Blood type
|
WikiDoc Resources for Blood type |
|
Articles |
|---|
|
Most recent articles on Blood type |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Blood type at Clinical Trials.gov Clinical Trials on Blood type at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Blood type
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Blood type Discussion groups on Blood type Patient Handouts on Blood type Directions to Hospitals Treating Blood type Risk calculators and risk factors for Blood type
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Blood type |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
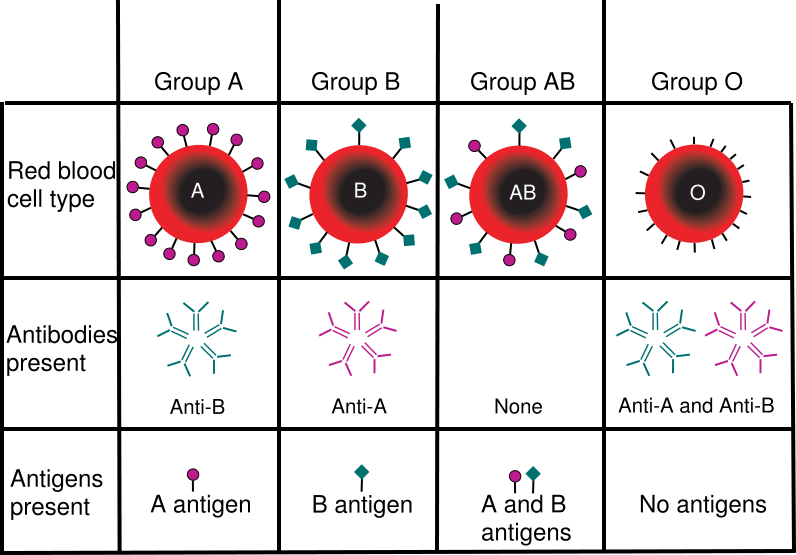
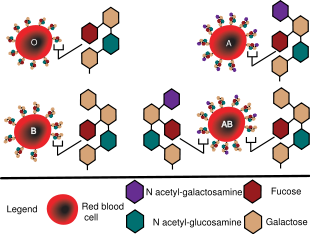
A blood type (also called a blood group) is a classification of blood based on the presence or absence of inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins or glycolipids, depending on the blood group system, and some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens, that stem from one allele (or very closely linked genes), collectively form a blood group system.
Immunological effects of mismatched blood transfusions are much more likely to involve components of the ABO blood group system or the RhD antigen (also known as the Rhesus factor or Rhesus D antigen) of the Rhesus blood group system than components of any of the other blood group systems; hence, in the routine preparation of blood for transfusion in a blood bank, the presence or absence the immunogenic blood group antigens, the A antigen, the B antigen and the RhD antigen are always determined for all recipient and donor blood. This identifies the ABO blood group and the RhD antigen status, which are both stated in the common terminology A positive, O negative, etc., where a capital letter (A, B or O) refers to the ABO blood group, and positive or negative refers to the presence or absence of the RhD antigen of the Rhesus blood group system. In the routine preparation and selection of donor blood for blood transfusion, it is not necessary to determine the status of any other blood group antigens or antibodies, because antibody screening and cross-matching (or computer aided simulated cross-matching) prior to transfusion detects if there are any other blood group incompatibilities between potential donor blood and intended recipients.
If an individual is exposed to a blood group antigen that is not recognised as self, the immune system will produce antibodies that can specifically bind to that particular blood group antigen and an immunological memory against that antigen is formed. The individual will have become sensitized to that blood group antigen. These antibodies can bind to antigens on the surface of transfused red blood cells (or other tissue cells) often leading to destruction of the cells by recruitment of other components of the immune system. When IgM antibodies bind to the transfused cells, the transfused cells can clump. It is vital that compatible blood is selected for transfusions and that compatible tissue is selected for organ transplantation. Transfusion reactions involving minor antigens or weak antibodies may lead to minor problems. However, more serious incompatibilities can lead to a more vigorous immune response with massive RBC destruction, low blood pressure, and even death.
