Cleft lip and palate surgery
|
Cleft lip and palate Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Cleft lip and palate surgery On the Web |
|
American Roentgen Ray Society Images of Cleft lip and palate surgery |
|
Risk calculators and risk factors for Cleft lip and palate surgery |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Cleft lip and palate is very treatable, however the kind of treatment depends on the type and severity of the cleft. Most children with a form of clefting are monitored by a cleft palate team or craniofacial team through young adulthood. Care can be lifelong. Treatment procedures can vary between craniofacial teams. For example, some teams wait on jaw correction until the child is aged 10 to 12 (argument: growth is less influential as deciduous teeth are replaced by permanent teeth, thus saving the child from repeated corrective surgeries), while other teams correct the jaw earlier (argument: less speech therapy is needed than at a later age when speech therapy becomes harder). Within teams, treatment can differ between individual cases depending on the type and severity of the cleft.
Cleft lip Surgery
Within the first 2-3 months after birth, surgery is performed to close the cleft lip. While surgery to repair a cleft lip can be performed soon after birth, the often preferred age is at approximately 10 weeks of age, following the "rule of 10s" coined by surgeons Wilhelmmesen and Musgrave in 1969 (the child is at least 10 weeks of age; weighs at least 10 pounds, and has at least 10 g haemoglobin). If the cleft is bilateral and extensive, two surgeries may be required to close the cleft, one side first, and the second side a few weeks later. The most common procedure to repair a cleft lip is the Millard procedure pioneered by Ralph Millard.
Often an incomplete cleft lip requires the same surgery as complete cleft. This is done for two reasons. Firstly the group of muscles required to purse the lips run through the upper lip. In order to restore the complete group a full incision must be made. Secondly, to create a less obvious scar the surgeon tries to line up the scar with the natural lines in the upper lip (such as the edges of the philtrum) and tuck away stitches as far up the nose as possible. Incomplete cleft gives the surgeon more tissue to work with, creating a more supple and natural-looking upper lip.
D. Ralph Millard pioneered the technique of rotation-advancement procedure for cleft lip repair, performing the first procedure at a Mobile Army Surgical Hospital unit in Korea.[1] This technique is the standard used to repair unilateral cleft lip all over the world.
Cleft palate Surgery
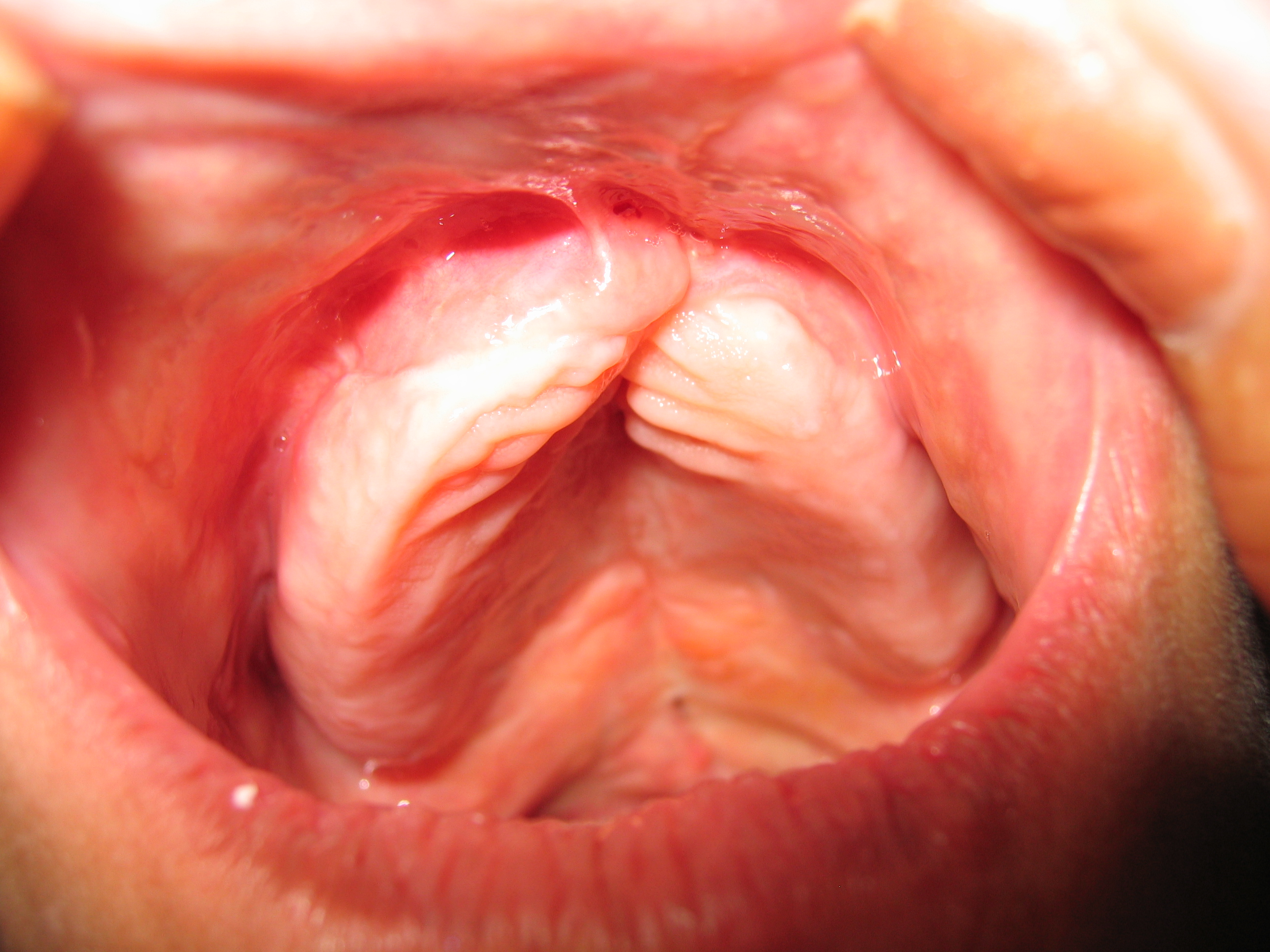
Often a cleft palate is temporarily closed using a palatal obturator. The obturator is a prosthetic device made to fit the roof of the mouth covering the gap.
