Pulmonary embolism case studies
| Resident Survival Guide |
|
Pulmonary Embolism Microchapters |
|
Diagnosis |
|---|
|
Pulmonary Embolism Assessment of Probability of Subsequent VTE and Risk Scores |
|
Treatment |
|
Follow-Up |
|
Special Scenario |
|
Trials |
|
Case Studies |
|
Pulmonary embolism case studies On the Web |
|
Directions to Hospitals Treating Pulmonary embolism case studies |
|
Risk calculators and risk factors for Pulmonary embolism case studies |
Editor(s)-In-Chief: The APEX Trial Investigators, C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Case Studies
Case Study #1
Case Study #2
-
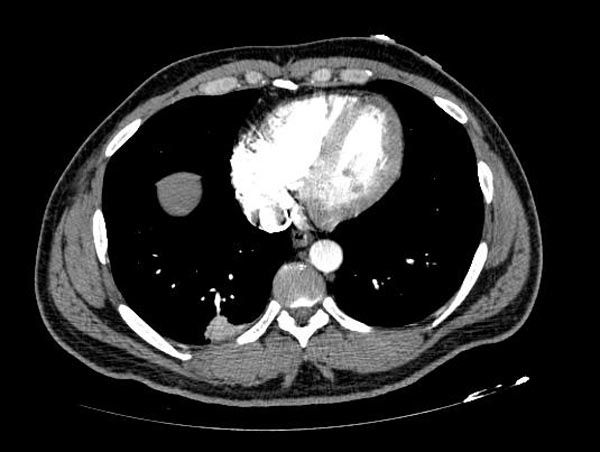
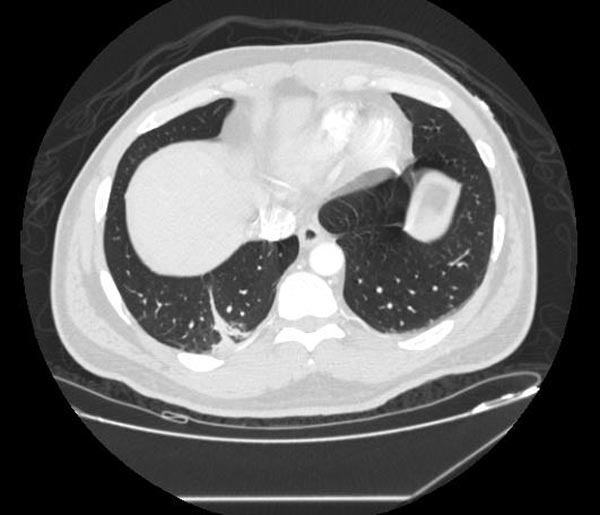
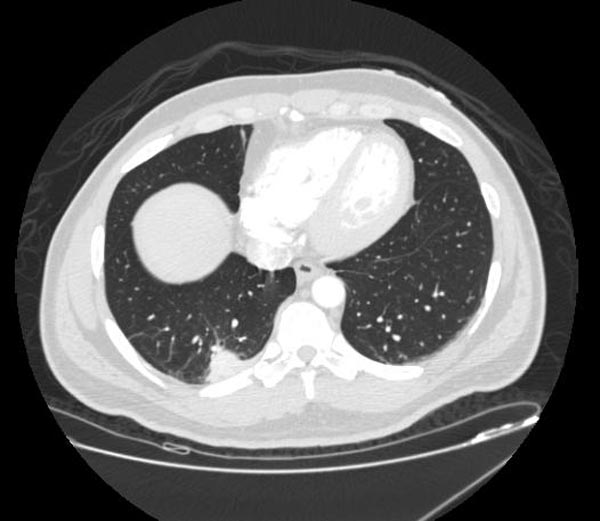
CT: Pulmonary Embolism and Infarction
-
CT: Pulmonary Embolism and Infarction
-
CT: Pulmonary Embolism and Infarction
Case Study #3
- A patient with shortness of breath:
Images shown below are courtesy of RadsWiki and copylefted.
Case Study #4
- A patient who had an acute RBBB;
Images shown below are courtesy of RadsWiki and copylefted.
Case Study #5
Chronic pulmonary embolism (PE) and Deep Venous Thrombosis (DVT): A 49 year old man complains of sudden onset of shortness of breath. Doppler ultrasound examination of the lower extremities revealed femoral vein thrombus. V/Q scan showed complete lack of perfusion of the right lung. A markedly dilated azygous vein is identified. Also, dilated azygous and hemiazygous veins are identified in the retrocrural space. There is acute thrombus within the common iliacs, external and internal iliac veins, and common femoral veins bilaterally. Above the confluence of the common iliac veins, the inferior vena cava is unapparent. Multiple collateral vessels are present around the aorta and the azygous and hemiazygous veins are prominent. The portal venous axis is patent.
(Images shown below are courtesy of Professor Peter Anderson DVM PhD, and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology)
Case Study #6
- Central PE: 76 year old female had right lower lobe resection for stage II non-small cell carcinoma of the lung. Chest X-ray and CT images shown below.
- Chronic pulmonary embolism within the right pulmonary artery.
- Persistence of air within the decreased right pleural fluid collection with adjacent retraction of inflamed esophagus raises the suspicion for esophageal pleural fistula.
(Courtesy of Professor Peter Anderson DVM PhD © PEIR, University of Alabama at Birmingham, Department of Pathology)
Case Study #7
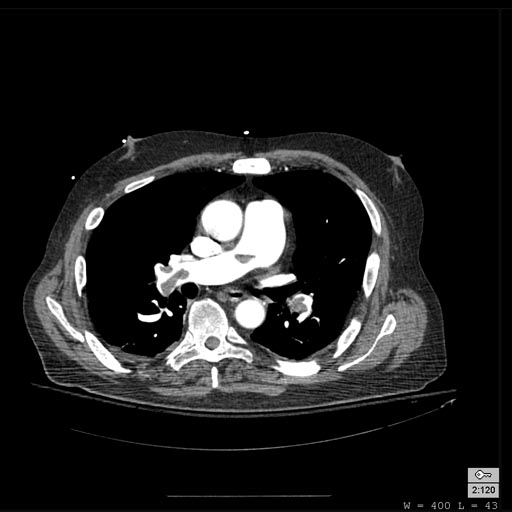
- Bilateral PE: A 74 year old male with recently diagnosed diabetes mellitus who presents with left sided chest pain and abdominal pain with a 50 pound weight loss.
The scan is performed to evaluate for occult malignancy. The patient has an apparent pulmonary embolus. Thoracoabdominal CT findings are as follow:
- Bilateral pulmonary thromboemboli involving both upper and both lower lobe pulmonary arteries, greater on the right side.
- Wedge shaped, pleural based opacities in the left upper lobe which may represent pleural effusions are probably related to the emboli.
- Dilated right ventricle. This may also be related to the pulmonary emboli.
- No signs of mass or lymphadenopathy.
- No evidence of malignancy or other significant abnormality within the abdomen or pelvis.
- Incidental findings included small calcification in the right adrenal gland, small left renal cyst, and enlarged prostate gland.
{Images shown below are courtesy of Professor Peter Anderson DVM PhD, and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology)