Liothyronine sodium
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
See full prescribing information for complete Boxed Warning.
|
Overview
Liothyronine sodium is a thyroid supplement that is FDA approved for the {{{indicationType}}} of congenital hypothyroidism, hypothyroidism, myxedema, myxedema coma, simple goiter. There is a Black Box Warning for this drug as shown here. Common adverse reactions include cardiac dysrhythmia, sweating, headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Mild Hypothyroidism
- Dosing Information
- Recommended starting dosage is 25 mcg daily. Daily dosage then may be increased by up to 25 mcg every 1 or 2 weeks. Usual maintenance dose is 25 to75 mcg daily.
- The rapid onset and dissipation of action of liothyronine sodium (T3), as compared with levothyroxine sodium (T4), has led some clinicians to prefer its use in patients who might be more susceptible to the untoward effects of thyroid medication. However, the wide swings in serum T3 levels that follow its administration and the possibility of more pronounced cardiovascular side effects tend to counterbalance the stated advantages.
- Cytomel (liothyronine sodium) Tablets may be used in preference to levothyroxine (T4) during radioisotope scanning procedures, since induction of hypothyroidism in those cases is more abrupt and can be of shorter duration. It may also be preferred when impairment of peripheral conversion of T4 to T3 is suspected.
Myxedema
- Dosing Information
- Recommended starting dosage is 5 mcg daily. This may be increased by 5 to 10 mcg daily every 1 or 2 weeks. When 25 mcg daily is reached, dosage may be increased by 5 to 25 mcg every 1 or 2 weeks until a satisfactory therapeutic response is attained. Usual maintenance dose is 50 to 100 mcg daily.
Myxedema Coma
- Dosing Information
- Myxedema coma is usually precipitated in the hypothyroid patient of long standing by intercurrent illness or drugs such as sedatives and anesthetics and should be considered a medical emergency.
- An intravenous preparation of liothyronine sodium is marketed by Jones Pharma Incorporated, under the trade name Triostat® for use in myxedema coma/precoma.
Simple (non-toxic) Goiter
- Dosing Information
- Recommended starting dosage is 5 mcg daily. This dosage may be increased by 5 to 10 mcg daily every 1 or 2 weeks. When 25 mcg daily is reached, dosage may be increased every week or two by 12.5 or 25 mcg. Usual maintenance dosage is 75 mcg daily.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Liothyronine sodium in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Liothyronine sodium in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Congenital Hypothyroidism
- Dosing Information
- Recommended starting dosage is 5 mcg daily, with a 5 mcg increment every 3 to 4 days until the desired response is achieved. Infants a few months old may require only 20 mcg daily for maintenance. At 1 year, 50 mcg daily may be required. Above 3 years, full adult dosage may be necessary.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Liothyronine sodium in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Liothyronine sodium in pediatric patients.
Contraindications
- Thyroid hormone preparations are generally contraindicated in patients with diagnosed but as yet uncorrected adrenal cortical insufficiency, untreated thyrotoxicosis and apparent hypersensitivity to any of their active or extraneous constituents. There is no well-documented evidence from the literature, however, of true allergic or idiosyncratic reactions to thyroid hormone.
Warnings
|
See full prescribing information for complete Boxed Warning.
|
- The use of thyroid hormones in the therapy of obesity, alone or combined with other drugs, is unjustified and has been shown to be ineffective. Neither is their use justified for the treatment of male or female infertility unless this condition is accompanied by hypothyroidism.
- Thyroid hormones should be used with great caution in a number of circumstances where the integrity of the cardiovascular system, particularly the coronary arteries, is suspected. These include patients with angina pectoris or the elderly, in whom there is a greater likelihood of occult cardiac disease. In these patients, liothyronine sodium therapy should be initiated with low doses, with due consideration for its relatively rapid onset of action. Starting dosage of Cytomel (liothyronine sodium) Tablets is 5 mcg daily, and should be increased by no more than 5 mcg increments at 2-week intervals. When, in such patients, a euthyroid state can only be reached at the expense of an aggravation of the cardiovascular disease, thyroid hormone dosage should be reduced.
