Hepatic cysts diagnostic criteria
|
Hepatic cysts Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Hepatic cysts diagnostic criteria On the Web |
|
American Roentgen Ray Society Images of Hepatic cysts diagnostic criteria |
|
Risk calculators and risk factors for Hepatic cysts diagnostic criteria |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Diagnostic criteria
Bile Duct Hamartoma
The diagnosis of BDH pre-operatively is important. Lab tests typically do not yield any information. In general, patients are diagnosed by ultrasound, after which they receive abdominal CT .[1] Problematically, it is impossible to distinguish BDH from cystadenomas by CT scan, and cystadenomas can degenerate into carcinoma. Up to 10% of simple cysts evaluated by CT turn out to be cystadenomas on final pathology. [2] Therefore, depending on the type of surgery received, this may mean a lifetime of follow-up scans in surveillance of recurrence and cancer.
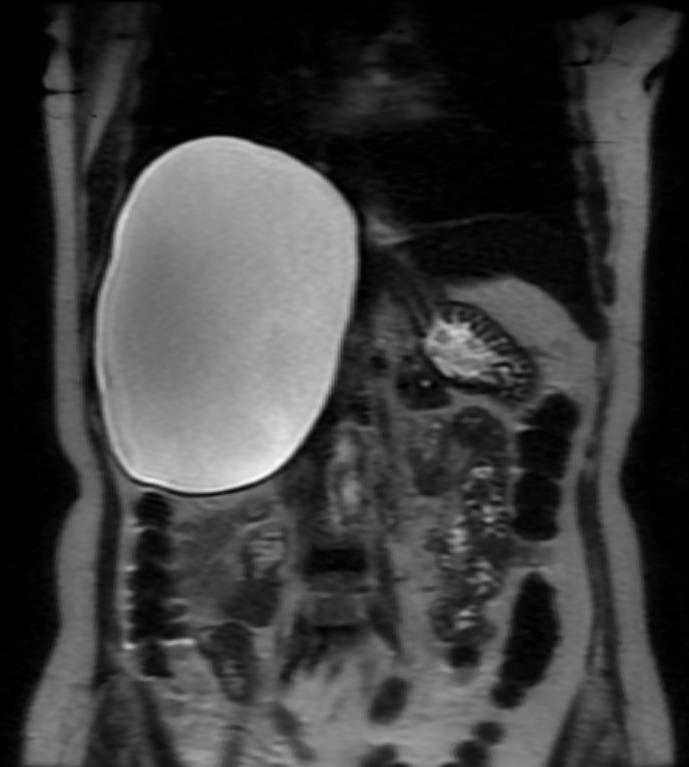
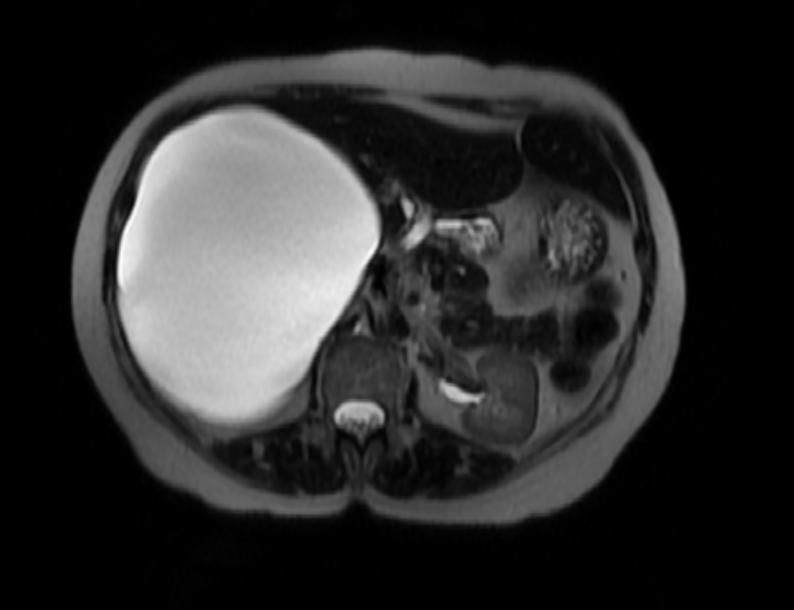
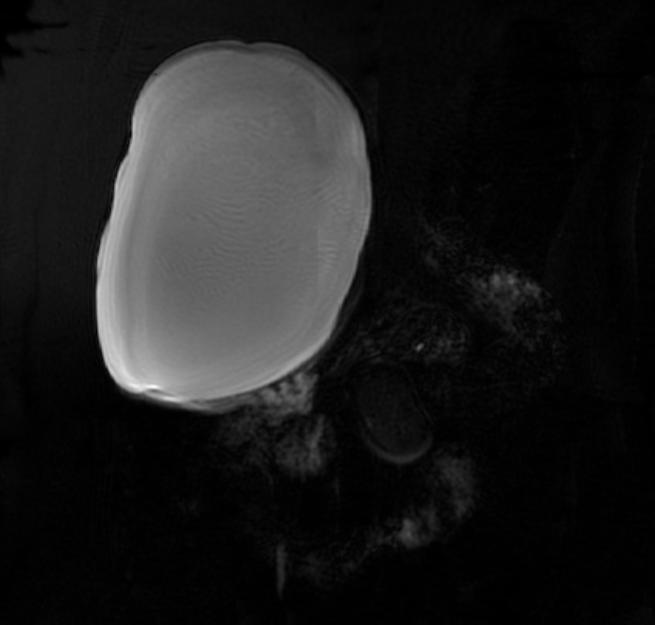
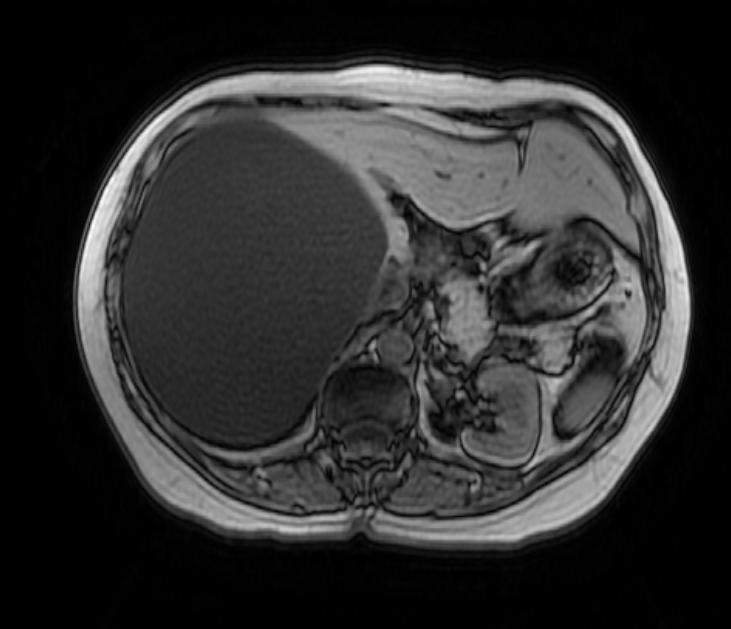
There is mounting evidence that MRI can be used to pre-operatively differentiates BDH from cystadenomas.[3][4][5][6] On MRI, BDH have well-defined, lobulated margins, thin septations, a thin rim of peripheral enhancement on T2 weighted images, internal fluid content that may contain hemorrhage and/or proteinaceaous material and are without any intracystic vascularized soft tissue elements.[7] By contrast, MRI evaluation of biliary cystadenomas and cystadenocarcinomas show smooth margins, mural nodules, and papillary projections without an enhancing peripheral rim.[8]
Cystadenoma and Cystadenocarcinomas
