Tricuspid regurgitation echocardiography
|
Tricuspid Regurgitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Tricuspid regurgitation echocardiography On the Web |
|
American Roentgen Ray Society Images of Tricuspid regurgitation echocardiography |
|
Risk calculators and risk factors for Tricuspid regurgitation echocardiography |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Vamsikrishna Gunnam M.B.B.S [2] Rim Halaby, M.D. [3] Fatimo Biobaku M.B.B.S [4] Basir Gill, M.B.B.S, M.D.[5]
Overview
Transthoracic echocardiography (TTE) is usually adequate for the evaluation of tricuspid regurgitation; to confirm the diagnosis, determine the etiology, establish the baseline severity and for the assessment of the function of the right ventricle prior to surgery. In cases of non-diagnostic transthoracic studies, transesophageal echocardiography (TEE) improves the visualization of the valvular structure and delineates the mechanism and severity of regurgitation.
Echocardiography
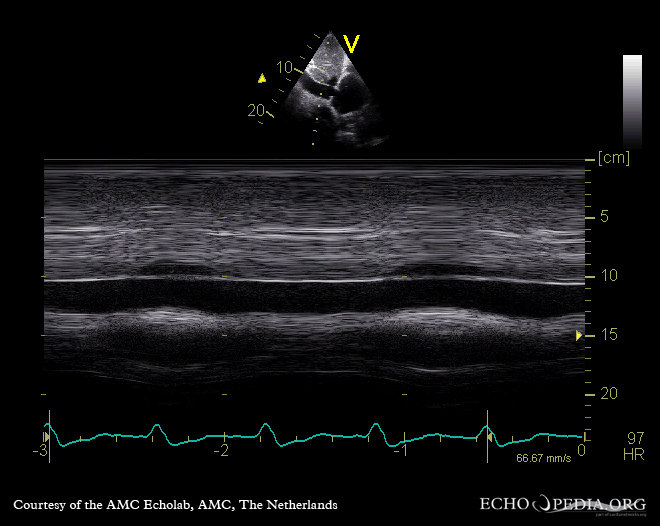
Echocardiography with doppler is the method of choice for the non-invasive detection and evaluation of the severity and etiology of valvular regurgitation. [1][2]Echocardiography allows the evaluation of the following:[3][4][5][6][7][8]
- Right ventricle structure and function
- Right atrium structure and function
- Inferior vena cava
- The structure and function of the left chambers of the heart
- The structures of the tricuspid valve and the underlying etiology of mitral regurgitation
- Pulmonary artery pressure
- Pressures in the heart chambers
- The severity of the tricuspid regurgitation through the measurement of:
- The tricuspid annular diameter in the apical 4-chamber view
- Tricuspid valve leaflet tethering height
- Tricuspid valve leaflet tethering area
- Tricuspid regurgitation jet velocity signal
- Characteristic primary valvular abnormalities can be detected by tricuspid valve motion which includes the conditions like:[9][10]
- Ebstein's anomaly
- Carcinoid heart disease
- Rheumatic valve disease
- Tricuspid valve prolapse
- Flail leaflet
- Endocarditis
- By using the vena contracta method with colour doppler we can estimate the severity of the tricuspid regurgitation and that includes:
- The vena contracta width has to be more than 0.7 cm along with systolic flow reversal in the hepatic veins
- In the presence of atrial fibrillation, systolic flow reversal in the hepatic veins cannot be accurate
- By using the modified Bernoulli equation, we can estimate pulmonary hypertension on echocardiography by measuring the right ventricle to right atrial systolic gradient from the velocity of the tricuspid regurgitation jet
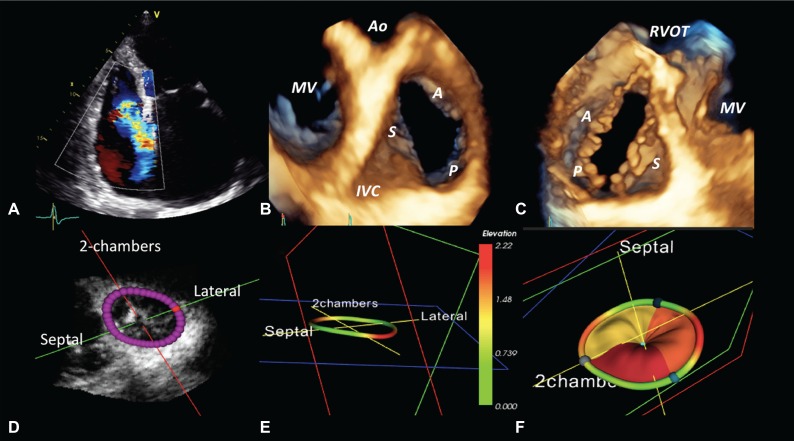
Grading severity of TR
While Transthoracic Echocardiography (TTE) remains the first-line modality, its results are dependent on acoustic windows and operator expertise, which can lead to the underestimation of TR severity.[12] To address consistent underestimation, the 2025 European guidelines have adopted specific cutoffs for 3D vena contracta area (≥75 mm2) and proximal isovelocity surface area (≥75 mm2).[12][13] Comprehensive assessment must include 3D color Doppler to measure the vena contracta area without geometric assumptions, though high-resolution image acquisition remains a challenge.[14] Severity grading has been expanded to a 5-grade scale—including 'massive' and 'torrential' beyond the 'severe' category—which has shown significant prognostic importance for both medical and transcatheter therapies.[15] Transesophageal echocardiography (TEE), specifically 3D TEE, is essential for enhanced valve visualization and provides critical guidance during transcatheter tricuspid valve interventions (TTVI).[16] Assessment of TR severity should ideally be performed when the patient is in a euvolemic state, as the severity can fluctuate significantly based on cardiac loading conditions.[17] Intraprocedural monitoring often utilizes 3D intracardiac echocardiography to supplement TEE, particularly to confirm successful leaflet grasping during edge-to-edge repair procedures.[18][19]