- Morphologic hypogonadism and nephrosis should be ruled out before the drug is administered. If hypopituitarism is present, the adrenal deficiency must be corrected prior to starting the drug. Myxedematous patients are very sensitive to thyroid; dosage should be started at a very low level and increased gradually.
- Severe and prolonged hypothyroidism can lead to a decreased level of adrenocortical activity commensurate with the lowered metabolic state. When thyroid-replacement therapy is administered, the metabolism increases at a greater rate than adrenocortical activity. This can precipitate adrenocortical insufficiency. Therefore, in severe and prolonged hypothyroidism, supplemental adrenocortical steroids may be necessary. In rare instances the administration of thyroid hormone may precipitate a hyperthyroid state or may aggravate existing hyperthyroidism.
Precautions
- Thyroid hormone therapy in patients with concomitant diabetes mellitus or insipidus or adrenal cortical insufficiency aggravates the intensity of their symptoms. Appropriate adjustments of the various therapeutic measures directed at these concomitant endocrine diseases are required.
- The therapy of myxedema coma requires simultaneous administration of glucocorticoids.
- Hypothyroidism decreases and hyperthyroidism increases the sensitivity to oral anticoagulants. Prothrombin time should be closely monitored in thyroid-treated patients on oral anticoagulants and dosage of the latter agents adjusted on the basis of frequent prothrombin time determinations. In infants, excessive doses of thyroid hormone preparations may produce craniosynostosis.
- Laboratory Tests
- Treatment of patients with thyroid hormones requires the periodic assessment of thyroid status by means of appropriate laboratory tests besides the full clinical evaluation. The TSH suppression test can be used to test the effectiveness of any thyroid preparation, bearing in mind the relative insensitivity of the infant pituitary to the negative feedback effect of thyroid hormones. Serum T4 levels can be used to test the effectiveness of all thyroid medications except products containing liothyronine sodium. When the total serum T4 is low but TSH is normal, a test specific to assess unbound (free) T4 levels is warranted. Specific measurements of T4 and T3 by competitive protein binding or radioimmunoassay are not influenced by blood levels of organic or inorganic iodine and have essentially replaced older tests of thyroid hormone measurements, i.e., PBI, BEI and T4 by column.
Adverse Reactions
Clinical Trials Experience
- Adverse reactions, other than those indicative of hyperthyroidism because of therapeutic overdosage, either initially or during the maintenance period are rare (see Overdosage).
- In rare instances, allergic skin reactions have been reported with Cytomel (liothyronine sodium) Tablets.
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Liothyronine sodium in the drug label.
Drug Interactions
- Oral Anticoagulants
- Thyroid hormones appear to increase catabolism of vitamin K-dependent clotting factors. If oral anticoagulants are also being given, compensatory increases in clotting factor synthesis are impaired. Patients stabilized on oral anticoagulants who are found to require thyroid replacement therapy should be watched very closely when thyroid is started. If a patient is truly hypothyroid, it is likely that a reduction in anticoagulant dosage will be required. No special precautions appear to be necessary when oral anticoagulant therapy is begun in a patient already stabilized on maintenance thyroid replacement therapy.
- Insulin or Oral Hypoglycemics
- Initiating thyroid replacement therapy may cause increases in insulin or oral hypoglycemic requirements. The effects seen are poorly understood and depend upon a variety of factors such as dose and type of thyroid preparations and endocrine status of the patient. Patients receiving insulin or oral hypoglycemics should be closely watched during initiation of thyroid replacement therapy.
- Cholestyramine
- Cholestyramine binds both T4 and T3 in the intestine, thus impairing absorption of these thyroid hormones. In vitro studies indicate that the binding is not easily removed. Therefore, 4 to 5 hours should elapse between administration of cholestyramine and thyroid hormones.
