Acute mesenteric ischemia pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby
|
Acute mesenteric ischemia Microchapters |
|
Differentiating Acute mesenteric ischemia from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Acute mesenteric ischemia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Acute mesenteric ischemia pathophysiology |
|
Risk calculators and risk factors for Acute mesenteric ischemia pathophysiology |
Overview
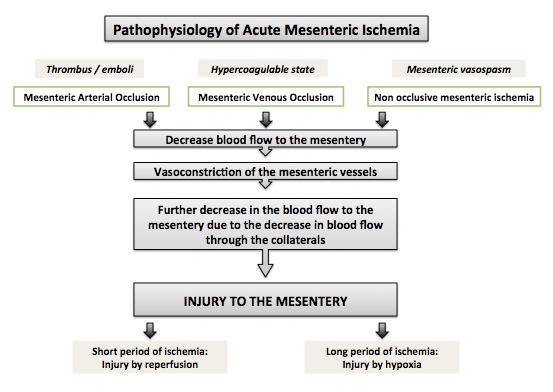
Acute mesenteric ischemia is caused by a sudden decrease in the blood flow to the small bowels leading to reperfusion and hypoxic injuries. The main protective mechanism, which is the supply of blood by collateral vessels, becomes no longer effective as the mesenteric vasculature constricts in response to ischemia. Hypoperfusion is caused either by occlusive or non occlusive causes.
Pathophysiology
- The main mechanism underlying mesenteric ischemia is decreased blood flow to the small intestine. The decrease in blood flow can be caused by:
- Occlusion
- Systemic hypoperfusion
- Spasm in the mesentery
- When blood flow to the mesentery decreases, collateral vessels try to compensate. However, following prolonged decrease in blood flow, vasoconstriction of the mesenteric vessels occurs leading to decreased blood flow in the collaterals, which were initially the main protective mechanism against ischemia.[1]
- It is worth mentioning that mesenteric vessel vasoconstriction can persist after the blood flow is restored which explains the use of vasodilator in the management of acute mesenteric ischemia.[1]
- Ischemia associated injury to the mesentery is either reperfusion injury when the ischemia occurs for a brief period of time or hypoxic injury when the ischemia occurs for a prolonged time.[1][2]
- Shown below is a diagram depicting the pathophysiology of acute mesenteric ischemia.
Mesenteric Arterial Occlusion
- Decreased blood flow in arterial occlusion occurs when the vessel, mainly superior mesenteric artery, is blocked by an embolism that has originated from the left heart or from a thrombus that has formed secondary to atherosclerosis, trauma or infection.[1][3]
- Strangulation of the small bowels might also lead to occlusion of the mesenteric arteries and subsequent ischemia.
Mesenteric Venous Occlusion
- Decreased blood flow to the mesentery in venous occlusion occurs with a sequence of events different from that of arterial occlusion. In hypercoagulable states, whether inherited or acquired, a blood clot is formed in the venous mesenteric vasculature. When the venous blood clot is formed, the resistance in the venous blood flow of the mesentery increases with subsequent increase in the fluid movement across the blood vessels. The result is bowel edema and systemic hypotension that leads to systemic hypoperfusion to the different organs, including the mesentery.[4]
Non Occlusive Mesenteric Ischemia
- Non occlusive mesenteric ischemia occurs when the blood flow to the mesentery decreases secondary to systemic hypoperfusion complicated by secondary mesenteric vasospasm. Non occlusive acute mesenteric ischemia occurs mainly in elderly with multiple cardiovascular risks and cardiovascular comorbidities in the setting of hypotension secondary to medication use, sepsis, myocardial infarction, congestive heart failre, kidney or liver failure. When hypotension occurs, the blood flow to the mesentery decreases and then it is complicated by further constriction of the mesenteric vasculature.[5]
- Cocaine can be a cause of non occlusive acute mesenteric ischemia.[6]
References
- ↑ 1.0 1.1 1.2 1.3 Reinus JF, Brandt LJ, Boley SJ (1990). "Ischemic diseases of the bowel". Gastroenterol Clin North Am. 19 (2): 319–43. PMID 2194948.
- ↑ Lapchak PH, Kannan L, Ioannou A, Rani P, Karian P, Dalle Lucca JJ; et al. (2012). "Platelets orchestrate remote tissue damage after mesenteric ischemia-reperfusion". Am J Physiol Gastrointest Liver Physiol. 302 (8): G888–97. doi:10.1152/ajpgi.00499.2011. PMID 22301111.
- ↑ Rosenblum JD, Boyle CM, Schwartz LB (1997). "The mesenteric circulation. Anatomy and physiology". Surg Clin North Am. 77 (2): 289–306. PMID 9146713.
- ↑ Haglund U. Mesenteric ischemia. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001. Available from: http://www.ncbi.nlm.nih.gov/books/NBK6883/
- ↑ Trompeter M, Brazda T, Remy CT, Vestring T, Reimer P (2002). "Non-occlusive mesenteric ischemia: etiology, diagnosis, and interventional therapy". Eur Radiol. 12 (5): 1179–87. doi:10.1007/s00330-001-1220-2. PMID 11976865.
- ↑ Sudhakar CB, Al-Hakeem M, MacArthur JD, Sumpio BE (1997). "Mesenteric ischemia secondary to cocaine abuse: case reports and literature review". Am J Gastroenterol. 92 (6): 1053–4. PMID 9177533.