Leprosy classification
|
Leprosy Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Leprosy classification On the Web |
|
American Roentgen Ray Society Images of Leprosy classification |
|
Risk calculators and risk factors for Leprosy classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2]Kiran Singh, M.D. [3]
Overview
The Ridley Jopling classification and the WHO classification are the two most widely used systems to classify Leprosy. These classification systems are based on clinical, microbiologic and histopathological features, and are used to determine the patient's prognosis and the treatment regimen.[1][2][3]
Classification
There are different systems for classifying leprosy. However, the two more common classification schemes include the WHO and the Ridley-Jopling systems.
| WHO | Ridley-Jopling | ICD-10 | MeSH | Description | Lepromin test | Immune target |
|---|---|---|---|---|---|---|
| Paucibacillary | Tuberculoid ("TT"), Borderline Tuberculoid ("BT") | A30.1, A30.2 | Tuberculoid | It is characterized by one or more hypopigmented skin macules and anaesthetic patches, where skin sensations are lost because of damaged peripheral nerves that have been attacked by the host's immune cells. | Positive | Bacillus (Th1) |
| Multibacillary | Midborderline or Borderline ("BB") | A30.3 | Borderline | Borderline leprosy is of intermediate severity and is the most common form. Skin lesions resemble tuberculoid leprosy but are more numerous and irregular; large patches may affect a whole limb, and peripheral nerve involvement with weakness and loss of sensation is common. This type is unstable and may become lepromatous, or may undergo a reversal reaction, becoming more like the tuberculoid form. | ||
| Multibacillary | Borderline Lepromatous ("BL"), and Lepromatous ("LL") | A30.4, A30.5 | Lepromatous | It is associated with symmetric skin lesions, nodules, plaques, thickened dermis and frequent involvement of the nasal mucosa resulting in nasal congestion and epistaxis but detectable nerve damage is late. | Negative | Plasmid inside Bacillus (Th2) |
Ridley Jopling Classification
There are 6 classes in the Ridley Jopling classification scheme. This classification is based on the following:[4]
- Cutaneous elements
- Neurological elements
- Biopsy findings
- Immunological status
- Presence of acid-fast bacilli in dermis
Tuberculoid or Paucibacillary Pole
This is the least severe form of the disease. In this form of the disease the following are present:
- 1 to 3 well-defined lesions with central hypopigmented area and hypoesthesia
- Well-developed immune response
- Granulomatous inflammation
- Rare acid-fast bacilli
Skin
Ear
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
Trunk
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
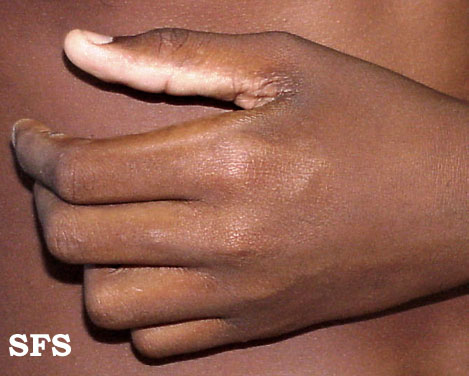
Extremity
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
Genitalia
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
Head
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
Gluteal Region
-
Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]
Nodular leprosy of childhood
Face
-
Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]
Trunk
-
Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]
-
Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]
Lepromatous or Multi-Bacillary Pole
In this form of the disease the following are present:
- Multiple undefined nodular lesions throughout the body
- Weak immune response
- Evidence of foamy macrophages in dermis filled with mycobacteria
- Patients are immunocompetent, despite not being able to fight mycobacterium leprae
Skin
Face
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
Trunk
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
Extremity
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
-
Lepromatous leprosy. Adapted from Dermatology Atlas.[5]
Ear
Image:Lepromatous leprosy09.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy18.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy23.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy27.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy28.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy35.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy36.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy40.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] Image:Lepromatous leprosy83.jpg|Lepromatous leprosy. Adapted from Dermatology Atlas.[5] </gallery>
Intermediate, Dimorphous or Borderline State
This last category is divided into 3 subcategories:
Borderline Tuberculoid, or BT
In this form of the disease the following are present:
- Progression towards the tuberculoid pole
- Increasing cell-mediated immunity
- Inflammation of the nerves and skin
Mid-Borderline, Borderline-Borderline, or BB
This is considered to be where the disease usually begins, progressing towards one of the poles afterwards.[1]
Borderline Lepromatous, or BL
In this form of the disease the following are present:
- Progression towards the lepromatous pole
- Common before treatment initiation
- Loss of cell-mediated immunity
Indeterminate
In this form of the disease the following are present:
- Early unspecific lesions
- Nerve infiltrates, lacking required criteria for being classified as above mentioned
- Used only when there is diagnostic proof of leprosy, from a biopsy sample, with evidence of mycobacterium leprae and perineural infiltrates but the disease is not advanced enough to show the clear patient position in the leprosy classification.