- Estrogen, Oral Contraceptives
- Estrogens tend to increase serum thyroxine-binding globulin (TBg). In a patient with a nonfunctioning thyroid gland who is receiving thyroid replacement therapy, free levothyroxine may be decreased when estrogens are started thus increasing thyroid requirements. However, if the patient's thyroid gland has sufficient function, the decreased free thyroxine will result in a compensatory increase in thyroxine output by the thyroid. Therefore, patients without a functioning thyroid gland who are on thyroid replacement therapy may need to increase their thyroid dose if estrogens or estrogen-containing oral contraceptives are given.
- Tricyclic Antidepressants
- Use of thyroid products with imipramine and other tricyclic antidepressants may increase receptor sensitivity and enhance antidepressant activity; transient cardiac arrhythmias have been observed. Thyroid hormone activity may also be enhanced.
- Digitalis
- Thyroid preparations may potentiate the toxic effects of digitalis. Thyroid hormonal replacement increases metabolic rate, which requires an increase in digitalis dosage.
- Ketamine
- When administered to patients on a thyroid preparation, this parenteral anesthetic may cause hypertension and tachycardia. Use with caution and be prepared to treat hypertension, if necessary.
- Vasopressors
- Thyroxine increases the adrenergic effect of catecholamines such as epinephrine and norepinephrine. Therefore, injection of these agents into patients receiving thyroid preparations increases the risk of precipitating coronary insufficiency, especially in patients with coronary artery disease. Careful observation is required.
Use in Specific Populations
Pregnancy
- Pregnancy Category A
- Thyroid hormones do not readily cross the placental barrier. The clinical experience to date does not indicate any adverse effect on fetuses when thyroid hormones are administered to pregnant women. On the basis of current knowledge, thyroid replacement therapy to hypothyroid women should not be discontinued during pregnancy.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Liothyronine sodium in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Liothyronine sodium during labor and delivery.
Nursing Mothers
- Minimal amounts of thyroid hormones are excreted in human milk. Thyroid is not associated with serious adverse reactions and does not have a known tumorigenic potential. However, caution should be exercised when thyroid is administered to a nursing woman.
Pediatric Use
- Pregnant mothers provide little or no thyroid hormone to the fetus. The incidence of congenital hypothyroidism is relatively high (1:4000) and the hypothyroid fetus would not derive any benefit from the small amounts of hormone crossing the placental barrier. Routine determinations of serum T4 and/or TSH is strongly advised in neonates in view of the deleterious effects of thyroid deficiency on growth and development.
- Treatment should be initiated immediately upon diagnosis and maintained for life, unless transient hypothyroidism is suspected, in which case, therapy may be interrupted for 2 to 8 weeks after the age of 3 years to reassess the condition. Cessation of therapy is justified in patients who have maintained a normal TSH during those 2 to 8 weeks.
Geriatic Use
- Clinical studies of liothyronine sodium did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy. This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Liothyronine sodium with respect to specific gender populations.
Race
There is no FDA guidance on the use of Liothyronine sodium with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Liothyronine sodium in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Liothyronine sodium in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Liothyronine sodium in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Liothyronine sodium in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Liothyronine sodium in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Liothyronine sodium in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Headache, irritability, nervousness, sweating, arrhythmia (including tachycardia), increased bowel motility and menstrual irregularities. Angina pectoris or congestive heart failure may be induced or aggravated. Shock may also develop. Massive overdosage may result in symptoms resembling thyroid storm. Chronic excessive dosage will produce the signs and symptoms of hyperthyroidism.
Management
- Dosage should be reduced or therapy temporarily discontinued if signs and symptoms of overdosage appear. Treatment may be reinstituted at a lower dosage. In normal individuals, normal hypothalamic-pituitary-thyroidaxis function is restored in 6 to 8 weeks after thyroid suppression.