| Mild (1+) | Moderate (2+) | Severe (3+) | Massive (4+) | Torrential (5+) | |
|---|---|---|---|---|---|
| Qualitative | |||||
| Tricuspid
Morphology |
Normal or mildly abnormal | Moderately abnormal | Severely abnormal (flail leaflet, large coaptation gap, marked tethering) | ||
| Color-flow jet area | Small, narrow, central | Moderate central | Large central, or eccentric, wall impinging | ||
| Flow convergence zone | Not visible, transient, or small | Intermediate in size and duration | Large throughout systole | ||
| CW-Doppler contour | Faint, partial,
parabolic |
Dense, parabolic | Dense, parabolic or
triangular |
Dense, often
triangular, may have low peak velocity |
Dense, usually triangular, often low peak velocity |
| Right heart size | Usually normal | Normal or mild
dilation |
Usually dilated | Dilated | |
| Semiquantitative | |||||
| VC width, mm | <3 | 3-6.9 | 7-13.9 | 14-20.9 | ≥21 |
| PISA radius, mm | ≤5.4 | 5.5-8.9 | ≥9 | ||
| Hepatic vein flow | Systolic dominant | Systolic blunting | Systolic flow reversal | ||
| Tricuspid inflow | A-wave dominant | Variable | E-wave dominant (≥1 m/s) | ||
| Quantitative | |||||
| PISA EROA, mm2 | <20 | 20-39 | 40-59 | 60-79 | ≥80 |
| Doppler volumetric | 75-94.9 | 95-114.9 | ≥115 | ||
| EROA, mm2 | |||||
| PISA RegVol, (mL) | <30 | 30-44 | 45-59 | 60-74 | ≥75 |
| RegFrac, % | <15 | 16-49% | ≥50 | ||
| 3D Vena contracta area, mm2 | 75-94.9 | 95-114.9 | ≥115 | ||
2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[22]
Recommendations for Diagnosis of TR
| Class I |
| 1. In patients with TR, TTE is indicated to evaluate the presence and severity of TR, determine the etiology, measure the sizes of the right-sided chambers and inferior vena cava, assess RV systolic function, estimate pulmonary artery systolic pressure, and characterize any associated left-sided heart disease. (Level of Evidence: C-LD)" |
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary[3]
| Class I |
| "1. TTE is indicated to evaluate severity of TR, determine etiology, measure sizes of right-sided chambers and inferior vena cava, assess RV systolic function, estimate pulmonary artery systolic pressure, and characterize any associated left-sided heart disease. (Level of Evidence: C)" |
| Class IIb |
| "1. CMR or real-time 3-dimensional echocardiography may be considered for assessment of RV systolic function and systolic and diastolic volumes in patients with severe TR (stages C and D) and suboptimal 2-dimensional echocardiograms. (Level of Evidence: C)" |
==2008 ACC/AHA Guidelines for the Management of Patients with Valvular Heart Disease - Evaluation of Tricuspid Valve Disease in Adolescents and Young Adults(DO NOT EDIT)[23]
| Class I |
| "1. Doppler echocardiography is indicated for the initial evaluation of adolescent and young adult patients with TR, and serially every 1 to 3 years, depending on severity. (Level C)" |
Sources
- 2008 ACC/AHA Guidelines incorporated into the 2006 guidelines for the management of patients with valvular heart disease. [23]
References
- ↑ Tornos Mas P, Rodríguez-Palomares JF, Antunes MJ (2015). "Secondary tricuspid valve regurgitation: a forgotten entity". Heart. 101 (22): 1840–8. doi:10.1136/heartjnl-2014-307252. PMC 4680164. PMID 26503944.
