Failure to thrive physical examination
|
Failure to thrive Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Failure to thrive physical examination On the Web |
|
American Roentgen Ray Society Images of Failure to thrive physical examination |
|
Risk calculators and risk factors for Failure to thrive physical examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
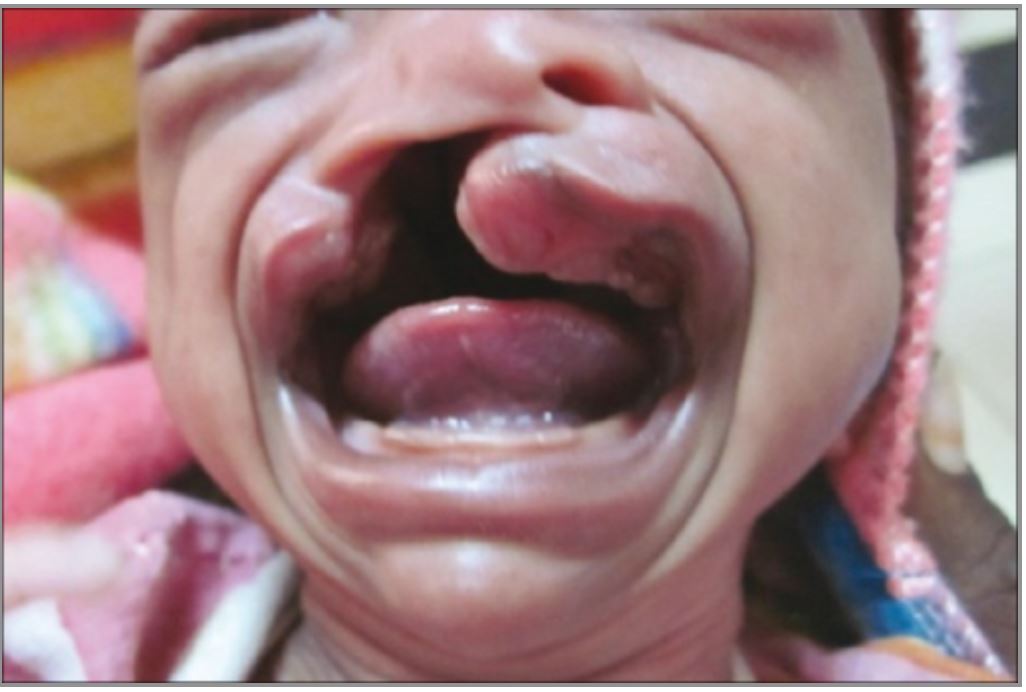
The patient encounter provides a good opportunity to not only physically examine the patient, but to also notice the interaction between the parents and the child. Murmurs, structural deformities such as cleft lip or palate, crackles secondary to a cystic fibrosis related pneumonia or rashes secondary to physical abuse are some important positive findings. With proper technique, anthropometric measurements should be plotted and compared with previous measurements.
Physical Examination
Appearance of the Patient[1][2]
- The patient encounter is a very good opportunity to notice the child, the parents, and the interaction between the two.
- Look for signs of physical abuse or neglect in the child; frightened, apathetic, withdrawn, minimal smiling with a lowered eye gaze. A poorly fed child would have a dysmorphic body habitus and may even be dehydrated.
- Mental status changes in a child can indicate poor bonding or cerebral palsy.
- Some studies have said that such children may present in a state of tonic immobility; with elbows flexed, humerus abducted and rotated outward with hands pronated.
- The parents should also be assessed in terms of their willingness to give details, their ability to calm the child down, recognize the child’s cues and their general demeanor. Parents may even be asked to feed the child, especially at a time when the child is hungry.
- Indices to be measured:
- Weight for height
- Weight for age
- Height for age
- Head circumference
- These indices should be compared with the measurements made on the previous visits on a growth chart.
-
Non accidental trauma
-
Non accidental trauma
-
Non accidental trauma
-
Severe acute malnutrition : Edematous and Non-edematous malnutrition
-
Cleft lip and cleft palate
-
Rickets
-
Microcephaly - Smith-Lemli-Opitz-syndrome
-
Hypertelorism- Smith-Lemli-Opitz-syndrome
Vital Signs
- High- fever – recurrent gastrointestinal/respiratory/skin infections, immunodeficiency syndromes
- Hypothermia/ hyperthermia may be present
- Tachycardia with regular pulse or irregularly irregular pulse – cyanotic heart disease
- Bradycardia with regular pulse or irregularly irregular pulse – congenital heart disease, part of Cushing’s triad in individuals with increased intracranial pressure.
