Gonorrhea Drug resistance
|
Gonorrhea Microchapters |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Gonorrhea Drug resistance On the Web |
|
American Roentgen Ray Society Images of Gonorrhea Drug resistance |
|
Risk calculators and risk factors for Gonorrhea Drug resistance |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Template:Saram
Overview
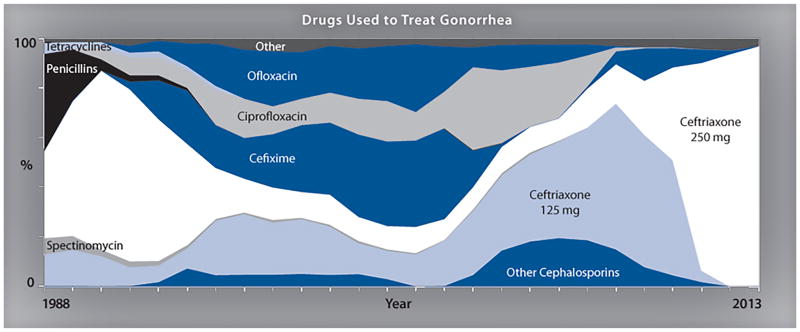
The mainstay of therapy for gonococcal infections is antimicrobial therapy. Gonorrhea treatment is complicated by the ability of N. gonorrhoeae to develop resistance to antimicrobials, therefore a combination therapy with Azithromycin and a Cephalosporin is used to improve treatment efficacy and potentially slow the emergence and spread of resistance.
Drug Resistance
- The mainstay of therapy for gonococcal infections is antimicrobial therapy.
- Gonorrhea treatment is complicated by the ability of Neisseria gonorrhoeae to develop resistance to antimicrobials, therefore a combination therapy with Azithromycin and a Cephalosporin is used to improve treatment efficacy and potentially slow the emergence and spread of resistance.
- High-level resistance to these expanded-spectrum cephalosporins is now reported, and it seems developing another effective treatment has become unaffordable.
- Although new combination antibiotic treatments are being evaluated. There are no affordable alternative therapeutic options currently available for the treatment of gonococcal disease. and it seems even newly developed antibiotics will be short solution and may be developed resistance as well.
The drug resistance may be developed by following mechanisms:
- Chromosomal mutations
- Acquisition of R factors (plasmids)
- In 1986, the CDC established the Gonococcal Isolate Surveillance Project (GISP)[1]
- Monitor antimicrobial susceptibility trends in the United States
- Characterize male patients with gonococcal infection
- Phenotypically characterize antimicrobial-resistant isolates of Niesseira gonorrhea

Penicillin
Penicillin has not been a first-line treatment option for gonorrhea for a number of decades. However, it has been tested for surveillance purposes.
- In 2012, Almost 13.1% of Niesseria gonorrhea from the GISP survey were resistant to penicillin mainly with two mechanisms:
- Chromosomal penicillin resistance (82.3%)
- Penicillinase production (17.7%)
Ceftriaxone
- In 1987, susceptibility testing for ceftriaxone began and continues to date.
- From 2008 to 2011, ceftriaxone Minimum inhibitory concentrations MICs increased from 0.1% to 0.4%.
- Five isolates with decreased ceftriaxone susceptibility (MIC 0.5 lg/ml) include:
- San Diego, California (1987)
- Cincinnati, Ohio (1992 and 1993)
- Philadelphia, Pennsylvania (1997)
- Oklahoma City, Oklahoma (2012)
- from 2006–2012, the prevalence of elevated Ceftriaxone (MICs) was higher in isolates from Men Who have Sex With Men (MSM) than from Men Who have Sex With women (MSW)
Cefixime
- In 1992, Cefixime susceptibility testing began and was discontinued in 2007
- In 2009, Cefixime susceptibility testing was restarted due to lack of drug supply in the United States
- From 2006 to 2010, ceftixim Minimum inhibitory concentrations (MICs) increased from 0.1 to 1.4
- from 2006–2012, the prevalence of elevated cefixime (MICs) was higher in isolates from Men Who have Sex With Men (MSM) than from Men Who have Sex With women (MSW)
References
- ↑ Schwarcz SK, Zenilman JM, Schnell D, et al. National surveillance of antimicrobial resistance in Neisseria gonorrhoeae. JAMA 1990;264:1413–7.