Cleft palate can also be corrected by surgery, usually performed between 9 and 18 months. Approximately 20-25% only require one palatal surgery to achieve a competent velopharyngeal valve capable of producing normal, non-hypernasal speech. However, combinations of surgical methods and repeated surgeries are often necessary as the child grows. One of the new innovations of cleft lip and cleft palate repair is the Latham appliance. The Latham is surgically inserted by use of pins during the child's 4th or 5th month. After it is in place, the doctor, or parents, turn a screw daily to bring the cleft together to assist with future lip and/or palate repair.
If the cleft extends into the maxillary alveolar ridge, the gap is usually corrected by filling the gap with bone tissue. The bone tissue can be acquired from the patients own chin, rib or hip.
Speech and hearing treatments
A tympanostomy tube is often inserted into the eardrum to aerate the middle ear. This is often beneficial for the hearing ability of the child. Speech problems are usually treated by a speech-language pathologist. In some cases pharyngeal flap surgery is performed to regulate the airflow during speech and reduce nasal sounds.
Sample treatment schedule
Note that each individual patient's schedule is treated on a case-by-case basis and can vary per hospital. The table below shows a common sample treatment schedule. The colored squares indicate the average timeframe in which the indicated procedure occurs. In some cases this is usually one procedure (for example lip repair) in other cases this it is an ongoing therapy (for example speech therapy).
age |
||||||||||||||||||||||
| Palatal obturator | ||||||||||||||||||||||
| Repair cleft lip | ||||||||||||||||||||||
| Repair soft palate | ||||||||||||||||||||||
| Repair hard palate | ||||||||||||||||||||||
| Tympanostomy tube | ||||||||||||||||||||||
| Speech therapy/Pharyngeal surgery | ||||||||||||||||||||||
| Bone grafting jaw | ||||||||||||||||||||||
| Orthodontics | ||||||||||||||||||||||
| Further cosmetic corrections |
Craniofacial team
A craniofacial team is routinely used to treat this condition. The majority of hospitals still use craniofacial teams; yet others are making a shift towards dedicated cleft lip and palate programs. While craniofacial teams are widely knowledgeable about all aspects of craniofacial conditions, dedicated cleft lip and palate teams are able to dedicate many of their efforts to being on the cutting edge of new advances in cleft lip and palate care.
Many of the top pediatric hospitals are developing their own CLP clinics in order to provide patients with comprehensive multi-disciplinary care from birth through adolescence. Allowing an entire team to care for a child throughout their cleft lip and palate treatment (which is ongoing) allows for the best outcomes in every aspect of a child's care. While the individual approach can yield significant results, current trends indicate that team based care leads to better outcomes for CLP patients. .[2]
References
- ↑ "Biography and Personal Archive". Retrieved 2007-07-01. at miami.edu
- ↑ Joanne Green. "The Importance of a Multi-Disciplinary Approach". Retrieved 2007-10-15.