Skin
Extremity
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
Trunk
-
Indeterminate leprosr. Adapted from Dermatology Atlas.<ref name="Dermatology Atlas">{{Cite
WHO classification
The WHO organization classification scheme is simpler, and it is based upon the number of skin lesions. This simpler classification scheme can be applied in the absence of laboratory support or clinical expertise. It allows a rapid diagnosis, selection and initiation of treatment. The leprosy subtypes include:[6][4]
Paucibacillary or PB
- Higher level of immunity
- Lower number of bacilli
- Up to five skin lesions in total body examination
- Requires less intensive treatment
Multibacillary or MB
- Lower level of immunity
- Higher number of bacilli
- Six or more skin lesions in total body examination
- Requires intensive treatment
If a skin smear is done and shows a positive result, then that patient will immediately be classified as multibacillary, irrespective of the number of skin lesions identified on physical examination. Despite its ease of use, this classification scheme may unfortunately mis-classify some patients resulting in under treatment of those cases.
References
- ↑ 1.0 1.1 Walker, Stephen L.; Lockwood, Dina N.J. (2007). "Leprosy". Clinics in Dermatology. 25 (2): 165–172. doi:10.1016/j.clindermatol.2006.05.012. ISSN 0738-081X.
- ↑ Eichelmann, K.; González González, S.E.; Salas-Alanis, J.C.; Ocampo-Candiani, J. (2013). "Leprosy. An Update: Definition, Pathogenesis, Classification, Diagnosis, and Treatment". Actas Dermo-Sifiliográficas (English Edition). 104 (7): 554–563. doi:10.1016/j.adengl.2012.03.028. ISSN 1578-2190.
- ↑ Bhat, Ramesh Marne; Prakash, Chaitra (2012). "Leprosy: An Overview of Pathophysiology". Interdisciplinary Perspectives on Infectious Diseases. 2012: 1–6. doi:10.1155/2012/181089. ISSN 1687-708X.
- ↑ 4.0 4.1 Pardillo FE, Fajardo TT, Abalos RM, Scollard D, Gelber RH (2007). "Methods for the classification of leprosy for treatment purposes". Clin Infect Dis. 44 (8): 1096–9. doi:10.1086/512809. PMID 17366457.
- ↑ 5.000 5.001 5.002 5.003 5.004 5.005 5.006 5.007 5.008 5.009 5.010 5.011 5.012 5.013 5.014 5.015 5.016 5.017 5.018 5.019 5.020 5.021 5.022 5.023 5.024 5.025 5.026 5.027 5.028 5.029 5.030 5.031 5.032 5.033 5.034 5.035 5.036 5.037 5.038 5.039 5.040 5.041 5.042 5.043 5.044 5.045 5.046 5.047 5.048 5.049 5.050 5.051 5.052 5.053 5.054 5.055 5.056 5.057 5.058 5.059 5.060 5.061 5.062 5.063 5.064 5.065 5.066 5.067 5.068 5.069 5.070 5.071 5.072 5.073 5.074 5.075 5.076 5.077 5.078 5.079 5.080 5.081 5.082 5.083 5.084 5.085 5.086 5.087 5.088 5.089 5.090 5.091 5.092 5.093 5.094 5.095 5.096 5.097 5.098 5.099 5.100 5.101 5.102 5.103 5.104 5.105 5.106 5.107 5.108 5.109 5.110 5.111 5.112 5.113 5.114 5.115 5.116 5.117 5.118 5.119 5.120 5.121 5.122 5.123 5.124 5.125 5.126 5.127 5.128 5.129 5.130 5.131 5.132 5.133 5.134 5.135 5.136 5.137 5.138 5.139 5.140 5.141 5.142 5.143 5.144 5.145 5.146 5.147 5.148 5.149 5.150 5.151 5.152 5.153 5.154 5.155 5.156 5.157 5.158 5.159 5.160 5.161 5.162 5.163 5.164 5.165 5.166 5.167 5.168 5.169 5.170 5.171 5.172 5.173 5.174 5.175 5.176 5.177 5.178 5.179 5.180 5.181 5.182 5.183 "Dermatology Atlas".