- Treatment of acute massive thyroid hormone overdosage is aimed at reducing gastrointestinal absorption of the drugs and counteracting central and peripheral effects, mainly those of increased sympathetic activity. Vomiting may be induced initially if further gastrointestinal absorption can reasonably be prevented and barring contraindications such as coma, convulsions, or loss of the gagging reflex. Treatment is symptomatic and supportive. Oxygen may be administered and ventilation maintained. Cardiac glycosides may be indicated if congestive heart failure develops. Measures to control fever, hypoglycemia, or fluid loss should be instituted if needed. Antiadrenergic agents, particularly propranolol, have been used advantageously in the treatment of increased sympathetic activity. Propranolol may be administered intravenously at a dosage of 1 to 3 mg over a 10-minute period or orally, 80 to 160 mg/day, especially when no contraindications exist for its use.
Chronic Overdose
There is limited information regarding Chronic Overdose of Liothyronine sodium in the drug label.
Pharmacology
| |
| |
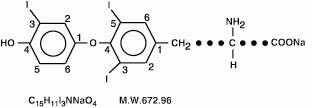
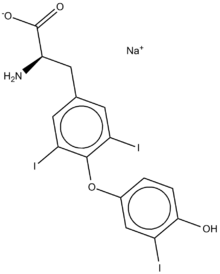
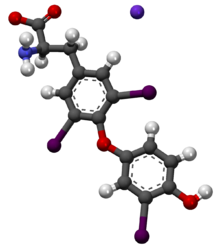
Liothyronine sodium
| |
| Systematic (IUPAC) name | |
| sodium (S)-2-amino-3-[4-(4-hydroxy-3-iodophenoxy)-3,5-diiodophenyl]propanoate | |
| Identifiers | |
| CAS number | |
| ATC code | H03 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 672.96 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 99.7% |
| Metabolism | ? |
| Half life | 2.5 days |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
A(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | ? |
Mechanism of Action
- The mechanisms by which thyroid hormones exert their physiologic action are not well understood. These hormones enhance oxygen consumption by most tissues of the body, increase the basal metabolic rate and the metabolism of carbohydrates, lipids and proteins. Thus, they exert a profound influence on every organ system in the body and are of particular importance in the development of the central nervous system.
Structure
- Thyroid hormone drugs are natural or synthetic preparations containing tetraiodothyronine (T4, levothyroxine) sodium or triiodothyronine (T3, liothyronine) sodium or both. T4 and T3 are produced in the human thyroid gland by the iodination and coupling of the amino acid tyrosine. T4 contains four iodine atoms and is formed by the coupling of two molecules of diiodotyrosine (DIT). T3 contains three atoms of iodine and is formed by the coupling of one molecule of DIT with one molecule of monoiodotyrosine (MIT). Both hormones are stored in the thyroid colloid as thyroglobulin.
- Thyroid hormone preparations belong to two categories: (1) natural hormonal preparations derived from animal thyroid, and (2) synthetic preparations. Natural preparations include desiccated thyroid and thyroglobulin. Desiccated thyroid is derived from domesticated animals that are used for food by man (either beef or hog thyroid), and thyroglobulin is derived from thyroid glands of the hog. The United States Pharmacopeia (USP) has standardized the total iodine content of natural preparations. Thyroid USP contains not less than (NLT) 0.17 percent and not more than (NMT) 0.23 percent iodine, and thyroglobulin contains not less than (NLT) 0.7 percent of organically bound iodine. Iodine content is only an indirect indicator of true hormonal biologic activity.
- Cytomel (liothyronine sodium) Tablets contain liothyronine (L-triiodothyronine or LT3), a synthetic form of a natural thyroid hormone, and is available as the sodium salt.
- The structural and empirical formulas and molecular weight of liothyronine sodium are given below.
- Twenty-five mcg of liothyronine is equivalent to approximately 1 grain of desiccated thyroid or thyroglobulin and 0.1 mg of L-thyroxine.
