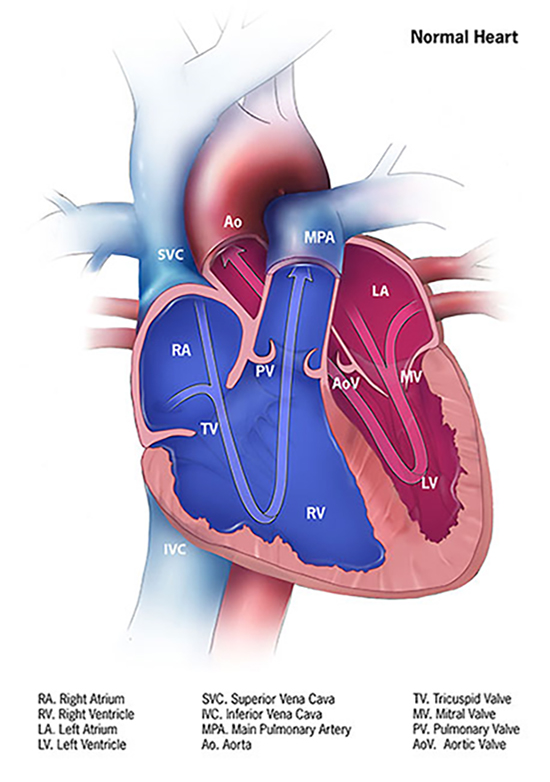
|[[File:Normal-heart-550px.jpg|thumb|none|400px|Normal heart<ref>https://www.cdc.gov/ncbddd/heartdefects/tapvr.html</ref>]] | |||
|} | |||
{| align="center" | |||
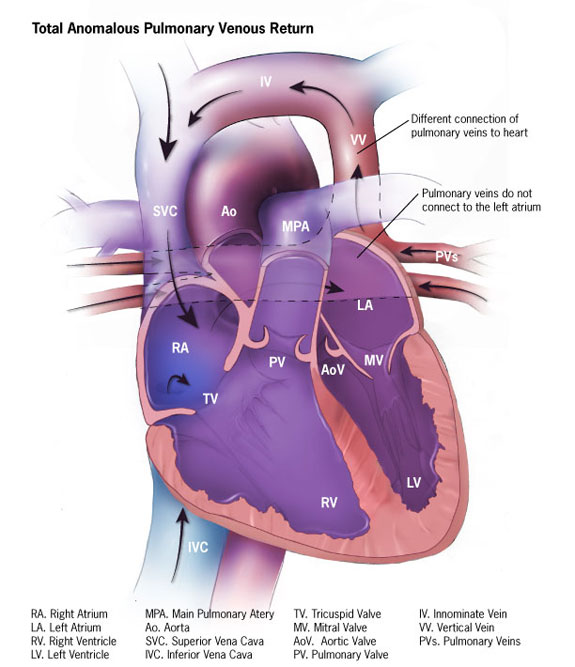
|[[ File:Tapv-575px.jpg|thumb|none|500px|Total anomalous pulmonary venous connection<ref> https://commons.wikimedia.org/wiki/File:Tapv-575px.jpg#/media/File:Tapv-575px.jpg | |||
</ref>]] | |||
|} | |||
==Genetic== | |||
[[Genetic]] [[mutations]] associated with total anomalous pulmonary venous connection include:<ref name="PhelanMcDermid2011">{{cite journal|last1=Phelan|first1=K.|last2=McDermid|first2=H.E.|title=The 22q13.3 Deletion Syndrome (Phelan-McDermid Syndrome)|journal=Molecular Syndromology|year=2011|issn=1661-8777|doi=10.1159/000334260}}</ref><ref name="BleylSaijoh2010">{{cite journal|last1=Bleyl|first1=Steven B.|last2=Saijoh|first2=Yukio|last3=Bax|first3=Noortje A.M.|last4=Gittenberger-de Groot|first4=Adriana C.|last5=Wisse|first5=Lambertus J.|last6=Chapman|first6=Susan C.|last7=Hunter|first7=Jennifer|last8=Shiratori|first8=Hidetaka|last9=Hamada|first9=Hiroshi|last10=Yamada|first10=Shigehito|last11=Shiota|first11=Kohei|last12=Klewer|first12=Scott E.|last13=Leppert|first13=Mark F.|last14=Schoenwolf|first14=Gary C.|title=Dysregulation of the PDGFRA gene causes inflow tract anomalies including TAPVR: integrating evidence from human genetics and model organisms|journal=Human Molecular Genetics|volume=19|issue=7|year=2010|pages=1286–1301|issn=0964-6906|doi=10.1093/hmg/ddq005}}</ref> | |||
==Associated Disorders== | |||
* [[Patent foramen ovale]] | |||
* [[Atrial septal defect]] | |||
* [[Patent ductus arteriosus]] | |||
* [[Pulmonary hypertension]] | |||
==Gross Pathology== | |||
{| align="left" | |||
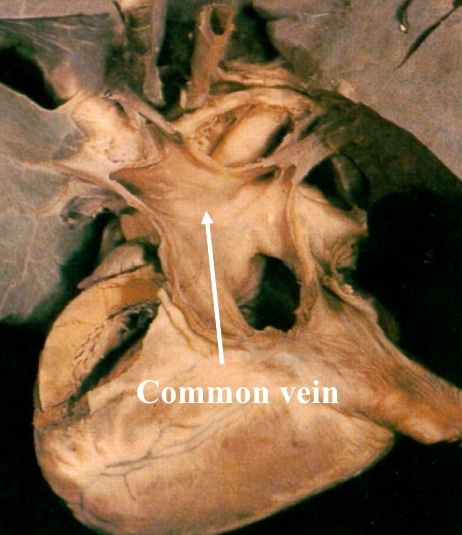
|[[File:CARDIAC TAPVC.jpg|thumb|none|250px|cardiac type of TAPVC with opening of cardiac vein into right atrium | |||
]] | |||
|} | |||
{| align="center" | |||
|[[ File:Supracardiac TAPVC.jpg|thumb|none|220px|supracardiac type of TAPVC with connecting vertical vein]] | |||
|} | |||
===Video=== | |||
Unobstructed forms: No significant stenosis of the pulmonary veins. | |||
Unobstructed forms | |||
{{#ev:youtube|eODH6E_OA_M}} | {{#ev:youtube|eODH6E_OA_M}} | ||
{{#ev:youtube|iiEI5TQ383w}} | {{#ev:youtube|iiEI5TQ383w}} | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
| Line 67: | Line 53: | ||
[[Category:Congenital heart disease]] | [[Category:Congenital heart disease]] | ||
[[Category:Pediatrics]] | [[Category:Pediatrics]] | ||
[[Category:Disease]] | |||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
Latest revision as of 18:59, 25 February 2020
|
Total anomalous pulmonary venous connection Microchapters |
|
Differentiating Total anomalous pulmonary venous connection from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Total anomalous pulmonary venous connection pathophysiology On the Web |