- ↑ "Enhanced global strategy for further reducing the disease burden due to leprosy (2011-2015)" (PDF).
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b4/Tuberculoid_leprosy40.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/8/84/Tuberculoid_leprosy81.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/6/6c/Tuberculoid_leprosy06.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e6/Tuberculoid_leprosy17.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/cc/Tuberculoid_leprosy18.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/6/67/Tuberculoid_leprosy27.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/1/1d/Tuberculoid_leprosy36.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/38/Tuberculoid_leprosy41.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/ac/Tuberculoid_leprosy45.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/ca/Tuberculoid_leprosy49.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/6/60/Tuberculoid_leprosy50.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/ea/Tuberculoid_leprosy56.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/a1/Tuberculoid_leprosy57.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/51/Tuberculoid_leprosy58.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/4/49/Tuberculoid_leprosy62.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e8/Tuberculoid_leprosy63.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c2/Tuberculoid_leprosy64.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/a5/Tuberculoid_leprosy65.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0f/Tuberculoid_leprosy66.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f8/Tuberculoid_leprosy88.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/a5/Tuberculoid_leprosy01.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f6/Tuberculoid_leprosy02.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0a/Tuberculoid_leprosy03.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/24/Tuberculoid_leprosy04.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2f/Tuberculoid_leprosy07.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/39/Tuberculoid_leprosy08.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/0/03/Tuberculoid_leprosy10.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/d/db/Tuberculoid_leprosy11.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b9/Tuberculoid_leprosy12.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0c/Tuberculoid_leprosy13.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/0/08/Tuberculoid_leprosy14.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d6/Tuberculoid_leprosy16.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/ef/Tuberculoid_leprosy19.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c9/Tuberculoid_leprosy20.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f9/Tuberculoid_leprosy25.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/58/Tuberculoid_leprosy31.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e5/Tuberculoid_leprosy32.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/30/Tuberculoid_leprosy34.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/79/Tuberculoid_leprosy35.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/79/Tuberculoid_leprosy37.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/bc/Tuberculoid_leprosy38.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f4/Tuberculoid_leprosy39.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c0/Tuberculoid_leprosy42.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/6/65/Tuberculoid_leprosy43.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/8/89/Tuberculoid_leprosy44.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b6/Tuberculoid_leprosy51.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/22/Tuberculoid_leprosy52.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/33/Tuberculoid_leprosy53.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/9/9e/Tuberculoid_leprosy54.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2c/Tuberculoid_leprosy55.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/4/4a/Tuberculoid_leprosy67.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/a4/Tuberculoid_leprosy68.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c3/Tuberculoid_leprosy69.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b1/Tuberculoid_leprosy70.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/7e/Tuberculoid_leprosy71.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/5e/Tuberculoid_leprosy73.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e7/Tuberculoid_leprosy74.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/1/18/Tuberculoid_leprosy77.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/a/ad/Tuberculoid_leprosy78.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/4/4f/Tuberculoid_leprosy75.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2e/Tuberculoid_leprosy79.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/71/Tuberculoid_leprosy80.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/9/9e/Tuberculoid_leprosy82.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/39/Tuberculoid_leprosy83.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/7b/Tuberculoid_leprosy84.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/50/Tuberculoid_leprosy86.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/58/Tuberculoid_leprosy87.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/70/Tuberculoid_leprosy21.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b4/Tuberculoid_leprosy22.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/f/fe/Tuberculoid_leprosy23.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/4/4d/Tuberculoid_leprosy24.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/1/16/Tuberculoid_leprosy48.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/cf/Tuberculoid_leprosy47.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2e/Tuberculoid_leprosy59.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b6/Tuberculoid_leprosy60.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/4/45/Tuberculoid_leprosy61.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/7/72/Tuberculoid_leprosy28.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/3/30/Tuberculoid_leprosy29.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c2/Tuberculoid_leprosy30.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/2/20/Tuberculoid_leprosy33.jpg)
![Tuberculoid leprosy. Adapted from Dermatology Atlas.[5]](/images/5/59/Tuberculoid_leprosy05.jpg)
![Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]](/images/0/01/Nodular_leprosy_of_childhood01.jpg)
![Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]](/images/4/44/Nodular_leprosy_of_childhood02.jpg)