Radiologically, as above, MRI evaluation of biliary cystadenomas and cystadenocarcinomas show smooth margins, mural nodules, and papillary projections without an enhancing peripheral rim. On pathology, cystadenomas are generally lobulated, multiloculated, and contain clear to mucinous fluid of various colors. The internal lining is generally smooth, composed of a simple columnar or cuboidal glandular epithelium. The key feature that distinguishes the cystadenoma from the BDH is the presence of ovarian-type stroma.[9]>[10] Many, if not most, cystadenomas stain positively for estrogen, progesterone and alpha-inhibin receptors which offer a partially hormonal explanation for the predilection of these lesions for women.[11]
Hydatid Cysts
The diagnosis can usually be made by history and physical examination. Basic blood tests are largely unrevealing vis-à-vis liver enzyme profiles and blood counts (eosinophil counts are rarely elevated). Antibody titers (usually IgE) are useful in disseminated disease or tracking recurrence[12]. Indirect immunofluorence (IFA) is the most sensitive (95%), but can cross-react with cystercercosis. Older methods include an intradermal injection of hydatid antigens – the Casoni test – which is positive when a wheal develops. It is up to 90% sensitive in hepatic hydatitosis. The Weinberg test is a complement fixation test that is positive when greater than 1:4. [13]
The diagnosis is usually and reliably made by imaging. Plain film X-rays have an 11% sensitivity so it is advisable to use either ultrasound or CT, which both achieve a sensitivity and specificity of 97-100% and 100%.[14] The management of hydatid cysts is usually based on the imaging findings. The Gharbi classification is depicted below.