- Each round, white to off-white Cytomel (liothyronine sodium) tablet contains liothyronine sodium equivalent to liothyronine as follows: 5 mcg debossed KPI and 115; 25 mcg scored and debossed KPI and 116; 50 mcg scored and debossed KPI and 117. Inactive ingredients consist of calcium sulfate, gelatin, starch, stearic acid, sucrose and talc.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Liothyronine sodium in the drug label.
Pharmacokinetics
- Since liothyronine sodium (T3) is not firmly bound to serum protein, it is readily available to body tissues. The onset of activity of liothyronine sodium is rapid, occurring within a few hours. Maximum pharmacologic response occurs within 2 or 3 days, providing early clinical response. The biological half-life is about 2-1/2 days.
- T3 is almost totally absorbed, 95 percent in 4 hours. The hormones contained in the natural preparations are absorbed in a manner similar to the synthetic hormones.
- Liothyronine sodium has a rapid cutoff of activity which permits quick dosage adjustment and facilitates control of the effects of overdosage, should they occur.
- The higher affinity of levothyroxine (T4) for both thyroid-binding globulin and thyroid-binding prealbumin as compared to triiodothyronine (T3) partially explains the higher serum levels and longer half-life of the former hormone. Both protein-bound hormones exist in reverse equilibrium with minute amounts of free hormone, the latter accounting for the metabolic activity.
Nonclinical Toxicology
- A reportedly apparent association between prolonged thyroid therapy and breast cancer has not been confirmed and patients on thyroid for established indications should not discontinue therapy. No confirmatory long-term studies in animals have been performed to evaluate carcinogenic potential, mutagenicity, or impairment of fertility in either males or females.
Clinical Studies
There is limited information regarding Clinical Studies of Liothyronine sodium in the drug label.
How Supplied
- Cytomel (liothyronine sodium) Tablets: 5 mcg in bottles of 100; 25 mcg in bottles of 100; and 50 mcg in bottles of 100.
- 5 mcg 100's: NDC 60793-115-01
- 25 mcg 100's: NDC 60793-116-01
- 50 mcg 100's: NDC 60793-117-01
- Store between 15° and 30°C (59° and 86°F).
Storage
There is limited information regarding Liothyronine sodium Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Liothyronine sodium |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Liothyronine sodium |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Patients on thyroid hormone preparations and parents of pediatric patients on thyroid therapy should be informed that:
- Replacement therapy is to be taken essentially for life, with the exception of cases of transient hypothyroidism, usually associated with thyroiditis, and in those patients receiving a therapeutic trial of the drug.
- They should immediately report during the course of therapy any signs or symptoms of thyroid hormone toxicity, e.g., chest pain, increased pulse rate, palpitations, excessive sweating, heat intolerance, nervousness, or any other unusual event.
- In case of concomitant diabetes mellitus, the daily dosage of antidiabetic medication may need readjustment as thyroid hormone replacement is achieved. If thyroid medication is stopped, a downward readjustment of the dosage of insulin or oral hypoglycemic agent may be necessary to avoid hypoglycemia. At all times, close monitoring of urinary glucose levels is mandatory in such patients.
- In case of concomitant oral anticoagulant therapy, the prothrombin time should be measured frequently to determine if the dosage of oral anticoagulants is to be readjusted.
- Partial loss of hair may be experienced by pediatric patients in the first few months of thyroid therapy, but this is usually a transient phenomenon and later recovery is usually the rule.
Precautions with Alcohol
- Alcohol-Liothyronine sodium interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Cytomel®[1]
Look-Alike Drug Names
There is limited information regarding Liothyronine sodium Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Page Name=Liothyronine sodium |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Liothyronine sodium |Label Name=Liothyronine sodium02.png
}}
{{#subobject:
|Label Page=Liothyronine sodium |Label Name=Liothyronine sodium03.png
}}
{{#subobject:
|Label Page=Liothyronine sodium |Label Name=Liothyronine sodium04.png
}}
{{#subobject:
|Label Page=Liothyronine sodium |Label Name=Liothyronine sodium05.png
}}