Capillary leak syndrome natural history, complications and prognosis
|
Capillary leak syndrome Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Capillary leak syndrome natural history, complications and prognosis On the Web |
|
American Roentgen Ray Society Images of Capillary leak syndrome natural history, complications and prognosis |
|
FDA on Capillary leak syndrome natural history, complications and prognosis |
|
CDC on Capillary leak syndrome natural history, complications and prognosis |
|
Capillary leak syndrome natural history, complications and prognosis in the news |
|
Blogs on Capillary leak syndrome natural history, complications and prognosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: M. Hassan, M.B.B.S
Overview
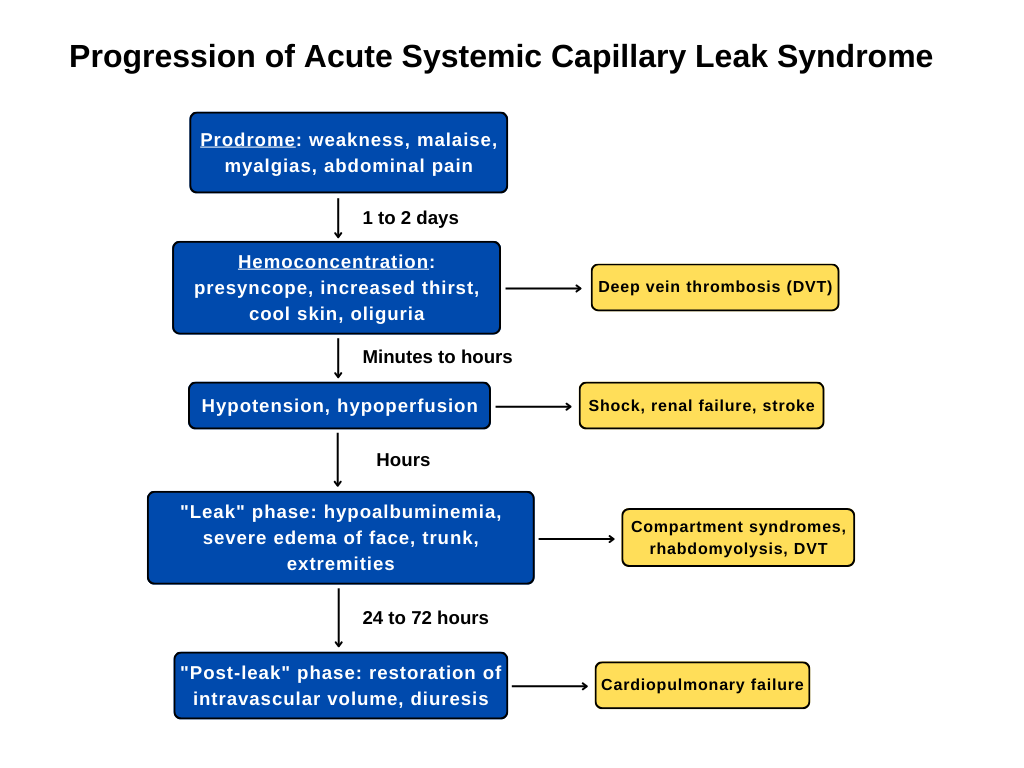
Capillary leak syndrome may present as an acute or chronic phase. The acute phase can be further subdivided into the capillary leak phase and the recruitment of interstitial fluid.
Capillary leak syndrome is associated with the following complications Compartment syndrome, Pulmonary edema, end-organ damage leading to multiorgan failure, Arrhythmias, Pericardial effusion, Myocardial edema, Pancreatitis, acute deep venous thrombosis, acute renal failure, Rhabdomyolysis, Pleural effusion, and acute ischemic stroke.
Mortality is reported in 21% of the 57 cases described. However, better management of this condition has recently led to lower mortality. Prognosis can be determined according to the SCLS Severity Scale which describes the condition according to grades.
