Multi-drug-resistant tuberculosis CT
|
Multi-drug-resistant tuberculosis Microchapters |
|
Differentiating Multi-drug-resistant tuberculosis from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Multi-drug-resistant tuberculosis CT On the Web |
|
American Roentgen Ray Society Images of Multi-drug-resistant tuberculosis CT |
|
Directions to Hospitals Treating Multi-drug-resistant tuberculosis |
|
Risk calculators and risk factors for Multi-drug-resistant tuberculosis CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Overview
The majority of patients with pulmonary tuberculosis will have abnormal findings in a chest CT, which include micronodules, interlobular septal thickening, cavitation and consolidation. CT scan is more sensitive than an X-ray to detect lymphadenopathies.
Computed Tomography
Pulmonary Tuberculosis
- Chest CT abnormalities are seen in the majority of patients with active pulmonary tuberculosis.
- CT findings include:[1]
- Micronodules
- Most commonly located in the subpleural region and peribronchovascular interstitium.
- CT scan allows an early and accurate detection of micronodules.
- Interlobular septal thickening
- Cavitation is the most important finding in secondary tuberculosis
- Appears as a lesion with thick walls and irregular margins.
- It may be observed in almost 50% of patients.
- It is most commonly seen in the upper lung.
- Cavities in the lower lung can be found in diabetes and HIV infection.[2][3]
- Although it is rare, cavities may be superinfected and an air-fluid level is seen inside the cavity.
- After the active infection is treated, small cavities with thin walls may remain as a residual finding.
- Homogeneous and dense consolidation
- CT is more sensitive to detect hiliar lymphadenpathy.
- The "tree-in-bud" sign is a CT finding that may be seen in pulmonary tuberculosis and it is caused by mucus or pus impaction into the small airways that accentuates the branching course of peripheral airways.[4]
 Image courtesy of Dr Natalie Yang, Radiopedia. (original file here) Creative Commons BY-SA-NC |
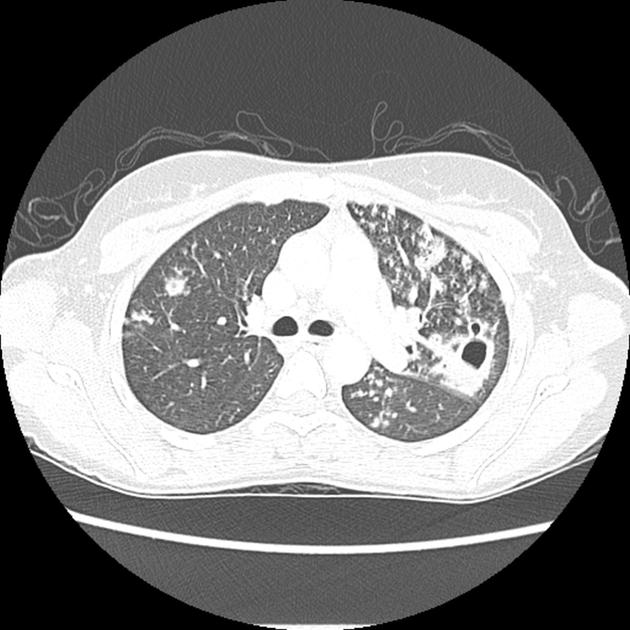 Image courtesy of Dr Natalie Yang, Radiopedia. (original file here) Creative Commons BY-SA-NC  Image courtesy of Wikimedia Commons. |
Extrapulmonary Tuberculosis
Cardiac Tuberculosis
- Pericardial thickening may be seen in a CT, specially if it is more than 3 mm.[5]
- Lymph node enlargment is also a common CT finding in cardiac tuberculosis.[5]
- Pericardial effusion is seen in less than 20% of patients.[5]
Miliary Tuberculosis
CT findings include multiple pulmonary nodules with a diameter of 1-2mm, distributed in a random pattern, pleural effusion may also be present.
 Image courtesy of Dr Frank Gaillard, Radiopedia. (original file here) Creative Commons BY-SA-NC |
 Image courtesy of Dr Frank Gaillard, Radiopedia. (original file here) Creative Commons BY-SA-NC |
Tuberculous Meningitis
- Head CT findings in tuberculous meningitis include meningeal enhancement consistent with meningeal inflammation and choroidal calcifications.[6]
- Areas of infarction and hemorrhage may also be seen in cases of miliar tuberculosis.
- Patients with late complications may show hydrocephalus.

Abdominal Tuberculosis
- CT findings in a pancreatic and spleen infection with tuberculosis may mimic a pancreatic cancer.[7]
- Shown below there is CT scan of the pancreas demonstrating a mass in the pancreatic tail and metastasizes in the spleen.
 |
 |
References
- ↑ Jeong Min Ko, Hyun Jin Park & Chi Hong Kim (2014). "Pulmonary Changes of Pleural Tuberculosis: Up-to-Date CT Imaging". Chest. doi:10.1378/chest.14-0196. PMID 25086249. Unknown parameter
|month=ignored (help) - ↑ Patel, AnandK; Rami, KiranC; Ghanchi, FerozD (2011). "Radiological presentation of patients of pulmonary tuberculosis with diabetes mellitus". Lung India. 28 (1): 70. doi:10.4103/0970-2113.76308. ISSN 0970-2113.
- ↑ Padyana, Mahesha; Bhat, RaghavendraV; Dinesha, M; Nawaz, Alam (2012). "HIV-Tuberculosis: A Study of Chest X-Ray Patterns in Relation to CD4 Count". North American Journal of Medical Sciences. 4 (5): 221. doi:10.4103/1947-2714.95904. ISSN 1947-2714.
- ↑ Eisenhuber, Edith (2002). "The Tree-in-Bud Sign1". Radiology. 222 (3): 771–772. doi:10.1148/radiol.2223991980. ISSN 0033-8419.
- ↑ 5.0 5.1 5.2 Burrill, Joshua; Williams, Christopher J.; Bain, Gillian; Conder, Gabriel; Hine, Andrew L.; Misra, Rakesh R. (2007). "Tuberculosis: A Radiologic Review1". RadioGraphics. 27 (5): 1255–1273. doi:10.1148/rg.275065176. ISSN 0271-5333.
- ↑ Komolafe, Morenikeji A; Sunmonu, Taofiki A; Esan, Olufunmi A (2008). "Tuberculous meningitis presenting with unusual clinical features in Nigerians: Two case reports". Cases Journal. 1 (1): 180. doi:10.1186/1757-1626-1-180. ISSN 1757-1626.
- ↑ Rong, YF; Lou, WH; Jin, DY (2008). "Pancreatic tuberculosis with splenic tuberculosis mimicking advanced pancreatic cancer with splenic metastasizes: a case report". Cases Journal. 1 (1): 84. doi:10.1186/1757-1626-1-84. ISSN 1757-1626.