Blood types are inherited and represent contributions from both parents. Often, pregnant women carry a fetus with a different blood type from their own, and sometimes the mother forms antibodies against the red blood cells of the fetus, which causes hemolysis of fetal RBCs, and which in turn can lead to low fetal blood counts, a condition known as hemolytic disease of the newborn. Some blood types are associated with inheritance of other diseases; for example, the Kell antigen is associated with McLeod syndrome.[1] Certain blood types may affect susceptibility to infections, an example being the resistance to specific malaria species seen in individuals lacking the Duffy antigen.[2] The Duffy antigen, presumedly as a result of natural selection, is less common in ethnic groups from areas with a high incidence of malaria.[3]
The two most significant blood group systems were discovered during early experiments with blood transfusion: the ABO group in 1901[4] and the Rhesus group in 1937.[5] Development of the Coombs test in 1945,[6] the advent of transfusion medicine, and the understanding of hemolytic disease of the newborn led to discovery of more blood groups. Today, a total of 29 human blood group systems are recognized by the International Society of Blood Transfusion (ISBT).[7] A complete blood type would describe a full set of 29 substances on the surface of RBCs, and an individual's blood type is one of the many possible combinations of blood group antigens. Across the 29 blood groups, over 600 different blood group antigens have been found,[8] but many of these are very rare or are mainly found in certain ethnic groups. Almost always, an individual has the same blood group for life; but very rarely, an individual's blood type changes through addition or suppression of an antigen in infection, malignancy or autoimmune disease.[9] Blood types have been used in forensic science and in paternity testing, but both of these uses are being replaced by DNA analysis, which provides greater certitude.
Blood group systems
ABO blood group system
The ABO system is the most important blood group system in human blood transfusion. The associated anti-A antibodies and anti-B antibodies are usually "Immunoglobulin M", abbreviated IgM, antibodies. ABO IgM antibodies are produced in the first years of life by sensitization to environmental substances such as food, bacteria and viruses. The "O" in ABO is often called "0" (zero/null) in other languages.[10]
| Phenotype | Genotype |
|---|---|
| A | AA or AO |
| B | BB or BO |
| AB | AB |
| O | OO |
Rhesus blood group system
The Rhesus system is the second most significant blood group system in human blood transfusion. The most significant Rhesus antigen is the RhD antigen because it is the most immunogenic of the five main rhesus antigens. It is common for RhD negative individuals not to have any anti-RhD IgG or IgM antibodies, because anti-RhD antibodies are not usually produced by sensitization against environmental substances. However, RhD negative individuals can produce IgG anti-RhD antibodies following a sensitizing event: possibly a fetomaternal transfusion of blood from a fetus in pregnancy or occasionally a blood transfusion with RhD positive RBCs.
ABO and Rh distribution by nation
| Country | O+ | A+ | B+ | AB+ | O− | A− | B− | AB− |
|---|---|---|---|---|---|---|---|---|
| Argentina[11] | 53.8% | 34.7% | 8.8% | 2.7% | 8.4% | 0.44% | 0.21% | 0.06% |
| Austria[12] | 30% | 33% | 12% | 6% | 7% | 8% | 3% | 1% |
| Australia[13] | 40% | 31% | 8% | 2% | 9% | 7% | 2% | 1% |
| Belgium | 38.1% | 34% | 8.5% | 4.1% | 7% | 6% | 1.5% | 0.8% |
| Canada[14] | 39% | 36% | 7.6% | 2.5% | 7% | 7% | 1.4% | 0.5% |
| Denmark[15] | 35% | 37% | 8% | 4% | 6% | 7% | 2% | 1% |
| Finland[16] | 27% | 38% | 15% | 7% | 4% | 6% | 2% | 1% |
| France[17] | 36% | 37% | 9% | 3% | 6% | 7% | 1% | 1% |
| Germany | 35% | 37% | 9% | 4% | 6% | 6% | 2% | 1% |
| Hong Kong, China[18] | 40% | 26% | 27% | 7% | <0.3% | <0.3% | <0.3% | <0.3% |
| Korea, South[19] | 27.4% | 34.4% | 26.8% | 11.2% | 0.1% | 0.1% | 0.1% | 0.05% |
| Netherlands[20] | 39.5% | 35% | 6.7% | 2.5% | 7.5% | 7% | 1.3% | 0.5% |
| Poland[21] | 31% | 32% | 15% | 7% | 6% | 6% | 2% | 1% |
| Sweden[22] | 32% | 37% | 10% | 5% | 6% | 7% | 2% | 1% |
| UK[23] | 37% | 35% | 8% | 3% | 7% | 7% | 2% | 1% |
| USA[24] | 38% | 34% | 9% | 3% | 7% | 6% | 2% | 1% |
Other blood group systems
The International Society of Blood Transfusion currently recognizes 29 blood group systems (including the ABO and Rh systems).[7] Thus, in addition to the ABO antigens and Rhesus antigens, many other antigens are expressed on the RBC surface membrane. For example, an individual can be AB RhD positive, and at the same time M and N positive (MNS system), K positive (Kell system), Lea or Leb negative (Lewis system), and so on, being positive or negative for each blood group system antigen. Many of the blood group systems were named after the patients in whom the corresponding antibodies were initially encountered.
