Lidocaine detailed information
 | |
| Clinical data | |
|---|---|
| Pregnancy category |
|
| Routes of administration | IV, subcutaneous, topical |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 35% (oral) 3% (topical) |
| Metabolism | Hepatic, 90% CYP1A2-mediated |
| Elimination half-life | 1.5–2 hours |
| Excretion | renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
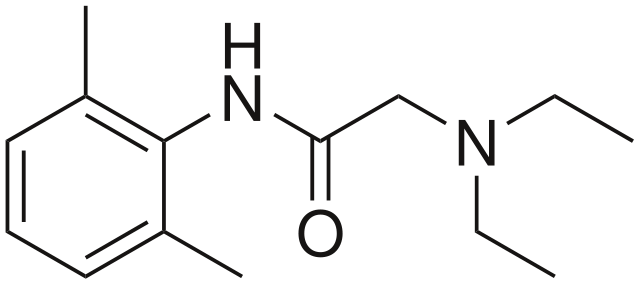
| Formula | C14H22N2O |
| Molar mass | 234.34 g/mol |
| 3D model (JSmol) | |
| Melting point | 68 °C (154.4 °F) |
| |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Lidocaine (INN) (Template:PronEng) or lignocaine (former BAN) (Template:IPA) is a common local anesthetic and antiarrhythmic drug. Lidocaine is used topically to relieve itching, burning and pain from skin inflammations, injected as a dental anesthetic, and in minor surgery. The most commonly encountered lidocaine preparations are marketed by Abraxis Pharmaceutical Products under the brand names Xylocaine and Xylocard, and as 'Lanacane' topical ointment in the UK, though lidocaine is also found in many other proprietary preparations.
History
Lidocaine, the first amino amide-type local anesthetic, was first synthesised under the name xylocaine by Nils Löfgren in 1943.[1] His colleague Bengt Lundqvist made the first injection anesthesia experiments on himself.[1]It was first marketed in 1948.
Pharmacokinetics
Lidocaine has a more rapid onset of action and longer duration of action than amino ester-type local anesthetics such as procaine. It is approximately 90% metabolized in the liver by CYP1A2 (and to a minor extent CYP3A4) to the pharmacologically-active metabolites monoethylglycinexylidide and glycinexylidide.
The elimination half-life of lidocaine is approximately 1.5–2 hours in most patients. This may be prolonged in patients with hepatic impairment (average 343 minutes) or congestive heart failure (average 136 minutes). (Thomson et al., 1973)
Pharmacodynamics
Anesthesia
Lidocaine alters depolarization in neurons, by blocking the fast voltage gated sodium (Na+) channels in the cell membrane. With sufficient blockade, the membrane of the presynaptic neuron will not depolarize and so fail to transmit an action potential, leading to its anesthetic effects. Careful titration allows for a high degree of selectivity in the blockage of sensory neurons, whereas higher concentrations will also affect other modalities of neuron signalling.
Clinical use
Indications
Indications for the use of lidocaine include:
- Topical, infiltration, nerve block, ophthalmic, epidural and intrathecal anaesthesia, IV regional anaesthesia (IVRA)
- Treatment of serious ventricular arrhythmias (IV preparations), including ventricular fibrillation (VF) and ventricular tachycardia (VT) associated with cardiac arrest
Topical lidocaine has been shown to relieve postherpetic neuralgia in some patients, although there is not enough study evidence to recommend it as a first-line treatment. (Khaliq et al., 2007)
Contraindications
Contraindications for the use of lidocaine include:
- Heart block, second or third degree (without pacemaker)
- Severe sinoatrial block (without pacemaker)
- Serious adverse drug reaction to lignocaine or amide local anaesthetics
- Concurrent treatment with quinidine, flecainide, disopyramide, procainamide (Class I antiarrhythmic agents)
- Prior use of Amiodarone Hydrochloride
- Hypotension not due to Arrhythmia
- Bradycardia
- Accelerated idioventricular rhythm
Adverse drug reactions
Adverse drug reactions (ADRs) are rare when lidocaine is used as a local anesthetic and is administered correctly. Most ADRs associated with lidocaine for anesthesia relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, but allergic reactions can rarely occur.
Systemic exposure to excessive quantities of lidocaine mainly result in central nervous system (CNS) and cardiovascular effects – CNS effects usually occur at lower blood plasma concentrations and additional cardiovascular effects present at higher concentrations, though cardiovascular collapse may also occur with low concentrations. CNS effects may include CNS excitation (nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, seizures) followed by depression (drowsiness, loss of consciousness, respiratory depression and apnea). Cardiovascular effects include hypotension, bradycardia, arrhythmias, and/or cardiac arrest – some of which may be due to hypoxemia secondary to respiratory depression. (Rossi, 2006)
ADRs associated with the use of intravenous lidocaine are similar to toxic effects from systemic exposure above. These are dose-related and more frequent at high infusion rates (≥3 mg/minute). Common ADRs include: headache, dizziness, drowsiness, confusion, visual disturbances, tinnitus, tremor, and/or paraesthesia. Infrequent ADRs associated with the use of lidocaine include: hypotension, bradycardia, arrhythmias, cardiac arrest, muscle twitching, seizures, coma, and/or respiratory depression. (Rossi, 2006)
Dosage forms
Lidocaine, usually in the form of lidocaine hydrochloride, is available in various forms including:
- Injected local anesthetic (sometimes combined with epinephrine)
- Dermal patch (sometimes combined with prilocaine)
- Intravenous injection (sometimes combined with epinephrine)
- Intravenous infusion
- Nasal instillation/spray (combined with phenylephrine)
- Oral gel (often referred to as "viscous lidocaine" or abbreviated "lidocaine visc" or "lidocaine hcl visc" in pharmacology; used as teething gel)
- Oral liquid
- Topical gel (as with Aloe Vera gels that include Lidocaine)
- Topical liquid
- Topical patch (Lidocaine 5% patch is marketed as "Lidoderm" in the US (since 1999) and "Versatis" in the UK (since 2007 by Grünenthal))
Additive in cocaine
Lidocaine is often added to cocaine as a diluent. Cocaine numbs the gums when applied, and since lidocaine causes stronger gingival numbness, customers get the impression of high-quality cocaine when checking the purity this way even if the substance is of poor quality. Usage of lidocaine-diluted cocaine is dangerous due to the potential side effects of lidocaine including causing cardiac arrhythmias.
References
- Khaliq W, Alam S, Puri N (2007). "Topical lidocaine for the treatment of postherpetic neuralgia". Cochrane Database Syst Rev (2): CD004846. doi:10.1002/14651858.CD004846.pub2. PMID 17443559.
- Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- Thomson PD, Melmon KL, Richardson JA; et al. (1973). "Lidocaine pharmacokinetics in advanced heart failure, liver disease, and renal failure in humans". Ann. Intern. Med. 78 (4): 499–508. PMID 4694036.
Template:Antiarrhythmic agents Template:Vasoprotectives Template:Antipruritics
Template:Throat preparations
Template:Otologicals
ar:ليدوكائين
cs:Lidokain
da:Lidokain
de:Lidocain
hr:Lidokain
hu:Lidokain
nl:Lidocaïne
fi:Lidokaiini
sv:Lidokain
- Pages with script errors
- Pages with citations using unsupported parameters
- Drugs with non-standard legal status
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Antiarrhythmic agents
- Local anesthetics
- Drugs