- ↑ Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA; et al. (2003). "Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography". J Am Soc Echocardiogr. 16 (7): 777–802. doi:10.1016/S0894-7317(03)00335-3. PMID 12835667 PMID: 12835667 Check
|pmid=value (help). - ↑ 3.0 3.1 Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, Guyton RA; et al. (2014). "2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines". Circulation. 129 (23): 2440–92. doi:10.1161/CIR.0000000000000029. PMID 24589852.
- ↑ Chen TE, Kwon SH, Enriquez-Sarano M, Wong BF, Mankad SV (2013). "Three-dimensional color Doppler echocardiographic quantification of tricuspid regurgitation orifice area: comparison with conventional two-dimensional measures". J Am Soc Echocardiogr. 26 (10): 1143–1152. doi:10.1016/j.echo.2013.07.020. PMID 23993694.
- ↑ de Agustin JA, Viliani D, Vieira C, Islas F, Marcos-Alberca P, Gomez de Diego JJ; et al. (2013). "Proximal isovelocity surface area by single-beat three-dimensional color Doppler echocardiography applied for tricuspid regurgitation quantification". J Am Soc Echocardiogr. 26 (9): 1063–72. doi:10.1016/j.echo.2013.06.006. PMID 23860094.
- ↑ Zoghbi, William A.; Adams, David; Bonow, Robert O.; Enriquez-Sarano, Maurice; Foster, Elyse; Grayburn, Paul A.; Hahn, Rebecca T.; Han, Yuchi; Hung, Judy; Lang, Roberto M.; Little, Stephen H.; Shah, Dipan J.; Shernan, Stanton; Thavendiranathan, Paaladinesh; Thomas, James D.; Weissman, Neil J. (2017). "Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation". Journal of the American Society of Echocardiography. 30 (4): 303–371. doi:10.1016/j.echo.2017.01.007. ISSN 0894-7317.
- ↑ Hahn, Rebecca T.; Thomas, James D.; Khalique, Omar K.; Cavalcante, João L.; Praz, Fabien; Zoghbi, William A. (2019). "Imaging Assessment of Tricuspid Regurgitation Severity". JACC: Cardiovascular Imaging. 12 (3): 469–490. doi:10.1016/j.jcmg.2018.07.033. ISSN 1936-878X.
- ↑ Hudzik B, Poloński L, Gąsior M (2016). "Lancisi sign: giant C-V waves of tricuspid regurgitation". Intern Emerg Med. 11 (8): 1139–1140. doi:10.1007/s11739-015-1384-4. PMC 5114320. PMID 26758273.
- ↑ Adler, Dale S. (2017). "Non-functional tricuspid valve disease". Annals of Cardiothoracic Surgery. 6 (3): 204–213. doi:10.21037/acs.2017.04.04. ISSN 2225-319X.
- ↑ Paranon, S.; Acar, P. (2008). "Ebstein's anomaly of the tricuspid valve: from fetus to adult". Heart. 94 (2): 237–243. doi:10.1136/hrt.2006.105262. ISSN 1355-6037.
- ↑ "Revisit of Functional Tricuspid Regurgitation; Current Trends in the Diagnosis and Management".