Clinical significance
Blood transfusion
Transfusion medicine is a specialized branch of hematology that is concerned with the study of blood groups, along with the work of a blood bank to provide a transfusion service for blood and other blood products. Across the world, blood products must be prescribed by a medical doctor (licensed physician or surgeon) in a similar way as medicines. In the USA, blood products are tightly regulated by the Food and Drug Administration.
Much of the routine work of a blood bank involves testing blood from both donors and recipients to ensure that every individual recipient is given blood that is compatible and is as safe as possible. If a unit of incompatible blood is transfused between a donor and recipient, a severe acute immunological reaction, hemolysis (RBC destruction), renal failure and shock are likely to occur, and death is a possibility. Antibodies can be highly active and can attack RBCs and bind components of the complement system to cause massive hemolysis of the transfused blood.
Patients should ideally receive their own blood or type-specific blood products to minimize the chance of a transfusion reaction. Risks can be further reduced by cross-matching blood, but this may be skipped when blood is required for an emergency. Cross-matching involves mixing a sample of the recipient's blood with a sample of the donor's blood and checking to see if the mixture agglutinates, or forms clumps. If agglutination is not obvious by direct vision, blood bank technicians usually check for agglutination with a microscope. If agglutination occurs, that particular donor's blood cannot be transfused to that particular recipient. In a blood bank it is vital that all blood specimens are correctly identified, so labeling has been standardized using a barcode system known as ISBT 128.
The blood group may be included on identification tags or on tattoos worn by military personnel, in case they should need an emergency blood transfusion. Frontline German Waffen-SS had such tattoos during World War II. Ironically, this was an easy form of SS identification.[25]
Rare blood types can cause supply problems for blood banks and hospitals. For example Duffy-negative blood occurs much more frequently in people of African origin,[26] and the rarity of this blood type in the rest of the population can result in a shortage of Duffy-negative blood for patients of African ethnicity. Similarly for RhD negative people, there is a risk associated with travelling to parts of the world where supplies of RhD negative blood are rare, particularly East Asia, where blood services may endeavor to encourage Westerners to donate blood.[27]
Hemolytic disease of the newborn (HDN)
A pregnant woman can make IgG blood group antibodies if her fetus has a blood group antigen that she does not have. This can happen if some of the fetus' blood cells pass into the mother's blood circulation (e.g. a small fetomaternal hemorrhage at the time of childbirth or obstetric intervention), or sometimes after a therapeutic blood transfusion. This can cause Rh disease or other forms of hemolytic disease of the newborn (HDN) in the current pregnancy and/or subsequent pregnancies. If a pregnant woman is known to have anti-RhD antibodies, the RhD blood type of a fetus can be tested by analysis of fetal DNA in maternal plasma to assess the risk to the fetus of Rh disease.[28] Antibodies associated with some blood groups can cause severe HDN, others can only cause mild HDN and others are not known to cause HDN.
Compatibility
Blood products
In order to provide maximum benefit from each blood donation and to extend shelf-life, blood banks fractionate some whole blood into several products. The most common of these products are packed RBCs, plasma, platelets, cryoprecipitate, and fresh frozen plasma (FFP). FFP is quick-frozen to retain the labile clotting factors V and VIII, which are usually administered to patients who have a potentially fatal clotting problem caused by a condition such as advanced liver disease, overdose of anticoagulant, or disseminated intravascular coagulation (DIC).
Units of packed red cells are made by removing as much of the plasma as possible from whole blood units.
Clotting factors synthesized by modern recombinant methods are now in routine clinical use for hemophilia, as the risks of infection transmission that occur with pooled blood products are avoided.
Red blood cell compatibility
- Blood group AB individuals have both A and B antigens on the surface of their RBCs, and their blood serum does not contain any antibodies against either A or B antigen. Therefore, an individual with type AB blood can receive blood from any group (with AB being preferable), but can donate blood only to another group AB individual.
