Ulnar fracture overview
|
|
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ulnar fracture overview On the Web |
|
American Roentgen Ray Society Images of Ulnar fracture overview |
|
Risk calculators and risk factors for Ulnar fracture overview |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2] ;
Overview
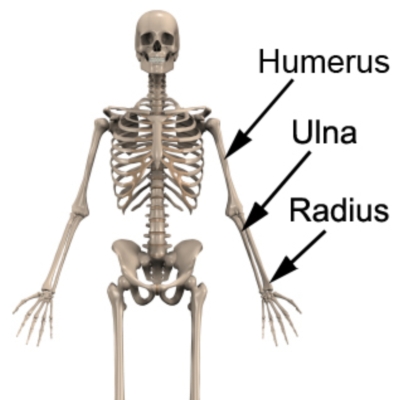
The forearm comprises of 2 long bones: radius and the ulna; they forms joints with the humerus. The ulnar fracture is known as the break in the ulna bone during any trauma affecting this side of body. An ulna as one of the long bones of the forearm is located in in human upper limb and its fracture is a relatively common condition. Forearm bones can break in different ways: they can break into many pieces or can crack just slightly. These broken pieces my line up straight or be in a different location.
Type
- Nightstick fracture: fracture of the middle portion of the ulna without other fractures.
- Hume fracture: fracture of the olecranon with an associated anterior dislocation of the radial head
- Distal ulna fractures: fracture occur along with distal radius fractures.
- Monteggia fracture: fracture of the proximal third of the ulna with the dislocation of the head of the radius
Epidemiology and demographics
According to data from the 2010 National Electronic Injury Surveillance System (NEISS) database and the 2010 US Census, the forearm fractures accounted for 17.8% of all fractures and were the most common type of fracture in the pediatric population (With the range of 0-19 years). National Hospital Ambulatory Medical Care Survey showed that fractures of the radius, the ulna, or both accounted for 44% of all forearm and hand fractures in the United States. The fracture of ulna usually occurs in combination with other injuries such as a sprained or dislocated wrist or elbow, a fractured radius, or other fractures of the hand, wrist or forearm. Based on the affected area during the trauma the severity and type of injuries varies from avulsion fracture, stress fracture, medial epicondyle fracture, olecranon fracture, displaced fracture, un-displaced fracture to the greenstick, comminuted.
Cause
- Direct blow
- road / traffic accidents
- contact sports
- Falling
Sign and Symptoms
- Pain
- Swelling
- Bruising
- Inability to rotate arm
- Numbness in the fingers or wrist
- weakness in the fingers or wrist
Daignosis
- Physical Exam Main step
- X-ray is required to confirm diagnosis
- MRI, CT scan or bone scan for further investigations
Treatment
- Nonsurgical Treatment
- Cast
- Brace
- Surgical Treatment
- Open reduction and internal fixation with plates and screws.
- Open reduction and internal fixation with rods
- External fixation
Prognosis
Using appropriate management such as surgical or conservative treatments for the fractured ulna usually make a full recovery. One of the most important components for recovery is that the patient rests sufficiently. Evaluation of the fracture with follow up X-rays is important to ensure the fracture is healing in an ideal position. Getting back to activity or sport can be found in weeks to months but in patients with severe injuries involving other bones, soft tissue, nerves or blood vessels, recovery time may be somehow prolonged; meanwhile it should be guided by the orthopedic surgeon and treating physiotherapist.
Physiotherapy involving ulna bone:
- Soft tissue massage
- Joint mobilization
- Electrotherapy (e.g. ultrasound)
- Taping or bracing
- Exercises to improve strength and flexibility
- Activity modification
Based on the orthopedic surgeons opinion many types of medicines are available to help manage pain, including opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and local anesthetics.
Cases studies
Related chapters
External link
The American Orthopaedic Association
American Academy of Orthopedic Surgeons