|
American Roentgen Ray Society Images of Total anomalous pulmonary venous connection pathophysiology |
|
FDA on Total anomalous pulmonary venous connection pathophysiology |
|
CDC on Total anomalous pulmonary venous connection pathophysiology |
|
Total anomalous pulmonary venous connection pathophysiology in the news |
|
Blogs on Total anomalous pulmonary venous connection pathophysiology |
|
Risk calculators and risk factors for Total anomalous pulmonary venous connection pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Keri Shafer, M.D. [3]; Priyamvada Singh, MBBS[4]; Assistant Editor-In-Chief: Kristin Feeney, B.S. [5]
Overview
In patients of total anomalous pulmonary venous connection (TAPVC) there is a mixing of oxygenated pulmonary venous blood with deoxygenated blood from systemic circulation.
Pathophysiology
Mixing of blood could occur at three levels i.e. supracardiac, infracardiac and cardiac. In the former two the mixing occurs outside the heart and in latter inside the heart (right atrium).
This mixed deoxygenated blood is shunted from right-to-left side of heart (patent foramen ovale, atrial septal defect or patent ductus arteriosus). This right to left shunting causes cyanosis in the patient.
Since, the right side of heart is receiving blood both from pulmonary and systemic circulation it leads to development of pulmonary hypertension, right atrial and ventricular hypertrophy.
Obstructive forms: In the supracardiac form of TAPVC, the obstruction can occur by compression of the ascending vertical vein between the left main stem bronchus and left pulmonary artery. It can also occur as narrowing at the insertion of the vertical vein into the innominate vein. Obstruction is present in almost all cases of infracardiac TAPVC but is uncommon in the cardiac form.
Images
 |
 |
Genetic
Genetic mutations associated with total anomalous pulmonary venous connection include:[3][4]
Associated Disorders
Gross Pathology
 |
 |
Video
Unobstructed forms: No significant stenosis of the pulmonary veins. {{#ev:youtube|eODH6E_OA_M}}
{{#ev:youtube|iiEI5TQ383w}}
References
- ↑ https://www.cdc.gov/ncbddd/heartdefects/tapvr.html
- ↑ https://commons.wikimedia.org/wiki/File:Tapv-575px.jpg#/media/File:Tapv-575px.jpg
- ↑ Phelan, K.; McDermid, H.E. (2011). "The 22q13.3 Deletion Syndrome (Phelan-McDermid Syndrome)". Molecular Syndromology. doi:10.1159/000334260. ISSN 1661-8777.
- ↑ Bleyl, Steven B.; Saijoh, Yukio; Bax, Noortje A.M.; Gittenberger-de Groot, Adriana C.; Wisse, Lambertus J.; Chapman, Susan C.; Hunter, Jennifer; Shiratori, Hidetaka; Hamada, Hiroshi; Yamada, Shigehito; Shiota, Kohei; Klewer, Scott E.; Leppert, Mark F.; Schoenwolf, Gary C. (2010). "Dysregulation of the PDGFRA gene causes inflow tract anomalies including TAPVR: integrating evidence from human genetics and model organisms". Human Molecular Genetics. 19 (7): 1286–1301. doi:10.1093/hmg/ddq005. ISSN 0964-6906.