- Blood group A individuals have the A antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the B antigen. Therefore, a group A individual can receive blood only from individuals of groups A or O (with A being preferable), and can donate blood to individuals of groups A or AB.
- Blood group B individuals have the B antigen on the surface of their RBCs, and blood serum containing IgM antibodies against the A antigen. Therefore, a group B individual can receive blood only from individuals of groups B or O (with B being preferable), and can donate blood to individuals of groups B or AB.
- Blood group O (or blood group zero in some countries) individuals do not have either A or B antigens on the surface of their RBCs, but their blood serum contains IgM anti-A antibodies and anti-B antibodies against the A and B blood group antigens. Therefore, a group O individual can receive blood only from a group O individual, but can donate blood to individuals of any ABO blood group (ie A, B, O or AB). If anyone needs a blood transfusion in a dire emergency, and if the time taken to process the recipient's blood would cause a detrimental delay, O Negative blood can be issued.
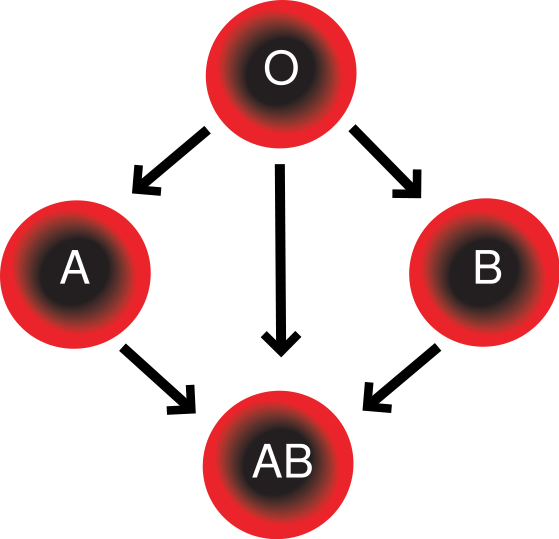
In addition to donating to the same blood group; type O blood donors can give to A, B and AB; blood donors of types A and B can give to AB.
| Recipient[1] | Donor[1] | |||||||
|---|---|---|---|---|---|---|---|---|
| O- | O+ | A- | A+ | B- | B+ | AB- | AB+ | |
| O- | Template:Check mark | |||||||
| O+ | Template:Check mark | Template:Check mark | ||||||
| A- | Template:Check mark | Template:Check mark | ||||||
| A+ | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | ||||
| B- | Template:Check mark | Template:Check mark | ||||||
| B+ | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | ||||
| AB- | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | ||||
| AB+ | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark |
Table note
1. Assumes absence of atypical antibodies that would cause an incompatibility between donor and recipient blood, as is usual for blood selected by cross matching.
A RhD negative patient who does not have any anti-RhD antibodies (never being previously sensitized to RhD positive RBCs) can receive a transfusion of RhD positive blood once, but this would cause sensitization to the RhD antigen, and a female patient would become at risk for hemolytic disease of the newborn. If a RhD negative patient has developed anti-RhD antibodies, a subsequent exposure to RhD positive blood would lead to a potentially dangerous transfusion reaction. RhD positive blood should never be given to RhD negative women of childbearing age or to patients with RhD antibodies, so blood banks must conserve Rhesus negative blood for these patients. In extreme circumstances, such as for a major bleed when stocks of RhD negative blood units are very low at the blood bank, RhD positive blood might be given to RhD negative females above child-bearing age or to Rh negative males, providing that they did not have anti-RhD antibodies, to conserve RhD negative blood stock in the blood bank.
The converse is not true; RhD positive patients do not react to RhD negative blood.