Gharbi’s Ultrasound Classification of Hepatic Hydatidosis
- Type 1: Pure fluid collection.
- Type 2: Fluid collection with a split wall.
- Type 3: Fluid collection with a daughter cyst.
- Type 4: Heterogeneous echo pattern.
- Type 5: Calcified wall
(Images courtesy of RadsWiki)
References
- ↑ Regev A et al. Large Cystic Lesions of the Liver in Adults:A 15-Year Experience in a Tertiary Center. J Am Coll Surg 2001;193:36–45
- ↑ Gamblin TC, Holloway SE, Heckman JT, Geller DA. Laparoscopic resection of benign hepatic cysts: a new standard. J Am Coll Surg. Nov 2008;207(5):731-736.
- ↑ Semelka RC, Hussain SM, Marcos HB, Woosley JT. Biliary hamartomas: solitary and multiple lesions shown on current MR techniques including gadolinium enhancement. J Magn Reson Imaging. 1999;10(2):196-201.
- ↑ Tohme-Noun C, Cazals D, Noun R, Menassa L, Valla D, Vilgrain V. Multiple biliary hamartomas: magnetic resonance features with histopathologic correlation. Eur Radiol. Mar 2008;18(3):493-499.
- ↑ Zheng RQ, Zhang B, Kudo M, Onda H, Inoue T. Imaging findings of biliary hamartomas. World J Gastroenterol 2005; 11:6354-6359.
- ↑ Tapper EB, Adsay NV, Kalb B, Martin D, Kooby D, Sarmiento JM. Symptomatic Bile Duct Hamartomas: Surgical Management in an MRI Driven Practice. Accepted by Journal of Gastrointestinal Surgery (Feb 2010)
- ↑ apper EB, Adsay NV, Kalb B, Martin D, Kooby D, Sarmiento JM. Symptomatic Bile Duct Hamartomas: Surgical Management in an MRI Driven Practice. J Gastrointest Surg. 2010 May 18. [Epub ahead of print]
- ↑ Lewin M, Mourra N, Honigman I, et al. Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol 2006;16(2):407-413
- ↑ Lam MM et al. Ovarian-Type Stroma in Hepatobiliary Cystadenomas and Pancreatic Mucinous Cystic Neoplasms. Am J Clin Pathol 2008;129:211-218
- ↑ Vogt et al. Cystadenoma and Cystadenocarcinoma of the Liver: A Single Center Experience. J AmColl Surg 2005;200:727–733
- ↑ Zamboni G, Scarpa A, Bogina G, et al. Mucinous cystic tumors of the pancreas: clinicopathological features, prognosis, and relationship to other mucinous cystic tumors. Am J SurgPathol. 1999;23:410-422.
- ↑ Force L et al.Evaluation of eight serological tests in the diagnosis of human echinococcosis and follow-up. Clin Infect Dis. 1992 Sep;15(3):473-80
- ↑ Biava MF et al. Laboratory Diagnosis of Cystic Hydatic Disease. World J. Surg 2001;25:10–14
- ↑ Balik AA et al. Surgical Treatment of Hydatid Disease of the Liver: Review of 304 Cases.Arch Surg. 1999;134:166-169