- Tachypnea / bradypnea – Cystic fibrosis
Skin
- Pallor – iron deficiency anemia is the most common complication in failure to thrive
- Icterus – biliary atresia
- Cyanosis – congenital heart disease
- Clubbing – cyanotic heart disease
- Rashes, signs of abuse such as bruises – child abuse
- Stomatitis, cheilosis, acrodermatitis enterohepatica – vitamin deficiency
HEENT
- * Evidence of trauma – posterior rib fractures, battle sign, retinal hemorrhages
- Icteric sclera
- Ophthalmoscopic exam may be abnormal with findings of corneal xerosis and bitot’s spots indicative of vitamin A deficiency
- Hearing acuity may be reduced
- Weber test may be abnormal (Note: A positive Weber test is considered a normal finding / A negative Weber test is considered an abnormal finding. To avoid confusion, you may write "abnormal Weber test".) – often cystic fibrosis patients develop sensorineural hearing loss due to macrolide consumption
- Rinne test may be positive (Note: A positive Rinne test is considered a normal finding / A negative Rinne test is considered an abnormal finding. To avoid confusion, you may write "abnormal Rinne test".) - often cystic fibrosis patients develop sensorineural hearing loss due to macrolide consumption
- Exudate from the ear canal – recurrent middle ear infections due to immunodeficiency syndromes
- Purulent exudate from the nares - recurrent middle ear infections due to immunodeficiency syndromes
- Erythematous throat with/without tonsillar swelling, exudates, and/or petechiae
Neck
- Jugular venous distension – congenital heart disease
- Lymphadenopathy – secondary to infection or underlying malignancy.
- Thyromegaly / thyroid nodules – hyperthyroidism
- Hepatojugular reflux
Lungs
- Asymmetric chest expansion
- Lungs are hyporesonant – nephrogenic or cardiogenic pulmonary edema
- Fine/coarse crackles upon auscultation of the lung bases/apices unilaterally/bilaterally – recurrent pneumonia secondary to cystic fibrosis
- Rhonchi
Heart
- Displaced point of maximal impulse (PMI) suggestive of cardiomegaly
- Heave / thrill – underlying valvular or congenital heart disease
- Friction rub - underlying valvular or congenital heart disease.
- S1
- S2 – S2 with a fixed split and a diastolic murmur heard over the tricuspid area is indicative of an atrial septal defect.
- S3 – volume overload.
- S4
- Gallops
- A high/low grade early/late systolic murmur / diastolic murmur best heard at the base/apex/(specific valve region) may be heard using the bell/diaphgram of the stethoscope – pansystolic murmur seen in ventricular septal defect, Tetralogy of Fallot.
Abdomen
- Abdominal distension – distended, tympanic abdomen with hyperactive bowel sounds. Secondary to small intestinal bowel obstruction
- Rebound tenderness – peritonitis
- A palpable abdominal mass in the right/left upper/lower abdominal quadrant – malignancy, inflammatory bowel disease
- Guarding may be present
- Hepatomegaly / splenomegaly / hepatosplenomegaly
Back
- Back examination of patients with [disease name] is usually normal.
Genitourinary
- Genitourinary examination of patients with [disease name] is usually normal.
Neuromuscular
- Patient is usually oriented to persons, place, and time
- Altered mental status
- Glasgow coma scale is ___ / 15 – patient may present with altered mental status secondary to an underlying space occupying lesion, uremic or hepatic encephalopathy.
- Clonus may be present
- Hyperreflexia / hyporeflexia / areflexia – cerebral palsy
- Positive (abnormal) Babinski / plantar reflex unilaterally/bilaterally
- Muscle rigidity -cerebral palsy
- Proximal/distal muscle weakness unilaterally/bilaterally
Extremities
- Cyanosis – congenital heart disease
- Clubbing – cyanotic heart disease
- Pitting/non-pitting edema of the upper/lower extremities – heart failure
- Muscle atrophy along with reduced subcutaneous fat
References
- ↑ Nangia S, Tiwari S (2013). "Failure to thrive". Indian J Pediatr. 80 (7): 585–9. doi:10.1007/s12098-013-1003-1. PMID 23604606.
- ↑ Goldbloom RB (1982). "Failure to thrive". Pediatr Clin North Am. 29 (1): 151–66. doi:10.1016/s0031-3955(16)34114-1. PMID 6276853.