Plasma compatibility
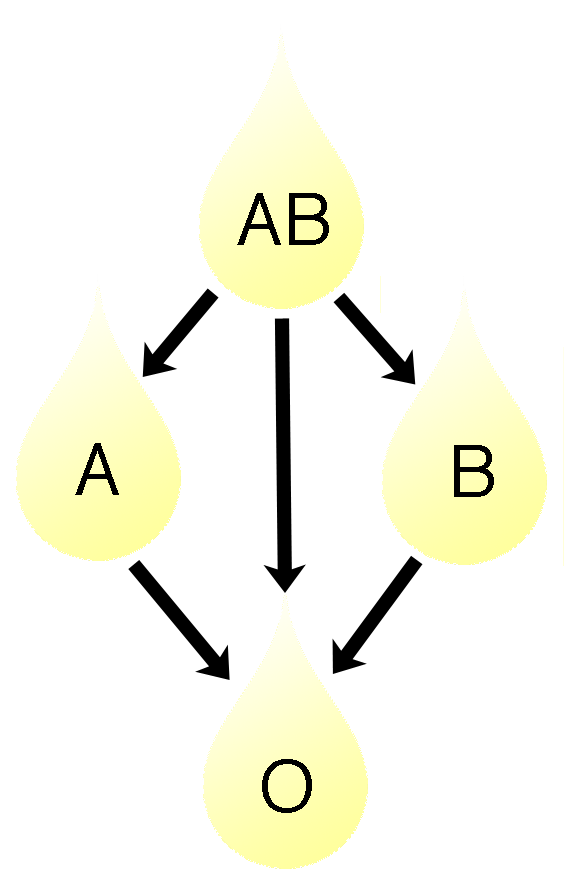
In addition to donating to the same blood group; plasma from type AB can be given to A, B and O; plasma from types A and B can be given to O.
Donor-recipient compatibility for blood plasma is the converse of that of RBCs. Plasma extracted from type AB blood can be transfused to individuals of any blood group, but type O plasma can be used only by type O recipients.
| Recipient | Donor[1] | |||
|---|---|---|---|---|
| O | A | B | AB | |
| AB | Template:Check mark | |||
| A | Template:Check mark | Template:Check mark | ||
| B | Template:Check mark | Template:Check mark | ||
| O | Template:Check mark | Template:Check mark | Template:Check mark | Template:Check mark |
Table note
1. Assumes absence of strong atypical antibodies in donor plasma
Rhesus D antibodies are uncommon, so generally neither RhD negative nor RhD positive blood contain anti-RhD antibodies. If a potential donor is found to have anti-RhD antibodies or any strong atypical blood group antibody by antibody screening in the blood bank, they would not be accepted as a donor (or in some blood banks the blood would be drawn the product would be appropriately labeled); therefore, donor blood plasma issued by a blood bank can be selected to be free of RhD antibodies and free of other atypical antibodies, and such donor plasma issued from a blood bank would be suitable for a recipient who may be RhD positive or RhD negative, as long as blood plasma and the recipient are ABO compatible.
Universal donors and universal recipients
With regard to transfusions of whole blood or packed red blood cells, individuals with type O negative blood are often called universal donors, and those with type AB positive blood are called universal recipients (Strictly speaking this is not true and individuals with Bombay blood group or Hh antigen system are the universal donors). Although blood donors with particularly strong anti-A, anti-B or any atypical blood group antibody are excluded from blood donation, the terms universal donor and universal recipient are an over-simplification, because they only consider possible reactions of the recipient's anti-A and anti-B antibodies to transfused red blood cells, and also possible sensitisation to RhD antigens. The possible reactions of anti-A and anti-B antibodies present in the transfused blood to the recipients RBCs are not considered, because a relatively small volume of plasma containing antibodies is transfused.
By way of example; considering the transfusion of O RhD negative blood (universal donor blood) into a recipient of blood group A RhD positive, an immune reaction between the recipient's anti-B antibodies and the transfused RBCs is not anticipated. However, the relatively small amount of plasma in the transfused blood contains anti-A antibodies, which could react with the A antigens on the surface of the recipients RBCs, but a significant reaction is unlikely because of the dilution factors. Rhesus D sensitisization is not anticipated.
Additionally, red blood cell surface antigens other than A, B and Rh D, might cause adverse reactions and sensitization, if they can bind to the corresponding antibodies to generate an immune response. Transfusions are further complicated because platelets and white blood cells (WBCs) have their own systems of surface antigens, and sensitization to platelet or WBC antigens can occur as a result of transfusion.
With regard to transfusions of plasma, this situation is reversed. Type O plasma can be given only to O recipients, while AB plasma (which does not contain anti-A or anti-B antibodies) can be given to patients of any ABO blood group.
Conversion
In April 2007, a method was discovered to convert blood types A, B, and AB to O, using enzymes. This method is still experimental and the resulting blood has yet to undergo human trials.[31][32] The method specifically removes or converts antigens on the red blood cells, so other antigens and antibodies would remain. This does not help plasma compatibility, but that is a lesser concern since plasma has much more limited clinical utility in transfusion and is much easier to preserve.