Natural History
Capillary leak syndrome may present as an acute or chronic phase. The acute phase is further subdivided into the Capillary Leak Phase and Recruitment of the Interstitial Fluid.[1]
Acute:
The Capillary Leak Phase (1-4 days)
The initial phase is the capillary leak phase, lasting from 1 to 4 days. Clinical features are abdominal pain, nausea, generalized edema and hypotension that may result in cardiopulmonary collapse. Acute renal failure is due to acute tubular necrosis consequent to hypovolemia and rhabdomyolysis.
Recruitment of the Interstitial Fluid
The second phase results in the recruitment of the initially extravasated fluid. Intravascular overload with polyuria and pulmonary edema often occur. Edema may be more severe due to massive fluid supply in the initial phase. It's necessary to monitor the patient in order to switch to depletion treatment with diuretics or hemofiltration.
Chronic:
The chronic subtype poses difficulty when diagnosing cases. Affected individuals often develop persistent but irregular generalized edema that progresses over time. Pleural and pericardial effusion may also be evident.[2]
Complications
Most common complications of capillary leak syndrome include the following:[4][5]
| Complications of Capillary Leak Syndrome |
|---|
|
Prognosis
Mortality is reported in 21% of the 57 cases described. However, better management of this condition has recently led to lower mortality. Prognosis can be determined according to the SCLS Severity Scale which describes the condition according to grades.[3]
| Grade | Prognosis | Treatment | Hemoconcentration | Hypoalbuminemia |
|---|---|---|---|---|
| 1a | Good | Oral fluids | Hgb ≤ 3 g/dL | Albumin ≤ 0.5 g/dL |
| 1b | Good | Oral fluids | Hgb ≥ 3 g/dL | Albumin ≥ 0.5 g/dL |
| 2 | Variable | IV fluids, no hospitalization | ||
| 3 | Poor | IV fluids, ICU | ||
| 4 | Fatal | ICU |
In the Mayo Clinic’s experience, the median survival of 25 patients that were followed over 30 years (counting only SCLS-related deaths) was approximately 15 years, and their 5-year survival rate was 76%. In European experience, the 5-year post-diagnosis survival rate was 85% in 23 patients who had received prophylactic treatment and 20% in 5 patients who had not. However, better identification and management of this condition appears to be resulting in lower mortality and improving survival and quality-of-life results as of late.[6]
References
- ↑ Druey KM, Greipp PR (2010). "Narrative review: the systemic capillary leak syndrome". Ann Intern Med. 153 (2): 90–8. doi:10.7326/0003-4819-153-2-201007200-00005. PMC 3017349. PMID 20643990.
- ↑ Druey KM, Greipp PR (2010). "Narrative review: the systemic capillary leak syndrome". Ann Intern Med. 153 (2): 90–8. doi:10.7326/0003-4819-153-2-201007200-00005. PMC 3017349. PMID 20643990.
- ↑ 3.0 3.1 Druey KM, Greipp PR (2010). "Narrative review: the systemic capillary leak syndrome". Ann Intern Med. 153 (2): 90–8. doi:10.7326/0003-4819-153-2-201007200-00005. PMC 3017349. PMID 20643990.
- ↑ Hajare KR, Patil P, Bansode J (2018). "Idiopathic Systemic Capillary Leak Syndrome". Indian J Crit Care Med. 22 (5): 369–371. doi:10.4103/ijccm.IJCCM_464_17. PMC 5971649. PMID 29910550.
- ↑ Kapoor P, Greipp PT, Schaefer EW, Mandrekar SJ, Kamal AH, Gonzalez-Paz NC; et al. (2010). "Idiopathic systemic capillary leak syndrome (Clarkson's disease): the Mayo clinic experience". Mayo Clin Proc. 85 (10): 905–12. doi:10.4065/mcp.2010.0159. PMC 2947962. PMID 20634497.
- ↑ Druey KM, Greipp PR (2010). "Narrative review: the systemic capillary leak syndrome". Ann Intern Med. 153 (2): 90–8. doi:10.7326/0003-4819-153-2-201007200-00005. PMC 3017349. PMID 20643990.