- ↑ 12.0 12.1 Praz, F., Borger, M. A., Lanz, J., Marin-Cuartas, M., Abreu, A., Adamo, M., Ajmone Marsan, N., Barili, F., Bonaros, N., Cosyns, B., De Paulis, R., Gamra, H., Jahangiri, M., Jeppsson, A., Klautz, R. J. M., Mores, B., Pérez-David, E., Pöss, J., Prendergast, B. D., … Moorjani, N. (2025). 2025 ESC/EACTS Guidelines for the management of valvular heart disease: Developed by the task force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal, 46(44), 4635–4736. https://doi.org/10.1093/eurheartj/ehaf194
- ↑ Tomaselli, M., Penso, M., Badano, L. P., Clement, A., Radu, N., Heilbron, F., Gavazzoni, M., Hădăreanu, D. R., Oliverio, G., Fisicaro, S., Springhetti, P., Pece, C., Delcea, C., & Muraru, D. (2025). Association with outcomes of correcting the proximal isovelocity surface area method to quantitate secondary tricuspid regurgitation. Journal of the American Society of Echocardiography: Official Publication of the American Society of Echocardiography, 38(3), 195–207. https://doi.org/10.1016/j.echo.2024.10.015
- ↑ Lancellotti, P., Pibarot, P., Chambers, J., La Canna, G., Pepi, M., Dulgheru, R., Dweck, M., Delgado, V., Garbi, M., Vannan, M. A., Montaigne, D., Badano, L., Maurovich-Horvat, P., Pontone, G., Vahanian, A., Donal, E., Cosyns, B., & the Scientific Document Committee of the European Association of Cardiovascular Imaging. (2022). Multi-modality imaging assessment of native valvular regurgitation: an EACVI and ESC council of valvular heart disease position paper. European Heart Journal - Cardiovascular Imaging, 23(5), e171–e232. https://doi.org/10.1093/ehjci/jeab253
- ↑ Hahn, R. T., & Zamorano, J. L. (2017). The need for a new tricuspid regurgitation grading scheme. European Heart Journal Cardiovascular Imaging, 18(12), 1342–1343. https://doi.org/10.1093/ehjci/jex139
- ↑ Hahn, R. T., Saric, M., Faletra, F. F., Garg, R., Gillam, L. D., Horton, K., Khalique, O. K., Little, S. H., Mackensen, G. B., Oh, J., Quader, N., Safi, L., Scalia, G. M., & Lang, R. M. (2022). Recommended standards for the performance of transesophageal echocardiographic screening for structural heart intervention: From the American society of echocardiography. Journal of the American Society of Echocardiography: Official Publication of the American Society of Echocardiography, 35(1), 1–76. https://doi.org/10.1016/j.echo.2021.07.006
- ↑ Hahn, R. T., & Zamorano, J. L. (2017). The need for a new tricuspid regurgitation grading scheme. European Heart Journal Cardiovascular Imaging, 18(12), 1342–1343. https://doi.org/10.1093/ehjci/jex139
- ↑ Gilbert H.L. Tang, MD, MSc, MBA, Zaid, S., Hahn, R. T., Aggarwal, V., Alkhouli, M., Aman, E., Berti, S., Chandrashekhar MD DM, Y., Chadderdon, S. M., D’Agostino, A., Fam, N. P., Ho, E. C., Kliger, C., Kodali, S. K., Krishnamoorthy, P., Latib, A., Lerakis, S., Scott Lim, D., Mahadevan, V. S., … von Bardeleben, R. S. (2025). Structural Heart Imaging Using 3-Dimensional Intracardiac Echocardiography: JACC: Cardiovascular Imaging Position Statement. Cardiovascular Imaging. https://doi.org/10.1016/j.jcmg.2024.05.012
- ↑ Wang, L., Tokhi, B., Petrossian, G. A., Chung, W. B., Khalique, O., Cohen, D. J., & Khan, J. M. (2025). Streamlined imaging and procedural workflow for tricuspid transcatheter edge-to-edge repair. JACC. Cardiovascular Imaging, 18(4), 500–510. https://doi.org/10.1016/j.jcmg.2025.01.010
- ↑ Invalid
<ref>tag; no text was provided for refs named:0 - ↑ Hahn, R. T., & Zamorano, J. L. (2017). The need for a new tricuspid regurgitation grading scheme. European Heart Journal Cardiovascular Imaging, 18(12), 1342–1343. https://doi.org/10.1093/ehjci/jex139
- ↑ Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP, Gentile F; et al. (2021). "2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines". Circulation. 143 (5): e72–e227. doi:10.1161/CIR.0000000000000923. PMID 33332150 Check
|pmid=value (help). - ↑ 23.0 23.1 Bonow RO, Carabello BA, Chatterjee K; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172. Unknown parameter
|month=ignored (help)