Popular use
The Japanese blood type theory of personality is a popular belief that a person's ABO blood type is predictive of their personality, character, and compatibility with others, according to books by Masahiko Nomi. This belief has carried over to a certain extent in other parts of East Asia such as South Korea and Taiwan. In Japan, asking someone their blood type is considered as normal as asking their astrological sign. It is also common for Japanese-made video games (especially role-playing games) and manga series to include blood type with character descriptions. This belief is completely dismissed by scientists.
The blood type diet is an American system whereby people seek improved health by modifying their food intake and lifestyle according to their ABO blood group and secretor status.[33] This system includes some reference to differences in personality, but not to the extent of the Japanese theory.
References
- ↑ Allen FH Jr, Krabbe SM, Corcoran PA. A new phenotype (McLeod) in the Kell blood-group system. Vox Sang. 1961 Sep;6:555-60. PMID 13477267
- ↑ Miller LH, Mason SJ, Clyde DF, McGinniss MH. "The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy." N Engl J Med. 1976 Aug 5;295(6):302-4 PMID 778616
- ↑ Kwiatkowski, DP (2005). "How Malaria Has Affected the Human Genome and What Human Genetics Can Teach Us about Malaria". Am J Hum Genet. 77 (2): 171–192. PMC 1224522. Retrieved 2006-11-16. Unknown parameter
|month=ignored (help)"The different geographic distributions of α thalassemia, G6PD deficiency, ovalocytosis, and the Duffy-negative blood group are further examples of the general principle that different populations have evolved different genetic variants to protect against malaria". - ↑ Landsteiner K. Zur Kenntnis der antifermentativen, lytischen und agglutinierenden Wirkungen des Blutserums und der Lymphe. Zentralblatt Bakteriologie 1900;27:357-62.
- ↑ Landsteiner K, Wiener AS. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc Soc Exp Biol Med 1940;43:223-224.
- ↑ Coombs RRA, Mourant AE, Race RR. A new test for the detection of weak and "incomplete" Rh agglutinins. Brit J Exp Path 1945;26:255-66.
- ↑ 7.0 7.1 "Table of blood group systems". International Society of Blood Transfusion. 2006. Retrieved 2006-11-14. Unknown parameter
|month=ignored (help) - ↑ "American Red Cross Blood Services, New England Region, Maine, Massachusetts, New Hampshire, Vermont". American Red Cross Blood Services - New England Region. 2001. Retrieved 2006-11-14.
there are more than 600 known antigens besides A and B that characterize the proteins found on a person's red cells
- ↑ Dean, Laura. "The ABO blood group". Blood Groups and Red Cell Antigens. online: NCBI.
A number of illnesses may alter a person's ABO phenotype
Stayboldt C, Rearden A, Lane T. "B antigen acquired by normal A1 red cells exposed to a patient's serum". Transfusion. 27 (1): 41–4. PMID 3810822. Matsushita S, Imamura T, Mizuta T, Hanada M (1983). "Acquired B antigen and polyagglutination in a patient with gastric cancer". Jpn J Surg. 13 (6): 540–2. PMID 6672386. Kremer Hovinga I, Koopmans M, de Heer E, Bruijn J, Bajema I (2007). "Change in blood group in systemic lupus erythematosus". Lancet. 369 (9557): 186–7, author reply 187. doi:10.1016/S0140-6736(07)60099-3. PMID 17240276. - ↑ "Your blood – a textbook about blood and blood donation" (PDF). p. 63. Retrieved 2006-11-21.
- ↑ [1]
- ↑ Austrian Red Cross - Blood Donor Information
- ↑ Blood Types - What Are They?, Australian Red Cross
- ↑ Types & Rh System, Canadian Blood Services
- ↑ Frequency of major blood groups in the Danish population.
- ↑ Suomalaisten veriryhmäjakauma
- ↑ "Les groupes sanguins (système ABO)". Centre Hospitalier Princesse GRACE - Monaco (in French). C.H.P.G. MONACO. 2005. Retrieved 2006-12-27.
- ↑ Blood Donation, Hong Kong Red Cross
- ↑ Statistics on annual blood donations 2002-2005, Gyung Nam Blood Center
- ↑ Blood bank Sanquin - Blood Donor information material
- ↑ Regionalne Centrum Krwiodawstwa i Krwiolecznictwa we Wrocławiu
- ↑ Frequency of major blood groups in the Swedish population.
- ↑ Frequency of major blood groups in the UK.
- ↑ Census CounterParts.
