Coronary circulation
|
Coronary Angiography | |
|
General Principles | |
|---|---|
|
Anatomy & Projection Angles | |
|
Normal Anatomy | |
|
Anatomic Variants | |
|
Projection Angles | |
|
Epicardial Flow & Myocardial Perfusion | |
|
Epicardial Flow | |
|
Myocardial Perfusion | |
|
Lesion Complexity | |
|
ACC/AHA Lesion-Specific Classification of the Primary Target Stenosis | |
|
Lesion Morphology | |
Template:Infobox Anatomy Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Rim Halaby, M.D. [3]
Overview
The coronary circulation is the circulation of blood in the blood vessels that supply blood to and from the heart muscle itself. Although blood fills the chambers of the heart, the muscle tissue of the heart, the myocardium, is so thick that it requires coronary blood vessels to deliver blood deep into it. The coronary arteries are the vessels that deliver oxygen-rich blood to the myocardium. Cardiac veins are the vessels that remove the deoxygenated blood from the heart muscle. Epicardial coronary arteries are the coronary arteries that run on the surface of the heart. These arteries, when healthy, are capable of autoregulation to maintain coronary blood flow at levels appropriate to the needs of the heart muscle. These relatively narrow vessels are commonly affected by atherosclerosis and can become blocked, causing angina or a heart attack. Subendocardial coronary arteries run deep within the myocardium. The coronary arteries are classified as end circulation, since they represent the only source of blood supply to the myocardium: there is very little redundant blood supply, which is why blockage of these vessels can be so critical.
Coronary Arteries and Veins
Coronary Arteries
he coronary arteries supply oxygenated blood to the heart muscle itself. Although blood fills the chambers of the heart, the muscle tissue of the heart, or myocardium, is so thick that it requires coronary blood vessels to deliver blood deep into it. There are two primary arteries supplying the heart, the left coronary artery and the right coronary artery. These two epicardial coronary arteries course along the surface of the heart and this is why they are called "epicardial" (on top of the heart) arteries. Smaller arteries dive deep into the heart muscle and are called subendocardial coronary arteries.
Click here for details about coronary arteries.
Cardiac Veins
The cardiac veins are the vessels that remove the deoxygenated blood from the heart muscle and return it to the right atrium.
Click here for details about cardiac veins.
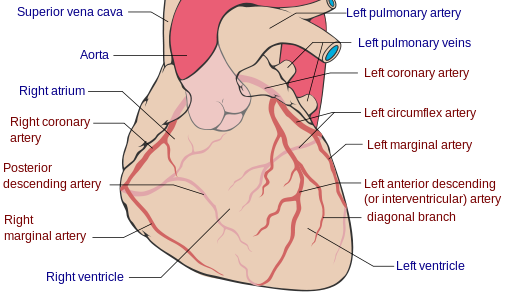
Shown below is an image depicting the coronary arteries and cardiac veins.
Blood Supply to the Papillary Muscles
- The papillary muscles tether the mitral valve (the valve between the left atrium and the left ventricle) and the tricuspid valve (the valve between the right atrium and the right ventricle) to the wall of the heart.
- If the papillary muscles are not functioning properly, the mitral valve leaks during contraction of the left ventricle and causes some of the blood to travel "in reverse", from the left ventricle to the left atrium, instead of forward to the aorta and the rest of the body.
- This leaking of blood to the left atrium is known as mitral regurgitation.
- The anterolateral papillary muscle:
- It receives two blood supplies: the LAD and LCX.
- It is therefore somewhat resistant to coronary ischemia (insufficiency of oxygen-rich blood).
- The posteromedial papillary muscle:
- It is supplied only by the PDA.
- This makes the posteromedial papillary muscle significantly more susceptible to ischemia.
- The clinical significance of the nature of blood supply to the papillary muscles is that a myocardial infarction involving the PDA is more likely to cause mitral regurgitation.
Coronary flow
- During contraction of the ventricular myocardium (systole), the subendocardial coronary vessels (the vessels that enter the myocardium) are compressed due to the high intraventricular pressures. However the epicardial coronary vessels (the vessels that run along the outer surface of the heart) remain patent. Because of this, blood flow in the subendocardium stops.
- As a result most myocardial perfusion occurs during heart relaxation (diastole) when the subendocardial coronary vessels are patent and under low pressure. This contributes to the filling difficulties of the coronary arteries.
- Failure of oxygen delivery via increases in blood flow to meet the increased oxygen demand of the heart results in tissue ischemia, a condition of oxygen debt.
- Brief ischemia is associated with intense chest pain, known as angina.
- Severe ischemia can cause the heart muscle to die of oxygen starvation, called a myocardial infarction.
- Chronic moderate ischemia causes contraction of the heart to weaken, known as myocardial hibernation.
- In addition to metabolism, the coronary circulation possesses unique pharmacologic characteristics. Prominent among these is its reactivity to adrenergic stimulation. The majority of vasculature in the body constricts to norepinephrine, a sympathetic neurotransmitter the body uses to increase blood pressure.
- In the coronary circulation, norepinephrine elicits vasodilation, due to the predominance of beta-adrenergic receptors in the coronary circulation.
- Agonists of alpha-receptors, such as phenylephrine, elicit very little constriction in the coronary circulation.