![Nodular leprosy of childhood. Adapted from Dermatology Atlas.[5]](/images/8/81/Nodular_leprosy_of_childhood03.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/99/Lepromatous_leprosy01.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f5/Lepromatous_leprosy02.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/ee/Lepromatous_leprosy11.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/eb/Lepromatous_leprosy12.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/2/29/Lepromatous_leprosy17.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/94/Lepromatous_leprosy22.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/06/Lepromatous_leprosy34.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/1/1d/Lepromatous_leprosy82.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0e/Lepromatous_leprosy85.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e2/Lepromatous_leprosy93.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b2/Lepromatous_leprosy94.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/4/4b/Lepromatous_leprosy95.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2b/Lepromatous_leprosy03.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/9c/Lepromatous_leprosy04.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b2/Lepromatous_leprosy05.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d6/Lepromatous_leprosy06.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/df/Lepromatous_leprosy07.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c6/Lepromatous_leprosy08.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f5/Lepromatous_leprosy14.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/7/79/Lepromatous_leprosy29.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/5d/Lepromatous_leprosy37.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/7/73/Lepromatous_leprosy38.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d9/Lepromatous_leprosy39.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/3/30/Lepromatous_leprosy41.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/8/87/Lepromatous_leprosy42.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/6/6d/Lepromatous_leprosy43.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/7/75/Lepromatous_leprosy44.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/db/Lepromatous_leprosy45.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/04/Lepromatous_leprosy47.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/3/38/Lepromatous_leprosy57.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/cc/Lepromatous_leprosy59.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2d/Lepromatous_leprosy60.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e1/Lepromatous_leprosy61.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/ed/Lepromatous_leprosy63.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/6/64/Lepromatous_leprosy64.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/1/11/Lepromatous_leprosy69.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e1/Lepromatous_leprosy70.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b7/Lepromatous_leprosy71.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/95/Lepromatous_leprosy77.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/3/3d/Lepromatous_leprosy78.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/ff/Lepromatous_leprosy86.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b3/Lepromatous_leprosy87.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c2/Lepromatous_leprosy88.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/55/Lepromatous_leprosy90.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d3/Lepromatous_leprosy89.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b6/Lepromatous_leprosy92.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/92/Lepromatous_leprosy96.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/9c/Lepromatous_leprosy97.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c4/Lepromatous_leprosy98.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/e7/Lepromatous_leprosy10.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d4/Lepromatous_leprosy13.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d2/Lepromatous_leprosy15.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/8/8b/Lepromatous_leprosy16.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/1/14/Lepromatous_leprosy19.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/5e/Lepromatous_leprosy20.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/9/98/Lepromatous_leprosy21.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/b1/Lepromatous_leprosy24.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/8/8f/Lepromatous_leprosy26.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2b/Lepromatous_leprosy30.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/d/d8/Lepromatous_leprosy31.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/a/ac/Lepromatous_leprosy32.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0b/Lepromatous_leprosy33.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/4/4f/Lepromatous_leprosy46.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/a/ac/Lepromatous_leprosy48.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/53/Lepromatous_leprosy49.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/50/Lepromatous_leprosy50.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/07/Lepromatous_leprosy51.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/51/Lepromatous_leprosy52.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/8/8b/Lepromatous_leprosy53.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/e/ea/Lepromatous_leprosy54.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/6/60/Lepromatous_leprosy55.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/0/0d/Lepromatous_leprosy56.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f5/Lepromatous_leprosy58.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/6/67/Lepromatous_leprosy62.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f9/Lepromatous_leprosy65.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/b/be/Lepromatous_leprosy66.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/3/3a/Lepromatous_leprosy67.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/7/7d/Lepromatous_leprosy68.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c0/Lepromatous_leprosy72.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/5e/Lepromatous_leprosy73.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/c/c7/Lepromatous_leprosy74.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/2/2d/Lepromatous_leprosy75.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/5e/Lepromatous_leprosy76.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/1/1f/Lepromatous_leprosy79.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/57/Lepromatous_leprosy80.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/5/54/Lepromatous_leprosy81.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/a/a0/Lepromatous_leprosy91.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/f/f3/Lepromatous_leprosy99.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/8/85/Lepromatous_leprosy100.jpg)
![Lepromatous leprosy. Adapted from Dermatology Atlas.[5]](/images/3/3f/Lepromatous_leprosy101.jpg)