- ↑ "German Intelligence Agents and Suspected Agents". Highlights of Freedom of Information releases in September 2005. The National Archives. 2005. Retrieved 2006-11-20.
... the trademark SS tattoo under his arm of his blood group
Unknown parameter|month=ignored (help) - ↑
Nickel, RG (1999 Aug). "Determination of Duffy genotypes in three populations of African descent using PCR and sequence-specific oligonucleotides". Hum Immunol. 60 (8): 738–42. doi:10.1016/S0198-8859(99)00039-7. PMID 10439320. Unknown parameter
|coauthors=ignored (help); Check date values in:|date=(help) - ↑ Bruce, MG (2002). "BCF - Members - Chairman's Annual Report". The Blood Care Foundation. Retrieved 2006-11-16.
As Rhesus Negative blood is rare amongst local nationals, this Agreement will be of particular value to Rhesus Negative expatriates and travellers
Unknown parameter|month=ignored (help) - ↑ Daniels G, Finning K, Martin P, Summers J. "Fetal blood group genotyping: present and future". Ann N Y Acad Sci. 1075: 88–95. doi:10.1196/annals.1368.011. PMID 17108196.
- ↑ "RBC compatibility table". American National Red Cross. 2006. Retrieved 2006-12-24. Unknown parameter
|month=ignored (help) - ↑ Blood types and compatibility bloodbook.com
- ↑
"Blood groups 'can be converted'". BBC News. 2007. Retrieved 2007-10-10. Unknown parameter
|month=ignored (help) - ↑ Liu Q, Sulzenbacher G, Yuan H, Bennett E, Pietz G, Saunders K, Spence J, Nudelman E, Levery S, White T, Neveu J, Lane W, Bourne Y, Olsson M, Henrissat B, Clausen H. "Bacterial glycosidases for the production of universal red blood cells". Nat Biotechnol. doi:10.1038/nbt1298. PMID 17401360.
- ↑
D'Adamo, Dr. Peter J (1996). Eat Right 4 Your Type: The Individualized Diet Solution to Staying Healthy, Living Longer and Achieving Your Ideal Weight. New York: Penguin Group (USA). ISBN 0-399-14255-X. Unknown parameter
|coauthors=ignored (help)
Further reading
- Dean, Laura. "Blood Groups and Red Cell Antigens, a guide to the differences in our blood types that complicate blood transfusions and pregnancy" (HTML, also PDF, Flash and PRC versions). NCBI. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - Mollison PL, Engelfriet CP and Contreras M. "Blood Transfusion in Clinical Medicine." 1997. 10th edition. Blackwell Science, Oxford, UK. ISBN 0-86542-881-6
External links
- BGMUT Blood Group Antigen Gene Mutation Database at NCBI, NIH has details of genes and proteins, and variations thereof, that are responsible for blood types
- Online Mendelian Inheritance in Man (OMIM) 110300 (ABO)
- Online Mendelian Inheritance in Man (OMIM) 111680 (Rhesus D)
- D'Adamo, Peter (2006). "Eat Right 4 Your Type". Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - Farr, A D (1979). "Blood group serology—the first four decades (1900--1939)". Med Hist. 23 (2): 215–226. PMC 1082436. Unknown parameter
|accessmonthday=ignored (help); Unknown parameter|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|month=ignored (help) - "Blood group test, Gentest.ch" (HTML, JavaScript). Gentest.ch GmbH. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help) - "Blood typing systems other than ABO". BloodBook.com. 2005-09-10. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - "Blood Facts". LifeShare Blood Centers. Text " Rare Traits " ignored (help); Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - "Modern Human Variation: Distribution of Blood Types" (HTML). Dr. Dennis O'Neil, Behavioral Sciences Department, Palomar College, San Marcos, California. 2001-06-06. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help);|archive-url=is malformed: timestamp (help) - "Racial and Ethnic Distribution of ABO Blood Types - BloodBook.com, Blood Information for Life". bloodbook.com. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help)
ar:فئات الدم bg:Кръвна група ca:Grup sanguini cs:Krevní skupina da:Blodtype de:Blutgruppe gl:Grupo sanguíneo ko:혈액형 id:Golongan darah it:Gruppo sanguigno he:סוג דם lt:Kraujo grupė hu:Vércsoport nl:Bloedgroep nn:Blodtype uz:Qon guruhlari simple:Blood type sl:Krvna skupina su:Golongan getih fi:Veriryhmä sv:Blodgrupper th:หมู่โลหิต